Cancer care has been defined by the four major pillars of treatment: surgery, radiotherapy, chemotherapy and immunotherapy. These four faithful modes of treatment have steadfastly saved and extended lives over the last century – while the pharmaceutical industry has experienced a rapid pace of innovation and refined individual agents and devices that improve upon established standards of care. However, many anticipate a fifth mode of action – particularly based upon recent trials: phototherapy. The transformative potential of providing a completely new avenue through which to eliminate cancerous cells cannot be understated – though there remain key new insights that are needed before the modality can progress further.
The Workings of Phototherapy
Treatments based on photodynamic therapy have been popular for conditions such as acne, psoriasis, atherosclerosis, and others. Recent research has also been investigating the usefulness of the therapy in treating fungal infections, as well as expanding its therapeutic role in macular disease. At its core, phototherapy harnesses the power of light to guide precise treatments that may have otherwise proven impossible or exceedingly difficult. Photodynamic therapy is the most common form. A photosensitising drug, such as porphyrins, chlorins and other dyes, are distributed to relevant tissues. Photosensitizers are typically selected for low toxicity in the absence of light and their ability to produce reactive oxygen species when excited by light.
Once activated by visible light, the drug produces reactive oxygen species – typically hydroxyl radicals, superoxide ions and singlet oxygen species, which can quickly lead to cellular death. With its potential to induce precise cytotoxic effects, photodynamic therapy is of obvious interest to oncology. The treatment strategy brings minimal invasiveness and toxicity, with the potential to simplify complex surgical procedures as well as reduce their disfiguring impact.
Examples of Success
Porfimer sodium is perhaps the oldest example of a widely used photodynamic therapy for cancer – particularly against solid tumors and high grade dysplasia in Barrett’s oesophagus. The first time a patient would receive photodynamic therapy with porfimer sodium was in 1975; FDA approval did not occur until 1994 – for palliative esophageal cancer treatments. The indication for porfimer sodium was later expanded to include non-small cell lung cancer (NSCLC). Side effects include lasting photosensitivity for months, with some association between a patient’s skin phototype and sex. Further investigations in the therapy hold the potential to minimize these side-effects.
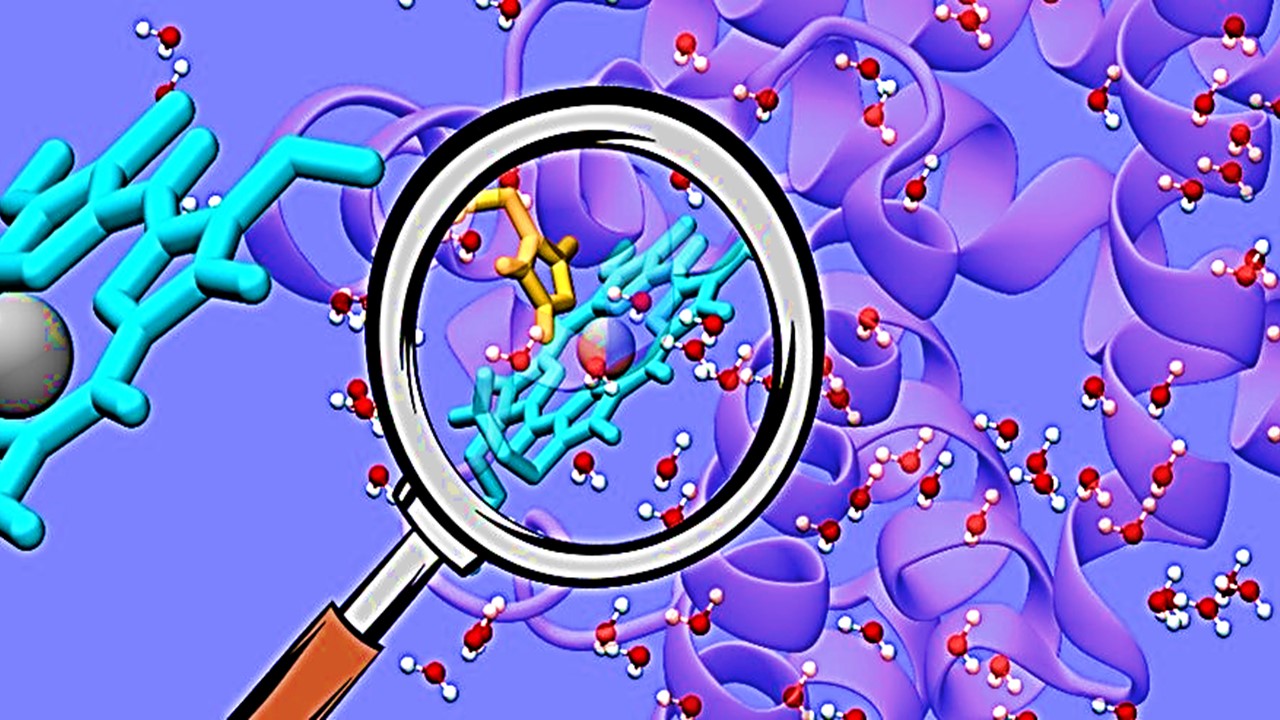
Newer agents have since been innovated, including benzoporphyrin derivatives, 5-aminolevulinic acid, as well as pheophorbide HPPH – all exhibiting similar or improved effects and accumulation profiles in neoplastic loci. Additionally, new generation photosensitizers exhibit improved light absorbance at more optimal wavelengths – such as 690nm, as well as providing additional sub-cellular targeting flexibility depending on their mode of delivery. Combinations of differing photosensitizing compounds are still a concept in its infancy. It is now widely understood that different agents can lead to cytotoxicity through various mechanisms – for example, by acting on mitochondria, the endoplasmic reticulum, or lysosomes. Using complementary agents to maximize tumor elimination is an avenue that merits further investigation.
