Amit Agarwal is the Senior Vice President for Clinical Development at Arch Oncology. Arch Oncology focuses on the development of antibody-based therapies for anti-cancer treatment. Arch Oncology specialises in anti-CD47 treatments – their lead product, AO-176, preferentially binds to tumour cells and enables macrophages to interact with them, in addition to performing a variety of other functions to destroy tumours.
PF: It is a genuine pleasure that you’ve agreed to this interview, Dr. Agarwal. Could you give us some background information on your own activities and work interests?
AA: Aside from being the SVP for Clinical Development at Arch Oncology, I am also a board-certified haematologist and oncologist. Prior to joining Arch I was involved in drug development and oncology for over 10 years – both at academic institutions and biotech companies . These include Celgene Corporation and Bristol Myers Squibb. Before that, I worked at the University of Arizona’s Comprehensive Cancer Center, where I cared for patients with haematological malignancies, as well as involving myself in multiple clinical trials for cancer therapies and translational research.
I have been fortunate to work in various spaces of oncological research. After medical school I did a PhD in Cancer Genetics. After carrying out more translational work, and seeing more patients on the clinical side of things – including work in Phase I & II studies, I was strongly drawn towards clinical development and management. I often describe my career journey as a sort of pendulum – swinging back and forth between medical care and clinical and translational research.
PF: As our understanding of cancer biology grows, so does the promise of more precise treatments – do you think this is the direction clinical research should follow in the future as well?
AA: I think you are absolutely right. We have seen significant growth and expansion in our understanding of tumour biology. And rightly so: cancer is not a simple disease – or even the same kind of disease across patients to begin with. Tumours are extremely heterogeneous, and standard treatments such as radiotherapy and chemotherapy will not have uniform effects across such different conditions. We have begun to characterise tumours based on very deep genetic and immunologic profiling on a regular basis.
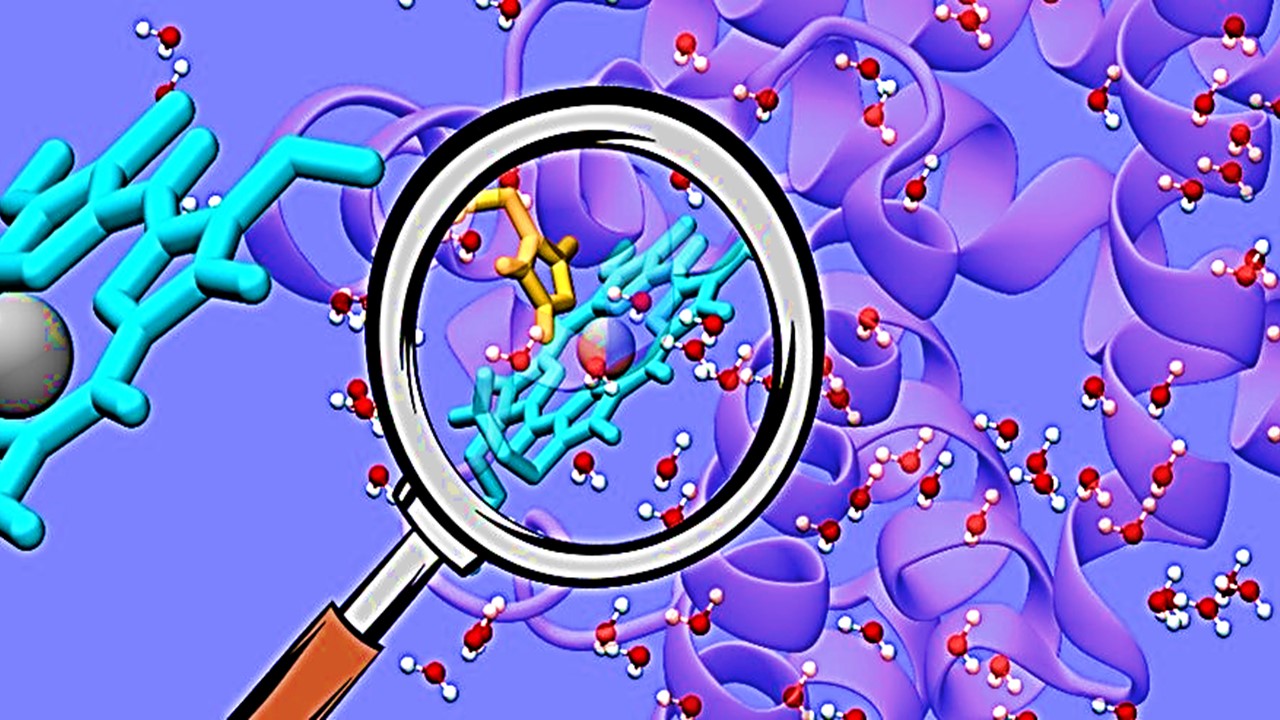
With personalised medicines in particular, it is extremely important to have a thorough understanding of how treatments interact with the tumour on a cellular and molecular level. This is why detailed models of pharmacokinetic and pharmacodynamic (PK/PD) activity are critical. But for these to be effective and understandable, we need concrete agreements on standardisation across industry and academia. This has already started to happen – one example would be Tumour Mutational Burden (TMB). With TMB, all key stakeholders have come together to agree on the way it will be defined for all future clinical trials. With an eye towards the future, this is something that should happen more prospectively rather than retrospectively.
Of particular importance is optimising our risk:benefit analyses to manage all the new therapies that are becoming available in immuno-oncology. This includes antibodies, cancer vaccines, adoptive cell transfers, checkpoint inhibitors, tumour-infecting viruses, cytokines and adjuvants. These analyses must grow as clinical trials progress. Their importance is even greater in searching for a Recommended Phase II Dose or RP2D.
In the past, the common approach was to try different doses in animal studies and approach the MTD in human studies. Precision medicine drugs don’t necessarily need to reach the MTD to be effective. Based on PK/PD analysis and a deeper understanding of how the active ingredient interacts with the target, we can minimise doses without pushing the boundaries for tolerability. The importance of this cannot be underestimated – not only would less toxic treatments be safer, but they would massively increase patient quality of life as well.
PF: Do you still feel that there are any evidence gaps that still need to be addressed in the existing framework that warrant attention?
