Patient and public involvement (PPI) has been an idea central to the improvement of clinical trials for decades. Adapting mindsets to frame clinical investigations as endeavors that are carried out “with”, rather than “for”, patients is a mission that must remain a priority for the sake of increased accountability and clinical success, as studies show. The increase in public involvement dovetails with the advent of decentralized clinical trials (DCT) and improved patient centricity: both can strengthen each other, and, through doing so, improve overall outcomes for trials.
What is PPI?
In the United Kingdom, the National Institute for Health Research expects PPI in research it funds – and has published guidelines for what that entails. Patients and public citizens are expected to be involved in setting the agenda, steering committees, ethics, protocol development, and other parts of the formal investigation process. PPI can have many shapes, whether through advocacy groups or individuals. The effects it can assume can be equally multifaceted: from transient, one-off, non-decision making involvement to constant and with supervisory privileges, or any variation thereof.
The moral argument for increased PPI is strong – many times, it is not merely patients benefiting from clinical trials, but also the ones funding them, whether directly or indirectly. But morals alone do not often justify rapid change. A review in the British Medical Journal shows that increased PPI can lead to significantly higher patient enrolment rates. Crucially, this boost in enrolment was greater when the involved members of the public had lived experiences of the area under investigation. Some studies also showed an increase in retention rates for trials employing PPI approaches.
For example, a review found that people with lived experiences of mental illnesses could improve diagnostic accuracy as well as reduce the stigma surrounding mental health when they are involved in trials and provide training to primary care practitioners. Exposure to recovery testimonials from such engaged members of the public showed that practitioners subsequently demonstrated lower levels of misdiagnosing diseases such as psychosis. This can prove crucial in mental health and other socially complex diseases, helping to tear down long-held prejudices.
PPI During a Pandemic
Much like other parts of the clinical development industry, Patient and Public Involvement bodies had a lot to adjust to during the onset of the COVID-19 pandemic. The non-pharmaceutical interventions and social distancing employed to limit the spread of the virus placed limits on how involvement could be done. Studies with described PPI measures in the UK had dropped off from their usual levels of ~80% to 20% in March-April 2020 . Yet the industry adjusted, and transformed the way PPI is done, resulting in PPI measures for 85% of COVID-19 studies by August 2020. This was handled by a National Healthcare Service (NHS) matching service, providing fast-tracked trials with support for the inclusion of PPI measures.
Researchers outline ways that technology can be harnessed to enable PPI during such times, which goes hand-in-hand with the increased uptake of smart technologies and applications for conducting clinical research in general. Technology can also present unique barriers – such as exacerbating potential digital divides, a need for increased flexibility and properly supporting PPI contributors. These considerations are crucial not only for PPI, but also in maintaining as diverse a pool of contributors and participants as possible: technology should tear down barriers, not raise them.
An article detailing the involvement of a PPI panel for a study at the London School of Hygiene and Tropical Medicine noted the importance of having access to participants with lived experiences in a study that seeks to adjust to a rapidly emerging threat. Additionally, they highlighted PPI is the best way to introduce new practices and technologies successfully while minimizing delays. This is particularly critical as we see novel technologies revolutionize how we conduct clinical research: many underscore the challenges and upfront investments required to make a switch to DCTs and virtual technologies, but few consider that the solution to smoother implementations may be an improved rapport with participants and the public.
Future Approaches
PPI acknowledges the importance and complexity of subjects in clinical practice – even the best of practitioners have to learn from the individuals in their subject area. This is particularly true in fields that have suffered from chronic stigmatization, or when complex change is required. Encouraging further patient centricity and decentralization is another promising avenue of transformation for the industry – but the public should also have a voice in bringing it about, for best results.
