The following is an interview with Jessicca Rege, Vice President and Head of Oncology at Alkermes. Alkermes has been an innovator in the field of Immuno-oncology, utilising immune-based treatments in the fight against cancer. Jessicca Rege will be attending the Oncology Strategy Meeting organised by Proventa International at Le Meridien in Cambridge, Boston on the 17th of May. She will be speaking about the future of immuno-oncology and how to handle resistance to immune checkpoint inhibitor-based treatments.
Immune checkpoint inhibitors have revolutionised the field of immuno-oncology. However, to pave the way for wider adoption of the treatment, we must further understand why they do not work in many patients. The reasons for such treatment resistance are multi-faceted, and a more intimate understanding of the underlying mechanisms at play can help tailor future treatment strategies to be more effective.
PF: Immune Checkpoint Inhibitors are an antibody-based therapy which functions by stopping tumours from expressing proteins that protect them from the body’s immune system. Do you feel that research is too focused on Immune Checkpoint Inhibitors? Should it move beyond them?
JR: Immune Checkpoint Inhibitor (CPI) therapy has really revolutionized cancer treatment. Checkpoint Inhibitor therapy today has diversified into inhibitors that can block PD-1, PD-L1, as well as the recent innovations with LAG-3 inhibitors. This has allowed immune checkpoint inhibitors to expand in use for treating multiple different types of cancer. However, even with these advancements, many patients are not eligible for treatment with CPIs and response rates remain low among those eligible. There also remain issues around treatment resistance.
While I do not think research is unnecessarily focused on checkpoint inhibitors, there is indeed a diverse array of immunotherapeutic agents that hold promise for future development, such as:
- – Novel cytokines that can trigger anti-cancer immune responses by activating and expanding cancer killing immune cells
- – Natural Killer cells, which can destroy tumour cells as well as secrete cytokines to modulate immune activity
- – Vaccines – multiple cancer vaccines are being developed targeting cancer mutations. This area of immuno-oncology has experienced particular growth in light of the success of mRNA vaccines for COVID-19. Additionally, vaccines can also target proteins which are only found in high risk populations – such as α-lactalbumin, which is not found in normal aging breast tissue after lactation, but its presence is indicative of high breast cancer risk
- – Antibody-Drug Conjugates – antibodies linked to drugs which can kill tumour cells, while not harming healthy cells
- – Bi/Tri-specific Antibodies – which can bind both to tumour cells and specific immune cells, enabling the immune system to initiate a response
I think further research will naturally include all of the above, as well as checkpoint inhibitors.
Additionally, immuno-oncology does not exist in a vacuum. It has real potential to be combined with more conventional therapies, such as chemotherapy or radiotherapy. Additionally, we can also do further research in turning tumours from immunologically inert to immunologically active using conventional agents, and then employing immunotherapies.
PF: You did mention the issue of treatment resistance – is there anything you think would benefit existing treatments, other than simply developing novel therapeutic agents? Do you feel we currently lack a deep understanding of the mechanisms behind resistance to these treatments?
JR: Treatment resistance is perhaps the biggest barrier to cross for cancer immunotherapies, particularly immune checkpoint inhibitors. We do have some predictive indicators of treatment responsiveness – for example, high tumour mutational burden (TMB) and high microsatellite instability (MSI) are positively correlated with responses to checkpoint inhibitor therapies such as PD-1 and PD-L1. Work in this area continues, and better record-keeping in the biomarker profiles of people who do respond to treatment is good practice for any trial.
But where more work needs to be done, especially in the future, is improving our understanding of non-responsive patients. Particularly when determining whether a tumour is hot or cold (with the former being a tumor that is exposed to the immune system, while the latter is not), we need to improve our analyses so as to better understand multiple factors:
- – The tumor’s microenvironment
- – Their cell populations
- – Characteristics unique to their own immune system
- – T-cell exhaustion
Additionally, we need to differentiate better between the different types of treatment resistance that can be observed: primary refractory (tumours that never responded to treatment), checkpoint resistance, tumours that did respond to treatment but progressed later. Different treatments offer varied outcomes dependent on the type of resistance observed – particularly in tumours that did respond but progressed.
Immuno-oncology can learn a lot from assimilating these lessons, improving non-responder analysis, and using this information to develop better clinical procedures in future treatments, as well as improving patient selection.
PF: Are there any more specific methods you think would be valuable in improving our understanding of treatment resistance and overcoming it, as well as immunotherapies in general?
JR: One of the most important inputs of data for improving our understanding of study participants is regular tissue sampling through biopsies. It is critical that researchers are able to assess not just the peripheral environment of the tumour, but also the internal microenvironments – and that is only possible through biopsies. The conditions prior to, and after, treatment should be compared not just between themselves, but also between the peripheral and micro- environments. The same should be true of the biomarker profile of each participant.
Obviously, there is a limit to how many biopsies can be conducted – and not every participant will be happy to have as many biopsies as would be ideal to illustrate the maximum amount of data. Liquid biopsies do offer a way around this, enabling us to observe the peripheral environment of the tumour. But they still do not yield definitive answers about the microenvironment of the tumour.
When developing new treatments, we also need to perform effective risk-benefit analyses, particularly with the potential toxicity of treatments. Improving treatment response is just one measure of improved treatment; maintaining treatment while reducing toxicity could be another.
PF: You’re part of the facilitating team for our strategy meeting – is there anything you feel that should be definitely covered?
JR: I think the strategy meeting has a jam-packed agenda with brilliant people that I have known for many years. It brings together great scientists and innovators. Your sessions on innovative trial designs also exhibit the need for better trials in oncology, and life sciences in general; we ourselves are always trying to improve our trial design. And as we said, cytokines, NK cells, vaccines and other new developments in oncology mean that the field is experiencing exciting times. I am also thrilled to be able to meet great mentors, friends and to share our collective thoughts and what there is to come.
PF: Yes thank you – we are also very excited to have you and look forward to returning to face to face events this year. We strongly believe that physical meetings have an important role to play in the exchange of information and ideas.
Jessicca Rege will be talking about going beyond the Immune Checkpoint Blockage at the Oncology Strategy Meeting organized by Proventa International in Boston in 2022. Join the meeting for a diverse array of insights from throughout oncology and the opportunity to exchange ideas with world-renowned experts