AA: There are always evidence gaps and things that could be done better, of course – that is the point of research. There is definitely a need to ask questions about potential biomarkers throughout the drug development process. There are some areas, where work has just begun, such as SIRPα where there is a need for more evidence. The CD47/SIRPα pathway, where the SIRPα protein binds to CD47 and inhibits macrophages from attacking tumour cells, is an immune checkpoint that Arch Oncology has been working on disrupting through developing antibodies that can enable the phagocytosis of tumour cells. These antibodies have well-characterised mechanisms of function, and we also have some idea of how they work in combination with our lead anti-CD47 antibody, AO-176. But we need to start biomarker development as soon as the drug is being developed; this is true for the entire field of immuno-oncology, as our drugs are highly precise and require defined biomarkers because the biology of how they work is simply not linear.
And I think that underscores the importance of composite scores in precision immunotherapies – biomarkers which can be measured in graded units rather than binary yes/no states. This is particularly important when biomarkers exhibit dependencies or interactions with each other – especially for combination therapies that are also interrelated, such as combination treatments with immune checkpoint inhibitors.
Another evidence gap would be real world data with real world studies. Real world data collection has made significant progress, particularly with smart technology and applications. A time-old criticism of such data was that conclusions drawn from it could not be trusted, simply because the data source was not trustworthy either – “garbage in, garbage out”. But we now have much better data.
PF: How do you think clinical trials can be better designed for patients that will benefit the most from candidate therapies?
AA: This is perhaps the million-dollar question; improving patient selection is a massive factor in trial development and its future success. Part of the answer depends on how much is known about a particular drug and its target. In cases where the candidate interacts with certain genetic mutations, it might be easier to design trials that select for that particular mutation. In cases where the candidate is an antibody that targets a marker, the situation is more complex. This is a situation where more continuous surveillance of biomarkers and deep translational understanding of PK/PD and how the drug may be affecting the target and what might be happening is required – clinical design of course has to adapt to that. By Phase II & III, biomarkers need to be incorporated in a much more meaningful manner, especially in trying to narrow down populations and design improvements for master & adaptive trials. As more trials occur, more improvements should be seen in biomarker understanding, as well.
I think the emergence of novel trial designs will have a big impact on not just genome-driven oncology, but precision oncology in general. As we move away from MTD and start to employ individualised dosing and translational understanding, the design of trials will be further innovated. A second theme I think that is becoming obvious is the use of master protocols which answer key questions in the precision oncology space. When there is a degree of uncertainty, further adding adaptive trials to explore a greater clinical development space is particularly helpful. We have to further adapt to the level of complexity in biomarker diversity and design that should be included in each trial – whether that be two or three biomarkers in addition to combination therapies, etc. Adaptive trials can help overcome challenges presented by these phenomena, especially in Phase IIs. Traditional trials will remain very useful for confirmatory analyses and once the signal is clear, however.
PF: You will be one of the facilitators for one of our round-table discussions – what do you think you will be looking to explore in our meeting in 2022?
AA: Personally I’m very excited about the oncology strategy meeting. It will allow us to meet colleagues after a long time – and your list of faculty and topics to be covered is wonderful. I am looking forward to mutual learning experiences in the meeting.
Drishti Goel, Producer, Proventa International
Nick Zoukas, Former Editor, PharmaFEATURES

Subscribe
to get our
LATEST NEWS
Related Posts

Interviews
Innovating the Canadian Biotech Sector with Joseph Mancini, adMare BioInnovations
With a wealth of globally-competitive scientific discovery, Canada is primed to lead the life sciences world. adMare is here to make that a reality!

Interviews
Leveraging Technology to Accelerate Trial Recruitment with Colleen Hoke, ObjectiveHealth
Utilizing proprietary technology, processes and trained on-site personnel, ObjectiveHealth delivers significant advances in the conduct of clinical research.
Read More Articles
Synthetic Chemistry’s Potential in Deciphering Antimicrobial Peptides
The saga of antimicrobial peptides unfolds as a testament to scientific ingenuity and therapeutic resilience.