Join Proventa International’s Clinical Operations Strategy Meeting in Boston to hear more on the subject of public involvement in clinical practice – network with leading industry and academic stakeholders and grab the pulse of current trends
Subscribe
to get our
LATEST NEWS
Related Posts

AI, Data & Technology
The Power of Unsupervised Learning in Healthcare
In healthcare’s dynamic landscape, the pursuit of deeper insights and precision interventions is paramount, where unsupervised learning emerges as a potent tool for revealing hidden data structures.

Clinical Operations
Supervised Learning: Harnessing Data to Revolutionize Patient Care
As healthcare enters a new era, the integration of ML promises to revolutionize oncology and medicine.
Read More Articles
Synthetic Chemistry’s Potential in Deciphering Antimicrobial Peptides
The saga of antimicrobial peptides unfolds as a testament to scientific ingenuity and therapeutic resilience.
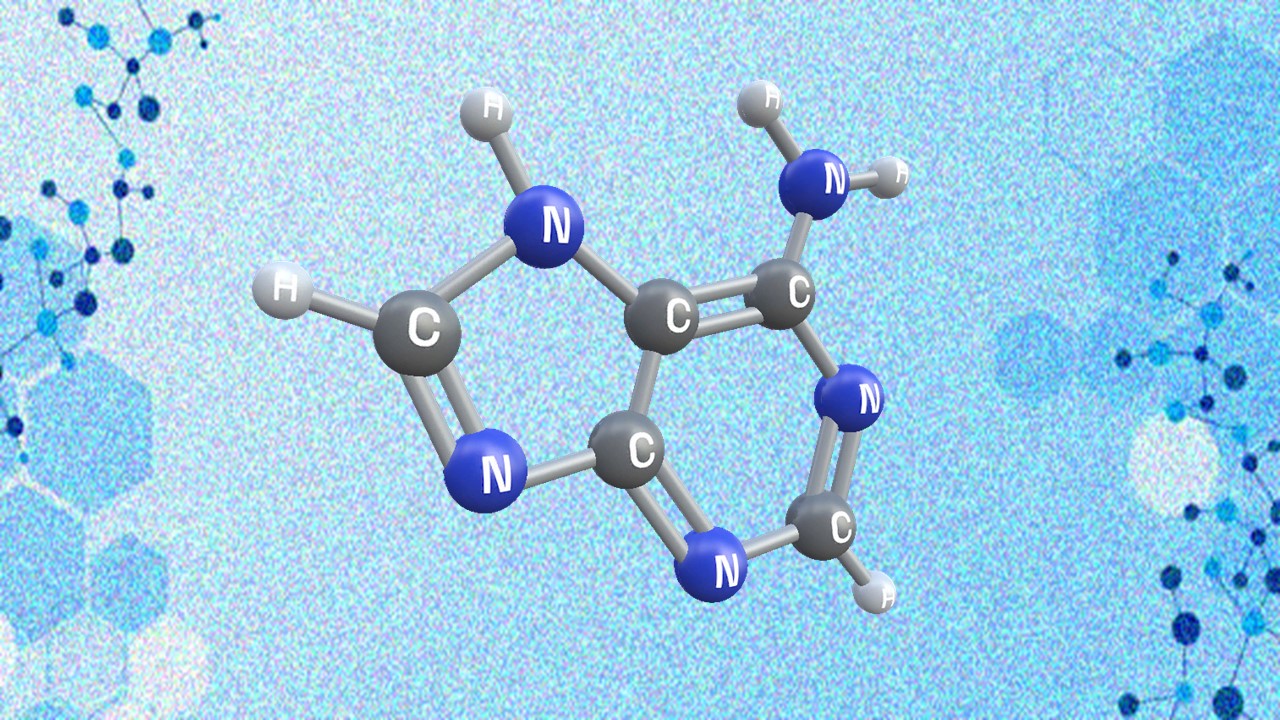
Appreciating the Therapeutic Versatility of the Adenine Scaffold: From Biological Signaling to Disease Treatment
Researchers are utilizing adenine analogs to create potent inhibitors and agonists, targeting vital cellular pathways from cancer to infectious diseases.