So far however, only 5-aminolevulinic acid has been able to garner widespread use other than Porfimer sodium. The main application for 5-aminolevulinic acid, marketed as the topical treatment Levulan, is as a treatment for actinic keratosis – a condition which can progress to cancer.
Combining Arms
But the landscape is set to change, particularly as research in combining photodynamic therapy with other novel treatment modalities gains traction – especially for indications of cancer with significant unmet need. The British Institute for Cancer Research led clinical trials in mice with glioblastoma using a new form of so-called “photoimmunotherapy”. The therapy in the trial aimed to launch a multi-pronged attack on one of the most lethal forms of cancer, with glioblastoma patients exhibiting only a 6% 5-year survival rate.
The photosensitizing drug’s fluorescent properties assisted with improving operability on the tumor, making it glow in the dark. Subsequent light-activation of the photosensitizing agents cleared residual tumor cells that may not have been eliminated through surgery. Additionally, the phototherapy primed the immune system to target cancer cells in the future – providing some measure of protection from recurrence. The therapy used affibody proteins targeting EGFR to localize to the tumor, due to the overexpression of EGFR in glioblastoma tissue. The groundbreaking work made waves across mainstream media, highlighting the transformative impact of further innovations in the area.
Future Potentials
The work on photodynamic therapies and the role they have to play within the greater framework of cancer care is only just beginning to be illuminated. The modality matured from a laboratory curiosity to a treatment modality worth prominent biomedical consideration – and is now experiencing a renaissance as the oncology community seeks innovative ways to eliminate cancer. Further improvements in targeting and localizing photosensitizing compounds, as well as positive synergies with existing treatment modalities will prove crucial in establishing photodynamic therapy within the pharmaceutical mainstream.
Join Proventa International’s Oncology Strategy Meeting in Boston to hear more on photodynamic therapies in Oncology, and how they can complement other innovative immuno-oncology and antibody-guided treatment strategies!
Subscribe
to get our
LATEST NEWS
Related Posts

Immunology & Oncology
Forging a Hopeful Outlook on Cancer Drug Development
The core of oncotherapy is still about reducing human suffering and facing the many challenges of this disease together.

Immunology & Oncology
Patterns, Profiles, and Patient Outcomes: AI in Oncotherapeutics
AI presents a beacon of hope in revolutionizing cancer management across various stages.
Read More Articles
Synthetic Chemistry’s Potential in Deciphering Antimicrobial Peptides
The saga of antimicrobial peptides unfolds as a testament to scientific ingenuity and therapeutic resilience.