The process of developing a new drug is a complex and intricate journey that requires meticulous planning, scientific expertise, and unwavering dedication. From the initial discovery of a potential drug to its availability to the general public, this article explores the various phases of clinical trials and their significance in bringing new treatments to those in need.
Phase 1 Clinical Trials: Unveiling the Safety Profile
Phase 1 clinical trials mark an important milestone in the drug development process, where the focus shifts from laboratory and animal studies to human subjects. This phase serves as a critical foundation for subsequent phases of clinical trials and plays a pivotal role in assessing the safety, tolerability, and pharmacokinetics of a new drug.
Selection of Healthy Volunteers. During Phase 1, a small group of carefully selected healthy volunteers becomes the first participants in human trials. These individuals are usually closely monitored and provide informed consent to participate. Healthy volunteers are chosen to establish a baseline understanding of the drug’s effects in the absence of underlying medical conditions, which helps isolate the drug’s impact on the body.
Evaluating Safety and Tolerability. The primary objective of Phase 1 trials is to evaluate the safety and tolerability of the new drug. Researchers administer varying doses of the drug to determine the maximum tolerated dose (MTD) without causing severe or intolerable side effects. The focus is on carefully observing any adverse reactions, documenting the body’s response to different doses, and ensuring participant well-being throughout the process.
Assessing Pharmacokinetics. Pharmacokinetics refers to how a drug is absorbed, distributed, metabolized, and excreted by the body. Phase 1 trials provide valuable insights into the pharmacokinetic profile of the new drug. Researchers analyze factors such as absorption rate, bioavailability, distribution in various tissues, metabolism, and elimination patterns. This information helps in understanding how the drug behaves within the body and guides subsequent dosing strategies.
Determining Optimal Dosage. Phase 1 trials also involve dose-ranging studies to identify the optimal dosage range for further testing. Researchers carefully escalate the dosage, starting from low levels, to establish a dose-response relationship. By analyzing the drug’s effects at different doses, researchers can determine the dosage that offers the most favorable balance between efficacy and safety.
Establishing Safety Parameters. The safety and well-being of participants are paramount during Phase 1 trials. Extensive monitoring of participants’ vital signs, laboratory tests, and adverse event reporting is conducted throughout the study. If any unexpected or severe adverse reactions occur, the trial may be modified or halted to ensure participant safety.
Building a Foundation for Subsequent Phases. Phase 1 trials lay the groundwork for subsequent phases of clinical trials. The insights gained from this phase help researchers make informed decisions regarding the drug’s further development. The safety, tolerability, and pharmacokinetic data generated in Phase 1 serve as critical inputs for designing and optimizing subsequent phases, such as Phase 2 and Phase 3 trials.
Phase 2 Clinical Trials: Expanding the Scope
After successfully completing Phase 1 clinical trials, the drug development process moves forward to Phase 2, which is a crucial step in evaluating the effectiveness of the new drug. In Phase 2 trials, a larger group of participants, consisting of both volunteers and patients with the specific condition or disease targeted by the drug, is enrolled. This phase aims to gather preliminary data on the drug’s effectiveness and assess its potential benefits in treating the intended disease.
Expanding Participant Pool. Phase 2 trials involve recruiting a larger group of participants compared to Phase 1. The participants selected for Phase 2 trials have the specific condition or disease for which the drug is intended to treat. By including individuals who represent the target patient population, researchers can better understand how the drug interacts with the disease and assess its potential efficacy.
Assessing Drug Effectiveness. The primary objective of Phase 2 trials is to gather preliminary data on the drug’s effectiveness. Researchers closely monitor the participants’ response to the drug, measuring relevant outcomes and endpoints specific to the targeted disease. These endpoints may include improvements in symptom severity, disease progression, laboratory markers, or other measurable indicators of therapeutic benefit. The data collected during this phase helps determine whether the drug shows promise in treating the intended condition.
Dose-Ranging and Treatment Optimization. Phase 2 trials often involve assessing different doses or dosing regimens to determine the optimal treatment strategy. Researchers explore various dosage levels to identify the most effective and safe dose for further evaluation in subsequent phases. This dose-ranging process helps refine the understanding of the drug’s therapeutic window and guides dosage selection for later stages of development.
Exploring Drug Safety. While Phase 2 trials primarily focus on assessing effectiveness, safety evaluation remains an integral part of the process. Researchers continue to monitor participants for any adverse effects or unexpected reactions to ensure the drug’s safety profile. By closely monitoring a larger group of participants, researchers can identify potential side effects that may have been missed in Phase 1 trials.
Generating Data for Further Development. Phase 2 trials generate valuable data that informs the decision-making process for further drug development. The findings from this phase provide critical insights into the drug’s efficacy, optimal dosing, and potential benefits in treating the targeted disease. The data collected helps researchers refine their understanding of the drug’s therapeutic potential and determine whether it is worth advancing to Phase 3 trials.
