In 2019, drug manufacturer Genzyme was thought to have lost up to $300m in revenue due to plant shutdown after product contamination. Ensuring appropriate aseptic practices are followed can mean the difference between efficient manufacturing operations and the shutting down of a plant. The devastating impact of cross-contamination has seen the industry develop technology and appropriate practices to reduce the risk of manufacturing failures.
Aseptic processing is defined as the “handling of sterile product, containers, and/or devices in a controlled environment, in which the air supply, materials, equipment, and personnel are regulated to maintain sterility”. This is a critical step in pharmaceutical manufacturing, which, if performed incorrectly or poorly, could adversely affect the quality of the drug through contamination.
The production of sterile drug products is dependent on aseptic processing or terminal sterilisation. Aseptic processing subjects the drug product and container to sterilisation separately before bringing them together in the final stages. Terminal sterilisation, on the other hand, involves filling and sealing product containers under high-quality environmental conditions to minimise the microbial and particulate content of the in-process product. After this stage, the product in its final container undergoes heat or irradiation for the final sterilisation process.
Aseptic processing and terminal sterilisation require validation and control to prevent avoidable errors. Should an error occur in either of these processes, it could lead to the distribution of a contaminated product, later posing a significant risk for patients.
In addition to hazardous safety implications, drug product contamination can have a substantial impact on manufacturers. According to a pharmaceutical news article, drug manufacturer Genzyme was forced to close its Massachusetts plant in 2009 after a virus was found to have contaminated a bioreactor. In terms of patient impact, the contamination halted production of two drugs, Fabrazyme and Cerezyme, that were at the time used by 8,000 patients globally.
From a pharmaceutical perspective, the halt in production was a financial blow for the manufacturer. In addition to a fine of $175m by the FDA, more than $28.4m worth of drug product was written off.
More recently in 2020, an article reported that the FDA announced that a number of drugs have been contaminated with a potential human carcinogen, NMDA. Metformin, a popular diabetes drug, is an example of a drug implicated in this incident. In said article, there were a number of potential causes for the incident including the useage of contaminated water, lack of pH or temperature control and pre-existing contamination of raw materials.
This resulted in the presence of NMDA in drugs above the acceptable daily intake (ADI) limit. The number of potential causes for contamination questions the quality control of the aseptic processes and sterile preparation by the manufacturers. This emphasises the need to develop more stringent aseptic and sterilisation protocols to prevent such errors occurring again.
Aseptic practices in drug manufacturing
The following are a few examples of conventional and more recent innovations in aspects of aseptic processing.
Training of personnel
Personnel across the manufacturing system are potential sources for contamination and “a vector for other contaminants”. Lack of appropriate training with aseptic practices, unauthorised access into controlled areas and personal cleanliness are a few of the areas in which personnel can compromise sterile production.
The industry is now focusing on thorough training and documented communication of procedures and best practices. This is vital to optimise facility operations as well as minimising contamination. The WHO good manufacturing practices is an example of such a document aimed to guide manufactures in the production of sterile pharmaceutical drugs.
Quality control and sanitation are 2 of 13 steps detailed throughout the steps for aseptic practices. During quality control, it is emphasised that while samples for sterility testing should be representative of the whole batch, some samples taken from parts of the batch are considered to be most at risk of contamination. In the case of injectable products, the water for the injection, the intermediate and the final product should be monitored for endotoxins.
Endotoxins are a major challenge for sterilisation. These are toxic substances “bound to the bacterial cell wall and released when the bacterium ruptures or disintegrates”.
Rapid Transfer Port
The Rapid Transfer Port (RTP) allows for transfer of hazardous or sterile materials while maintaining containment of sealed barriers. In order to address the risk of accidental manipulation during the transfer, a number of safety devices are in place.
RTPs are typically installed on isolators or production lines to enable the sterile transfer between two chambers without environmental exposure. This means that ‘clean’ material can be transported from “one sterile zone to another through a non-sterile zone, using the DPTE container or single use bag which can be reconnected without risk because the inside of the container is still sterile.”
According to an industry article, the risk of human error occurring during material transfer is “proportional to the number of manual operations required, of which RTPs generally entails a series of manual interventions”. So while the machinery and mechanisms work well to prevalent environmental exposure between transfer, and devices to reduce the chance of errors, humans are still required to operate them at every stage. This is an issue that needs to be addressed, potentially with the development of more automated systems in aseptic processing.
The popularity of the RTP system in the pharmaceutical industry is evident, with more than 40,000 Alpha units sold to global locations. Successful, validated systems like RTPs are a prime example of the evolution in developing more stringent aseptic practices.
