Many public and private organizations have demanded the creation of a publicly accessible, thorough, and transparent register of pertinent data on clinical trials for pharmaceuticals and biologics in an effort to increase public trust in clinical research. A public clinical trial registry is subject to varying expectations and perceived needs from members of the general public and different groups within the medical community (such as physicians, researchers, editors of medical journals, pharmaceutical corporations, health insurers, and regulators).
Springboarding the Registry Initiative
The Institute of Medicine (IOM) Board on Health Sciences Policy invited editors of medical journals, executives from the pharmaceutical and biotech industries, and representatives from the National Institutes of Health (NIH) and Food and Drug Administration (FDA) to a meeting in December 2004 to talk about the requirements for clinical trial registration that the International Committee of Medical Journal Editors (ICMJE) had published. Then after the meeting, the IOM set up a panel whose members continued their discussions with editors of medical journals and top executives from the pharmaceutical and biotech industries about potential elements and implementation strategies for a clinical trial registry which would satisfy the public’s demand for disclosure while encouraging innovation in the creation of new therapeutic strategies.
Central Registry Content Imperatives
Based on those discussions, the suggested goals for the central registry are as follows. Health care providers and their patients are expected to be provided reliable and apt information regarding clinical trials. In addition, the same stakeholders must be made cognizant of the results of the clinical trial once completed, especially when the drug product at study is available for commercial use. To prevent biased or selective report reporting, it is imperative to link every clinical trial with a reported outcome. Finally, the aforementioned trio of desired outcomes must be met while ensuring proprietary research data protection and innovation preservation.
Procedures to Proceed With
Succeeding the discussions of the committee is the identification of the cornerstone events that would serve as the edifice for fully establishing the aforementioned goal’s optimized implementation. Data disclosure, both at trial commencement and completion, and whether publicly or privately funded, must conform to uniformity of standards. An imperative balance is owed to the stakeholders with regards to both the maximized democratization of clinical trial information while maintaining confidentiality and proprietary research data protectivity measures. As with any other implementation of edicts or regulations, non-compliance must be duly dealt with mechanisms of fair sanctioning all while guaranteeing well-ruminated aspects as to how to effect full compliance. Ultimately, the National Library of Medicine (NLM) is identified, among other trusted government functional units or not-for-profit institutions, to hold major responsibilities for the development, management, and maintenance of the registry.
Undeniable Peremptoriness of the Clinical Registry
Clinical trial registries may serve four purposes. Clinical trial registries keep tabs on the progress of these studies. They offer data to help with patient recruitment. To help with conducting systematic reviews of the evidence, they offer an exhaustive database of all trials. Moreover, clinical trial registries disseminate study results.
Expanse of Stakeholders
Patients, healthcare professionals, researchers, editors of medical journals, pharmaceutical firms, health insurers, and regulators are just a few of the audiences for this information. Although the needs of these audiences for data and translation of the registry’s material vary, none of these needs can be fully satisfied by other sources.
The File Drawer Effect
Clinical trial data that are selectively published do not give a complete picture. There is an understandable predisposition toward the sharing of positive outcomes, known as the “file drawer phenomenon,” both intentionally and unintentionally. The pharmaceutical industry lacks a persuasive argument for why clinical trial findings that do not support the introduction of new drugs should be published. Positive outcomes are typically more eagerly published by researchers and journal editors than negative results. Peer-reviewed publications are substantially less popular when the findings are inconclusive. The findings are more likely to be reported if there are statistically significant differences for both safety and effectiveness data.
The Need for the Whole Picture
In most cases, a body of evidence rather than a single study is needed to sway the opinions of medical policy experts, researchers, physicians, and patients. In fact, the regulatory evaluation and approval of pharmaceutical goods is based on this body of information. Making decisions responsibly needs knowledge of both favorable and unfavorable clinical trial outcomes, as well as assurance that the results are readily accessible.
Data, Decision-Making and Democratized Quality of Care
Correspondingly, major players in the medical community have proposed that if clinical trials were systematically registered at their beginning, accompanied by the submission of summary results for the study, and both were widely obtainable to interested parties, then the full spectrum of clinical evidence encompassing an investigative treatment would become a matter of public record. The registry additionally offers a comprehensive record after a drug has been authorized, which can be used as information by individuals who create guidelines, insurance companies, and those who keep an eye on the standard of care in the US.
Heterogeneity of Hopes and Appraised Necessities
Regarding a public clinical trial registry, the general public and various organizations within the medical profession have varied expectations and perceived needs.
Patients and Their Loved Ones
Patients with various conditions, as well as their loved ones, want to know that the right medicines are being provided and that patient safety is being ensured. Also, a growing number of patients today want the freedom to look for research on their own that relates to their condition and, if appropriate, to enroll in a clinical trial.
Healthcare Professionals
Health care providers want the ability to examine the clinical data from any individual research as well as objective summaries of all drug or therapy trials that have been conducted. They don’t want to limit their analysis to medical journal publications or labels for licensed drugs.
Scientists, Legal Officers and Insurance Companies
By gaining access to all the trials undertaken on a drug or therapy, researchers can come up with fresh research concepts or spot data trends. In order to create policies pertaining to clinical research, regulators would find the data in a register useful. As the foundation for their insurance coverage policies, health insurers want to stay current on research that is supported by evidence.
