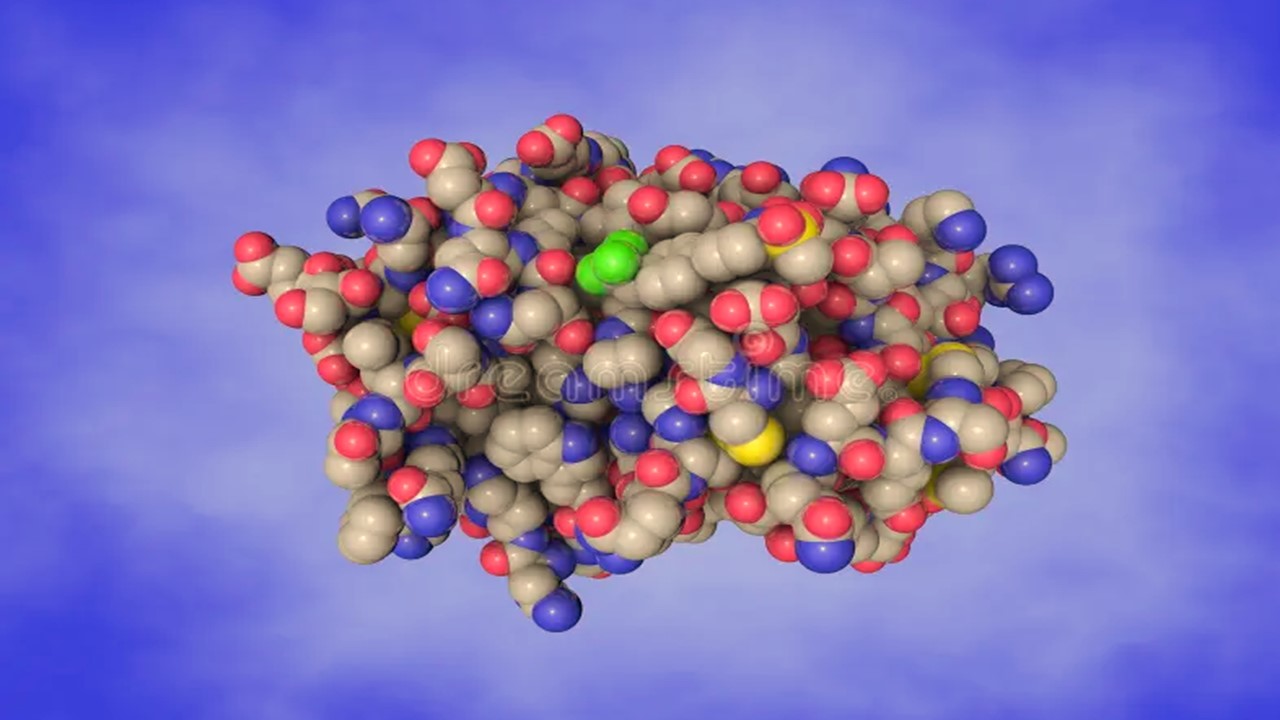
Human Immunodeficiency Virus (HIV) exerts a profound impact on the immune system, predominantly targeting and dismantling crucial components of innate defense mechanisms. This intricate process of immune dysregulation orchestrated by HIV results in a state of immunodeficiency, leaving the host vulnerable to opportunistic infections and malignancies. A comprehensive examination of the intricate molecular interactions and immunological perturbations induced by HIV unravels the complexity underlying the pathogenesis of HIV/AIDS, emphasizing the critical role of immune reconstitution strategies in managing this devastating disease.
HIV and CD4+ T Cell Depletion
HIV is a retrovirus that selectively infects CD4+ T cells, which serve as key orchestrators of the immune response. Through the utilization of the CD4 receptor and chemokine co-receptors, HIV gains entry into CD4+ T cells, leading to viral integration, replication, and ultimately, the destruction of infected cells. The depletion of CD4+ T cells, both in the peripheral blood and lymphoid tissues, is a hallmark of HIV infection and a major contributor to immune impairment.