Phase 3 Clinical Trials: Rigorous Evaluation for Market Approval
Phase 3 clinical trials represent a critical stage in the drug development process, serving as the definitive assessment of a new drug’s efficacy, safety, and comparative effectiveness. These trials are designed to provide robust evidence of the drug’s benefits and to determine how it compares to existing treatments. Phase 3 trials involve a substantial number of participants, often ranging from several hundred to thousands, allowing for a more comprehensive evaluation of the drug’s performance.
Enrollment of a Large and Diverse Participant Pool. Phase 3 trials aim to include a diverse range of participants, mirroring the population that the drug is intended to benefit. By recruiting a larger and more diverse group of individuals, researchers can evaluate the drug’s effectiveness across different demographics, such as age, gender, ethnicity, and underlying medical conditions. This diversity ensures that the results are applicable to a broad population and increases the generalizability of the findings.
Multicenter Trials and Global Collaboration. Phase 3 trials are often conducted at multiple study sites across different countries. This global collaboration allows for a larger sample size and ensures that the results are not limited to a single geographic region or healthcare system. Conducting trials in various locations also accounts for differences in disease prevalence, treatment practices, and patient characteristics, enhancing the generalizability and relevance of the trial findings.
Double-Blind and Randomized Study Design. To ensure unbiased results, Phase 3 trials are typically double-blind, meaning that neither the participants nor the investigators know which treatment the participants are receiving. This approach helps eliminate bias and ensures that the results are based solely on the drug’s effects rather than participants’ expectations or the investigators’ preferences. Randomization is employed to assign participants to different treatment groups, including the new drug and existing treatments or a placebo. This random assignment helps minimize confounding variables and increases the validity and reliability of the trial results.
Comprehensive Evaluation of Efficacy and Safety. Phase 3 trials comprehensively assess the efficacy and safety of the new drug. Researchers collect data on various endpoints, such as disease progression, symptom improvement, quality of life, and survival rates, depending on the specific condition being treated. Adverse events and side effects are closely monitored to ensure the drug’s safety profile. The large sample size allows for a more accurate evaluation of the drug’s efficacy and the detection of rare or long-term side effects that may not have been observed in earlier phases.
Regulatory Review and Market Approval. Once the Phase 3 trials are completed, the comprehensive trial results, along with manufacturing procedures, formulation details, and shelf-life data, are compiled into a regulatory submission. This submission is reviewed by regulatory authorities, such as the U.S. Food and Drug Administration (FDA) or the European Medicines Agency (EMA), to evaluate the drug’s safety and efficacy. The regulatory authorities carefully scrutinize the trial data to ensure that the drug meets the required standards for market approval. Market approval signifies that the drug has demonstrated significant benefits, an acceptable safety profile, and is considered effective compared to existing treatments.
Phase 4 Clinical Trials: Continued Evaluation and Monitoring
Phase 4 clinical trials, often referred to as post-marketing surveillance trials, are conducted after a drug has received market approval from regulatory authorities. These trials play a crucial role in monitoring the long-term safety, effectiveness, and real-world performance of the drug in a larger patient population. While Phase 1 to Phase 3 trials provide essential information on a drug’s benefits and risks, Phase 4 trials provide further insights into its long-term effects and usage in diverse patient populations.
Monitoring Long-Term Safety. One of the primary objectives of Phase 4 trials is to continuously monitor the drug’s safety profile. Although extensive safety data is collected during the earlier phases of clinical development, the larger patient population in Phase 4 trials allows for the identification of rare or long-term side effects that may not have been detected in earlier stages. These trials provide an opportunity to assess the drug’s safety in real-world settings, where patients may have comorbidities or be taking multiple medications that can influence the drug’s effects.
Assessing Long-Term Efficacy. In addition to safety monitoring, Phase 4 trials also focus on evaluating the drug’s long-term efficacy. By collecting data over an extended period, researchers can assess the drug’s sustained effectiveness in treating the targeted condition or disease. This information helps clinicians and regulatory authorities better understand the drug’s performance beyond the initial clinical trials and determine its continued benefits in real-world patient populations.
Real-World Scenarios and Drug Interactions. Phase 4 trials provide an opportunity to evaluate the drug’s performance in real-world scenarios, where factors such as patient adherence, healthcare settings, and healthcare provider practices come into play. This assessment helps bridge the gap between controlled clinical trials and everyday clinical practice. Additionally, Phase 4 trials examine the drug’s interaction with other treatments commonly used in clinical practice, allowing researchers to identify potential drug-drug interactions or synergistic effects that may affect patient outcomes.
Uncovering Rare Side Effects. During Phase 4 trials, researchers can uncover rare or unexpected side effects that may not have been detected in earlier stages due to the limited sample size or duration of previous trials. With a larger patient population, these trials provide an opportunity to identify and evaluate these infrequent adverse events, providing valuable safety information to healthcare providers and patients.
