Dr. Randi Isaacs is a haematologist & oncologist currently serving as the Chief Medical Officer for Werewolf Therapeutics, a company specializing in conditionally-activated immunotherapies to advance the fight against cancer. Werewolf focuses on the development of INDUKINE™ molecules, which combine proven immunomodulators with engineering enhancements for their activity and specificity. Dr. Isaacs will be joining Proventa International’s Oncology Strategy Meeting, in an effort to advance the discourse on the rapidly growing field of immuno-oncology.
PF: Good day Dr. Isaacs – it is such a pleasure to host you for an interview and have a glimpse into the life-saving work you are doing. You have been in the area for a long time – how would you describe your career?
RI: I am the Chief Medical Officer for Werewolf Therapeutics, a soon-to-be clinical stage biotechnology company that is focused on the delivery of pro-inflammatory mechanisms, particularly cytokines. I have been in oncology drug development for well over 20 years and I am a haematologist and oncologist by training. My specialization during my career lies squarely within the field of biologics, including monoclonal antibodies, antibody-drug conjugates, bispecific antibodies, T-cell engagers and adoptive cell therapies. My own career in the industry began, more years ago than I’d like to say, in cytokines – and now my work has come back full circle. Prior to Werewolf, I spent ten years at the Novartis Institutes for Biomedical Research, as the site head for early clinical development in Oncology, in New Jersey. There, I worked with a multidisciplinary team of physicians and scientists, all belonging to different programmes and with various other areas of expertise. As such, I have seen drug candidates through to their registration, but my passion remains in the early development space – which makes my current occupation with Werewolf Therapeutics all the more exhilarating.
PF: Indeed, your career in Oncology has been storied and distinguished – and the way it has come back full circle to cytokines seems really fitting, much like how the industry is now revisiting the subject. What makes you so passionate about Immuno-oncology?
RI: My primary motivation lies in the beauty of our immune system, and its innate functions to fight tumours. The field of immuno-oncology, and the immunotherapies that are being developed, utilise various mechanisms to recruit the immune system to fight against cancer, in line with its original intended purpose. At the stage where a tumour becomes malignant, a threshold of evasion is crossed – beyond which the tumour cells are able to elude the immune system and allow themselves to grow unchecked. Immuno-oncology seeks to correct this “malfunction” – which is what fascinates me. Additionally, immunotherapy had been on the periphery of oncological research for many years. As our understanding has grown, and as we have innovated life-extending and curative therapies such as immune checkpoint inhibitor therapies, including the recent innovations in anti-PD and anti-PDL1 inhibitors, there is now a prominent place for immunotherapies among the various treatment modalities available to oncologists.
PF: Indeed – I imagine seeing a field grow with you forms a special type of attachment, one that stays with you for life. And it is true that immunotherapies are a relative newcomer to the mainstream of oncological therapies – what is it that you would say makes them different?
RI: Current immunotherapies reinvigorate immune systems that no longer recognise cancer cells as unwanted, or they often take the brakes off of suppressive mechanisms that prevent the immune system from interacting with the cancer. Such suppressive mechanisms can be very prominent, and we have seen success in targeting them with immune checkpoint inhibitor therapies. Checkpoint inhibitors can lead to long-term control over various types of cancer, which is a very rare phenomenon in advanced tumours. For example, we have seen the possibility of strong remissions in metastatic melanoma cancers and even cures, when treated with Interleukin-2. For many years, metastatic melanoma had been an untreatable, fatal condition.
I also think it is important to differentiate immunotherapy from targeted therapeutics, which take advantage of genetic mutations or cell surface antigens, which can act as gateways to the cells, on their target tumours. Examples of these include tyrosine kinase inhibitors which may take advantage of EGFR mutations in lung cancer, or inhibitory monoclonal antibodies for tumours that overexpress proteins like HER2. Immunotherapy instead is a more non-specific mechanism, recruiting cells of the immune system. However, it does share some commonalities with targeted therapies – notably the need for better patient selection in studies. This is an area open to large improvements through enhanced data gathering.
PF: That rolls along nicely into my next question – the low responsiveness rate often associated with immunotherapies is an obvious area for improvement – particularly with regard to patient selection. What are other areas that need to be addressed, particularly within your field of cytokines?