Impact on Innate Immune Components
In addition to its direct impact on CD4+ T cells, HIV perturbs numerous other components of the innate immune system. Dendritic cells, critical antigen-presenting cells that bridge innate and adaptive immunity, become dysfunctional and fail to effectively activate T cell responses. This impairs the initiation of adaptive immune responses and compromises the ability to control viral replication. Macrophages, important phagocytic cells involved in host defense, can also be infected by HIV and serve as viral reservoirs, contributing to the persistence of the virus. Moreover, natural killer (NK) cells, key effectors of innate immunity, exhibit functional impairment during HIV infection, compromising their ability to recognize and eliminate infected cells.
Chronic Immune Activation and Dysregulation
The immunological consequences of HIV infection extend beyond the depletion of immune cells. Chronic immune activation, characterized by persistent inflammation and heightened immune responses, is a defining feature of HIV infection. Dysregulation of cytokine networks, disruption of the gut-associated lymphoid tissue, and perturbation of the gut microbiota contribute to this chronic immune activation. In turn, sustained immune activation drives immune exhaustion, whereby immune cells become functionally impaired and unable to mount effective immune responses.
Opportunistic Infections and Malignancies
The resulting immunodeficiency observed in HIV/AIDS leaves individuals susceptible to a wide range of opportunistic infections, including those caused by bacteria, viruses, fungi, and parasites. Furthermore, the increased incidence of certain malignancies, such as Kaposi sarcoma and non-Hodgkin lymphoma, underscores the compromised immune surveillance and control of oncogenic viruses in the setting of HIV-induced immunosuppression.
Antiretroviral Therapy (ART) and Immune Reconstitution
To address the immunodeficiency associated with HIV/AIDS, immune reconstitution strategies have emerged as crucial components of disease management. Antiretroviral therapy (ART) serves as the cornerstone of treatment, effectively suppressing viral replication and allowing immune recovery. By reducing viral load, ART allows for partial restoration of CD4+ T cell counts, mitigates chronic immune activation, and decreases the risk of opportunistic infections. However, complete immune reconstitution is often not achieved with ART alone, necessitating additional interventions to optimize immune recovery.
Strategies for Immune Reconstitution
Approaches to immune reconstitution in HIV/AIDS encompass the administration of immune modulators, such as interleukins or growth factors, to enhance immune cell production and function. Therapeutic vaccination strategies, aimed at stimulating HIV-specific immune responses, hold promise in boosting immune control of the virus. Furthermore, efforts to restore thymic function, either through thymic transplantation or regeneration, aim to rejuvenate the production of naïve T cells and enhance overall immune reconstitution.
Challenges and Future Directions
The complex and dynamic interactions between HIV and the immune system present ongoing challenges in the pursuit of effective immune reconstitution strategies. The delineation of the intricate molecular pathways, immune cell dysfunctions, and immunological perturbations induced by HIV infection serves as a foundation for the development of innovative therapeutic approaches. Continued research endeavors, driven by advanced technologies and interdisciplinary collaborations, hold the promise of unlocking novel avenues for immune reconstitution, ultimately leading to improved management and outcomes in HIV/AIDS.
Engr. Dex Marco Tiu Guibelondo, BS Pharm, RPh, BS CpE
Subscribe
to get our
LATEST NEWS
Related Posts

Immunology & Oncology
Forging a Hopeful Outlook on Cancer Drug Development
The core of oncotherapy is still about reducing human suffering and facing the many challenges of this disease together.

Immunology & Oncology
Patterns, Profiles, and Patient Outcomes: AI in Oncotherapeutics
AI presents a beacon of hope in revolutionizing cancer management across various stages.
Read More Articles
Synthetic Chemistry’s Potential in Deciphering Antimicrobial Peptides
The saga of antimicrobial peptides unfolds as a testament to scientific ingenuity and therapeutic resilience.