Promptly Addressing Emerging Concerns. Phase 4 trials play a critical role in promptly addressing any emerging concerns related to the drug’s safety or effectiveness. By continuously monitoring and evaluating data from real-world use, researchers can identify and respond to any new or previously unknown risks associated with the drug. This ongoing assessment allows for timely modifications to labeling, prescribing guidelines, or even potential regulatory actions to ensure patient safety.
The Path to Life-Changing Treatments
The drug development process is a complex and lengthy endeavor, necessitating meticulous planning and adherence to stringent regulations. From the initial stages of preclinical testing to the final stages of post-marketing surveillance, clinical trials play a pivotal role in determining the safety and effectiveness of new drugs. These trials, conducted in multiple phases, provide valuable insights into a drug’s potential benefits and risks, ultimately shaping the future of healthcare and offering hope to patients worldwide.
As scientific advancements continue to propel the drug development process, it is essential to recognize the dedication of researchers, the importance of volunteer participation, and the stringent regulatory measures that ensure the safety and efficacy of new treatments. Together, we can navigate this journey and bring life-changing therapies to those who most need them.
Subscribe
to get our
LATEST NEWS
Related Posts

Clinical Operations
Supervised Learning: Harnessing Data to Revolutionize Patient Care
As healthcare enters a new era, the integration of ML promises to revolutionize oncology and medicine.

Clinical Operations
The Interplay of Public and Private Sectors in Pharmaceutical Innovation
A delicate balance between public and private investments shapes the pharma R&D landscape.
Read More Articles
Synthetic Chemistry’s Potential in Deciphering Antimicrobial Peptides
The saga of antimicrobial peptides unfolds as a testament to scientific ingenuity and therapeutic resilience.
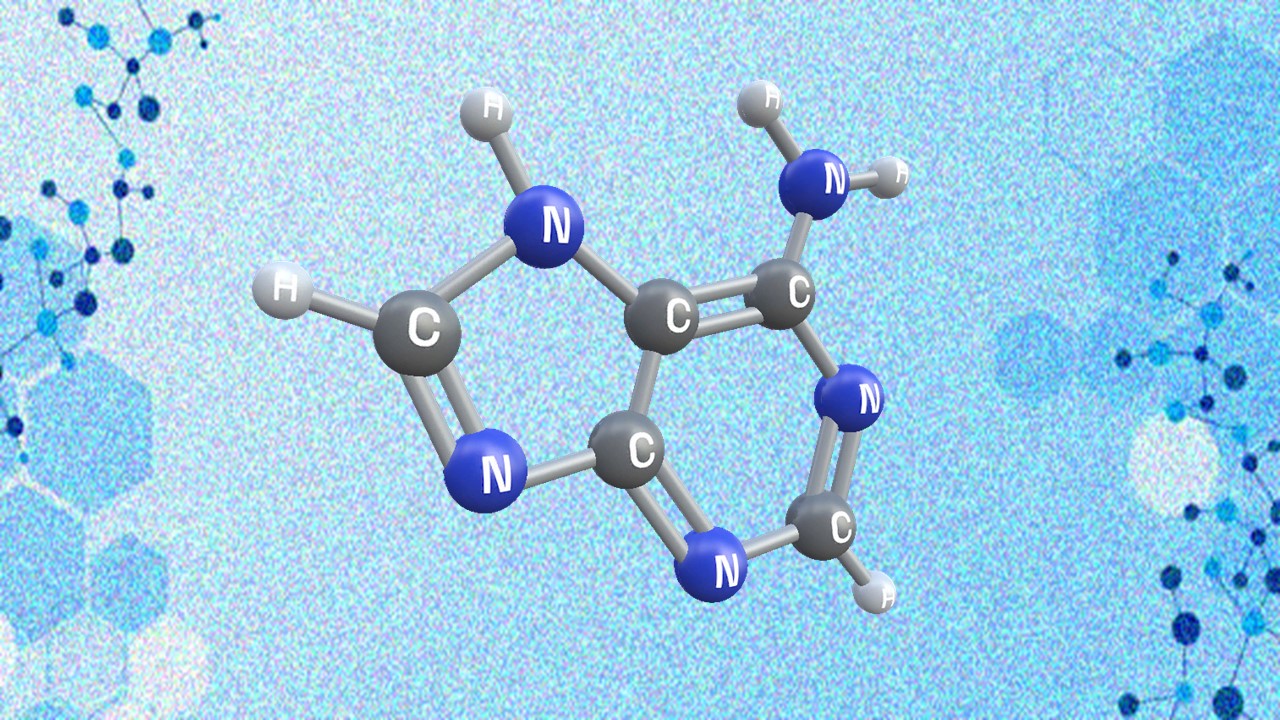
Appreciating the Therapeutic Versatility of the Adenine Scaffold: From Biological Signaling to Disease Treatment
Researchers are utilizing adenine analogs to create potent inhibitors and agonists, targeting vital cellular pathways from cancer to infectious diseases.