Nick Zoukas, Former Editor, PharmaFeatures
Drishti Goel, Producer, Proventa International
Subscribe
to get our
LATEST NEWS
Related Posts

Interviews
Innovating the Canadian Biotech Sector with Joseph Mancini, adMare BioInnovations
With a wealth of globally-competitive scientific discovery, Canada is primed to lead the life sciences world. adMare is here to make that a reality!

Interviews
Leveraging Technology to Accelerate Trial Recruitment with Colleen Hoke, ObjectiveHealth
Utilizing proprietary technology, processes and trained on-site personnel, ObjectiveHealth delivers significant advances in the conduct of clinical research.
Read More Articles
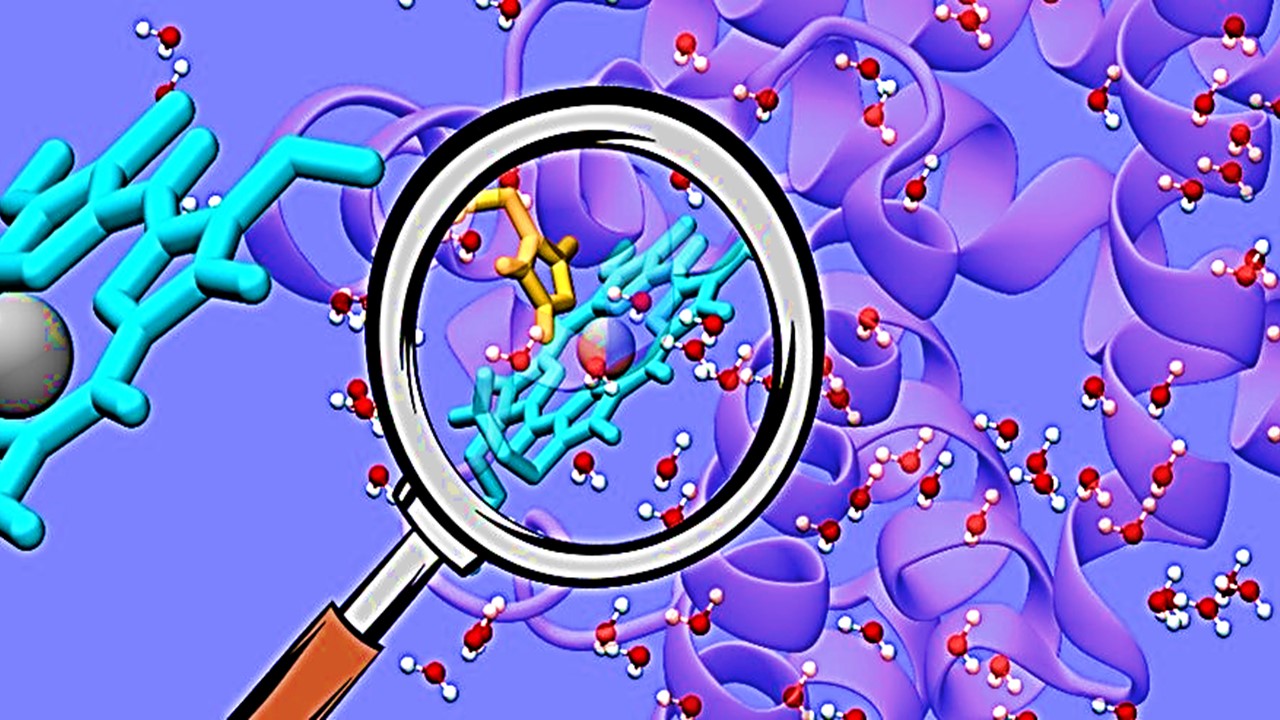
Synthetic Chemistry’s Potential in Deciphering Antimicrobial Peptides
The saga of antimicrobial peptides unfolds as a testament to scientific ingenuity and therapeutic resilience.