RI: One of the key areas where we can address gaps in immunotherapeutic treatment is maximising the therapeutic benefit of immunomodulators while minimising the toxicities. Pro-inflammatory cytokines are a class of over a dozen immune regulators which play a critical role in a diverse range of innate and adaptive immune mechanisms, and are capable of stimulating very potent antitumor immune responses. However, there are objective challenges in developing them as systemic immune therapies for two main reasons: they have poor drug-like properties: very short half-lives in circulation, very poor tissue distribution, and low specificity. As a consequence, pro-inflammatory cytokines can elicit immune activation in normal tissues as well. Their systemic administration often causes serious toxicities and adverse reactions owing to this. The body intends cytokines to act as indiscriminate agents – but for them to be potent immunotherapeutics, specificity is key. This is why Werewolf Therapeutics’ INDUKINE molecules aim to be conditionally activated when arriving to the tumour microenvironment. This would allow us to deliver them systemically, but harness their effects in the tumour microenvironment. We aim to minimize risks with the Werewolf platform and our pro-inflammatory mechanisms that can prevent the toxicities inherent to current systemic administration, thereby enhancing the risk-benefit profile; especially in refractory tumour settings. This is important regarding IL-2 and IL-12, which may have monotherapy potential for patients who have failed all other therapeutic options.
PF: Moving back to the previous question, immuno-oncology is definitely straddling the line between conventional and precision medicine in nearly all its incarnations, given how much of its effectiveness depends on specific biomarkers and factors that tend to be individual to subsets of patients. This often leads to a nearly endless need for ever more detailed data in immunotherapy studies – would you agree?
RI: Of course. A richness of data collection translates directly to better patient selection, which is one of the main drivers of success in the clinical development of immunotherapeutic agents. It is critical that current clinical studies incorporate robust biomarker analysis on blood and tumour tissues to create large databases that can facilitate a better understanding of the mechanisms of action, underpinning their investigational products. In turn, these can further assist in identifying patients best suited to these, or related, therapies. This is perhaps the first lesson one should learn in immuno-oncology – just think back to the amount of data that was necessary to demonstrate that checkpoint inhibitors could be utilised in a select patient subset, those with high PDL-1 expression in non-small cell lung cancer. It took enormous amounts of data to establish one specific patient selection strategy, and it is a strategy that does not always translate to the same effectiveness in combination studies. The more data we can glean, the better: this is the approach Werewolf is taking as it moves forward with its two most advanced Indukine candidates, WTX-124 and WTX-330, which aim to treat advanced malignancies. Both programmes have very robust biomarker analysis as part of the first in human clinical studies.
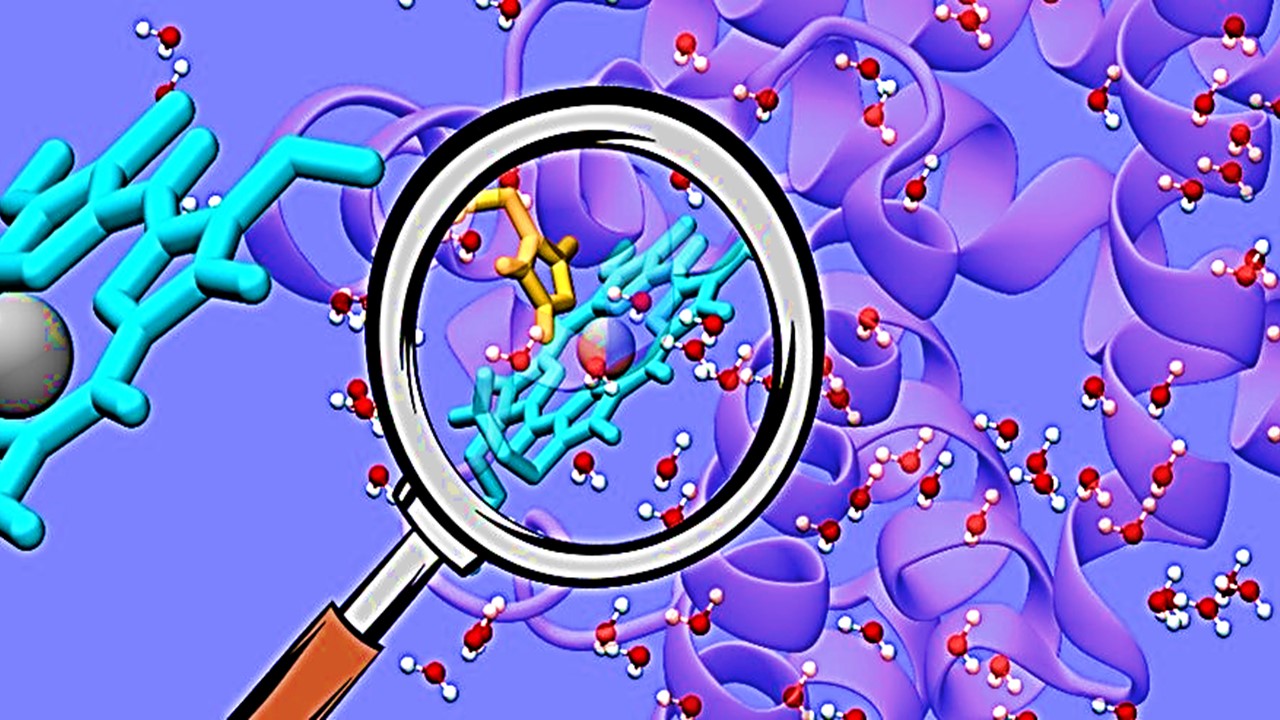
Another critical area for further study is the tumour microenvironment (TME) – especially for the development of therapies targeting its immuno-suppressive properties. Werewolf’s approach is to leverage our PREDATOR protein engineering platform, which aims to design conditionally activated molecules that stimulate both the innate and adaptive arms of the immune system and are applicable to a wide range of tumours. Our INDUKINE molecules are intended to remain inactive in healthy tissue yet activate selectively in the tumour microenvironment via cleavage from dysregulated tumour proteases. This is one of the possible approaches of improving the specificity of cytokine therapy – and it is the approach Werewolf is taking.