Single-use technology
Single-use technology is rapidly emerging in aseptic practices across the pharmaceutical industry, with the potential to reduce cross-contamination risk. This type of equipment can reduce costs by eliminating the need for in-house sterilisation. Although the initial cost of single-use equipment may be high, the benefits of a faster turnaround allows production to move faster and continuously.
Examples of single-use equipment include chromatography devices, bioreactors and ion exchange membranes.
One of the main benefits for single use equipment is sterility assurance during the manufacturing process. This is achieved by a reduction in the “possibility of cross-transference of microorganisms; minimising the risk of environmental microbial contamination”. The risk of cross-contamination especially is greatly reduced with the avoidance of cleaning components, thanks to single use equipment.
Due to the infancy of this technology, it is important to assess the possibility of leachables that could arise and pose a concern for quality control. This is echoed in an article which highlights the limited availability of the technology and potential development costs.
Charlotte Di Salvo, Lead Medical Writer
PharmaFeatures
Subscribe
to get our
LATEST NEWS
Related Posts

Manufacturing & Logistics
Enhancing Resilience in Pharmaceutical Supply Chains: A Comprehensive Approach
In the realm of healthcare, particularly within the pharmaceutical supply chain, resilience is of paramount importance.

Manufacturing & Logistics
Amerigo Scientific’s Lab Sample Storage Breakthrough: A -86°C Freezer
Amerigo Scientific’s latest innovative product represents a significant advancement in temperature-controlled storage technology.
Read More Articles
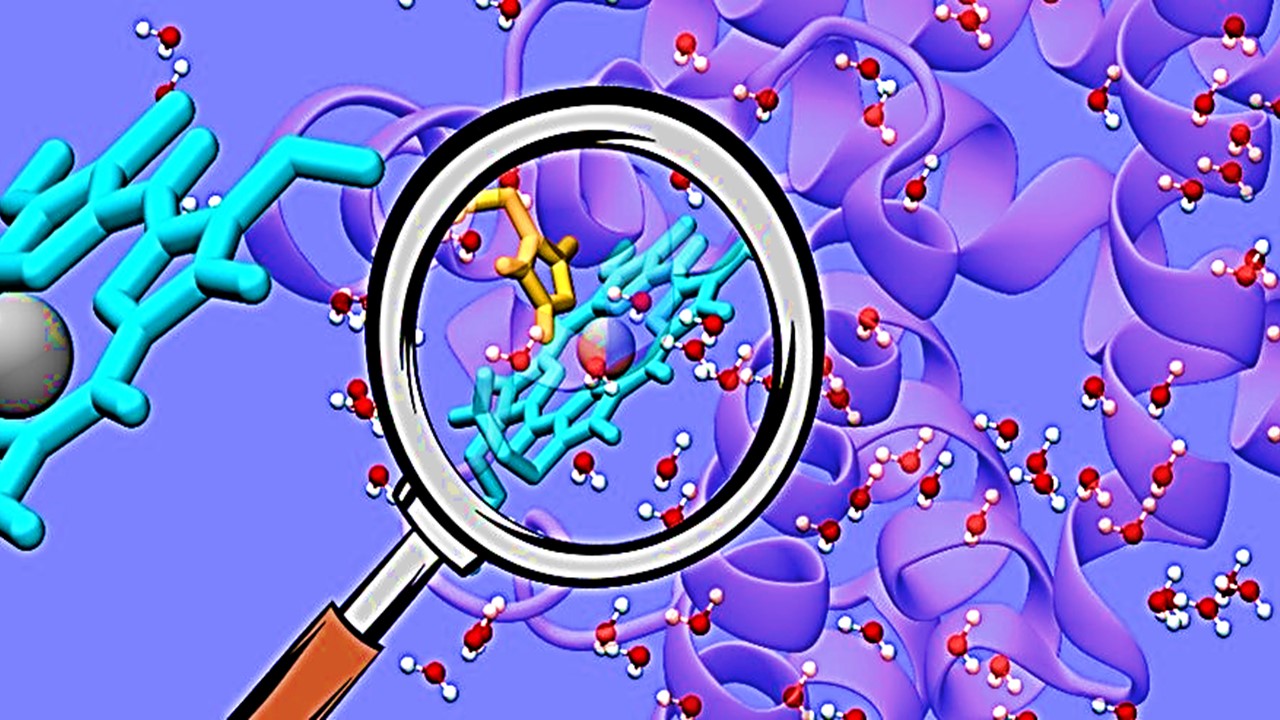
Synthetic Chemistry’s Potential in Deciphering Antimicrobial Peptides
The saga of antimicrobial peptides unfolds as a testament to scientific ingenuity and therapeutic resilience.