Study Sponsors
An expensive new therapy or medication is being developed by sponsors of research. For the organizations who fund the research, some of the data is highly sensitive and proprietary. Industry is worried that if all proprietary material were to be made widely available to the public at the start of clinical trials, they would not be able to repay their investment because rivals in the US or overseas would copy their discoveries. Also, they are aware of their duty to take all reasonable steps to maintain the public’s trust while still ensuring patient safety.
Scientific Publishers
Clinical practice and medical policy are significantly influenced by medical journals. Journal editors are concerned that they completely comprehend the study when they receive clinical trial manuscripts for publication. They want to determine whether there are any clinical studies that might clash with the manuscript that was submitted. Also, they want to know if the authors adhered to the initial research strategy because variations could indicate severe flaws in the study. In fact, when research is posted through the peer-review process, the credibility of the journal is at risk, as is the integrity of the whole research discipline.
Management, Maintenance and More
A national registry might be run by a reputable government body or a nonprofit group, according to various workshop attendees. A logical method to improve on current initiatives would be to expand the National Library of Medicine’s oversight of ClinicalTrials.gov to include more trials and information. It was also mentioned that the FDA holds some of the information that a clinical trial registry would require.
Maintaining public confidence in the validity of clinical research and the method by which research is converted into new pharmaceuticals and biologics is the overarching objective in achieving a balance between these conflicting interests regarding the scope of clinical trial registries.
Engr. Dex Marco Tiu Guibelondo, BS Pharm, RPh, BS CpE
Editor-in-Chief, PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts

Clinical Operations
Supervised Learning: Harnessing Data to Revolutionize Patient Care
As healthcare enters a new era, the integration of ML promises to revolutionize oncology and medicine.

Clinical Operations
The Interplay of Public and Private Sectors in Pharmaceutical Innovation
A delicate balance between public and private investments shapes the pharma R&D landscape.
Read More Articles
Synthetic Chemistry’s Potential in Deciphering Antimicrobial Peptides
The saga of antimicrobial peptides unfolds as a testament to scientific ingenuity and therapeutic resilience.
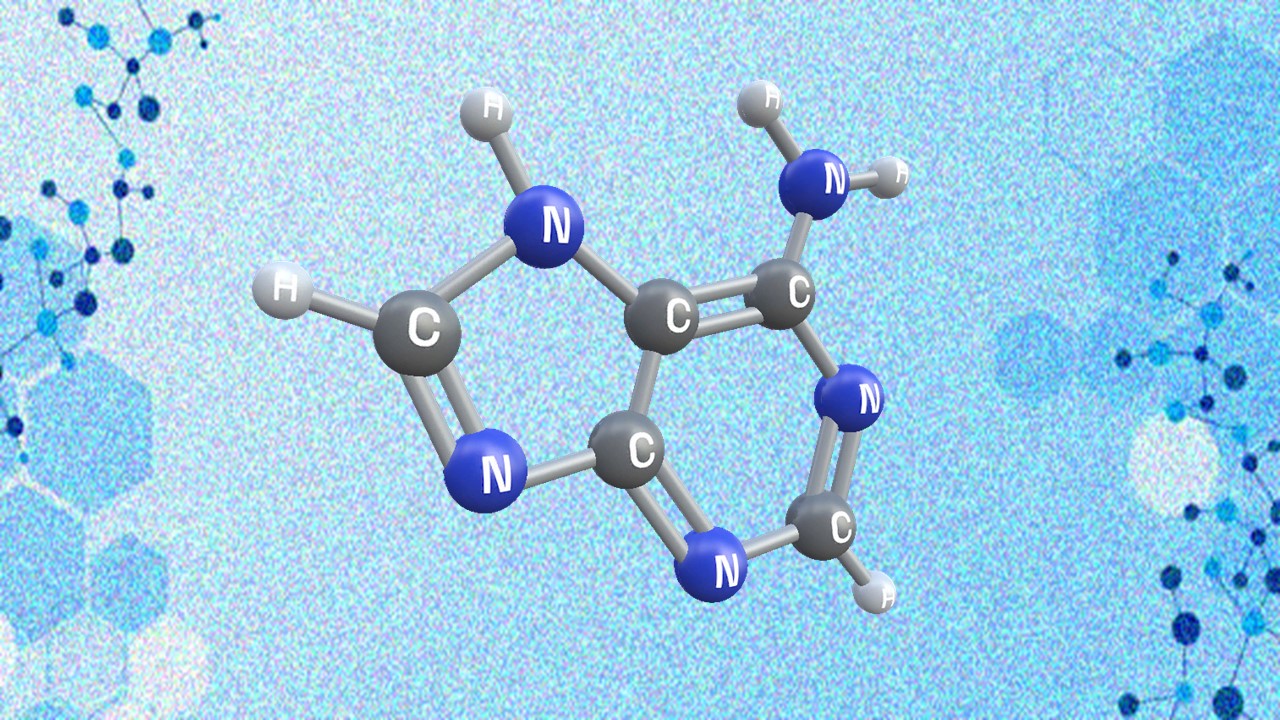
Appreciating the Therapeutic Versatility of the Adenine Scaffold: From Biological Signaling to Disease Treatment
Researchers are utilizing adenine analogs to create potent inhibitors and agonists, targeting vital cellular pathways from cancer to infectious diseases.