PF: That does sound promising – obviously, you see great potential in cytokines. Do you also see potential in their use within combination therapies, which have become a key trend in immuno-oncology?
RI: First and foremost, I would advocate that combination therapy is the mainstay of oncology. The value of checkpoint inhibitors has already been established, and I would not question it.
Combinations, including those that involve multiple immunotherapy agents, conventional therapies, or even adoptive cells, are something we must continue to explore. The synergistic effects they provide are often invaluable to deepen responses, and the way they prevent tumours from developing treatment resistance even more so. Additionally, multiple combination therapies have been proven to enhance the properties of immunotherapeutic agents. A well established example would be chemotherapy and radiotherapy, which can lead to neo-antigen presentation, reinforcing the ability of the immune system to target the tumour. We do have to be careful, however, as can be seen on the various registries of clinical trials, that there are many combination therapies that are being investigated. We need to choose these combinations wisely and carefully to think about how best to provide for patients. We need to provide the most promising, rational combinations for patients based on the evolving pre-clinical and clinical data.
PF: With a view towards 2022, do you think immuno-oncology will finally be able to shake off the mainstream perception that it only “sometimes works”, and have its potential realized?
RI: When answering this, I would be thinking about where we were when I started my career; since then, we have managed to actually find innovative critical therapies for a number of different cancer therapies that have extended lives and cured patients. We have peeled back many layers of the cancer problem. I am very hopeful for the future – I look at some haematological malignancies, and how we could say we have cures for them. I look at where we are with adoptive cell therapies and targeted therapies for certain tumour genotypes, which gives me hope. We continue to make breakthroughs because of our technological advances – whether it be with the modification of genes or protein engineering like we are doing with Werewolf and our modular proteins. It all consists of small steps towards transformational therapies.
PF: Regarding our oncology strategy meeting, is there anything you would be looking to explore or something to look forward to?
RI: I always love to hear what my peers are interested in and are presenting; we all learn from each other – which I feel is the most exciting thing about forums, observing the scientific advances brought about by our colleagues. And it also gives us an opportunity to put things together; many scientific advances come from the confluence of different ideas – the repurposing of ideas that may at first seem completely disparate, which are then applied to one’s own research. This is why I am excited to attend the conference!
Join Proventa International’s Oncology Strategy meeting in Boston for the latest insights in oncology; Dr. Randi Isaacs will be discussing the unique challenges presented by solid tumours for immuno-oncological treatments. Other world-renowned experts and professionals will present their own views on a plethora of subjects in the field.

Drishti Goel, Producer, Proventa International
Nick Zoukas, Former Editor, PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts

Interviews
Leveraging Translation Services in Clinical Trials with Stephane Millet, Acolad
Stephane Millet highlights the strength of Acolad’s leadership in delivering content that empowers, anywhere.

Interviews
Innovating the Canadian Biotech Sector with Joseph Mancini, adMare BioInnovations
With a wealth of globally-competitive scientific discovery, Canada is primed to lead the life sciences world. adMare is here to make that a reality!
Read More Articles
Synthetic Chemistry’s Potential in Deciphering Antimicrobial Peptides
The saga of antimicrobial peptides unfolds as a testament to scientific ingenuity and therapeutic resilience.