Companion diagnostic tests are an important part of precision medicine in oncology. In addition to matching optimal treatment options for patients, these tests enable clinicians to monitor the efficacy of therapeutic intervention in disease management. Innovations in cancer biopsies and blood tests aim to introduce more accurate and less-invasive companion diagnostics.
Introduction
According to the National Cancer Institute, companion diagnostic (CDx) tests are used to match appropriate treatment for patients with cancer. The test can identify specific genetic changes in tumours or biomarkers that are targeted by a specific drug. In addition, the tests can be used to determine whether the patient is a candidate for treatment or not. Companion diagnostics are also used to monitor the clinical response to specific drugs which helps to ensure safety and efficacy according to the FDA.
Companion diagnostics are an important tool for precision medicine in oncology as a strategy to optimise efficacy of patient treatment. Cancer pathology is highly complex: with over 100 variations of the disease and differing progression, personalised medicine is greatly sought after.
In companion diagnostics, mechanisms in molecular genomics (molecular interactions within the genome) are most associated with pathology, and as such are disease targets. Circulating tumour cells (CTCs) and circulating free tumour DNA (ctDNA) are the two main biomarkers detected by liquid biopsy (the analysis of tumour physiology using biomarkers circulating in bodily fluids). ctDNA is becoming an increasingly popular biomarker for a variety of tumours.
The presence of ctDNA arises when tumour cells release DNA into surrounding tissue, either via apoptosis (programmed cell death) or active secretion. The ctDNA is then delivered into the bloodstream. Circulating ctDNA is then identified by specific genetic mutations for a tumour type. Quantifying the biomarkers present measures the effect of treatment relative to disease progression, hence is an important part of treatment choice and disease management.
Barriers to use
The delivery of CDx tests is a topic under debate. While invasive diagnostic tests are potentially more accurate as they involve directly testing a patient’s tissue, they are often unpleasant and sometimes painful procedures. Hence, there is a clinical need to develop less invasive alternatives which are widely available and match the accuracy of invasive techniques.
Unfortunately, there are a multitude of barriers that prevent CDx tests being used in clinical practice. According to a recent article, inefficient market development planning for CDx tests prevents approximately 50% of cancer patients from receiving the correct test for “biomarker-guided treatment”. Other factors include that the test is not always required, and a sample is not always available. These challenges will need to be addressed to allow the right patients to benefit from some of the new tests that have recently been developed.
Latest innovations in next-generation techniques
Blood samples over invasive procedures
In March 2020, the IMvigor011 study reached phase III of an oncology clinical trial using Signatera, a companion diagnostic created by Natera. Natera is a clinical genetic testing company that specialises in cell-free DNA testing technology. Their focus is primarily on women’s health, organ health and oncology. In an article published in early 2020, it describes the randomised clinical trial, sponsored by Genetech Initiate, which was launched to evaluate the safety and efficacy of adjuvant treatment with the PD-L1 inhibitor. Eligible patients are to be screened with Signatera, a companion diagnostic used to identify muscle-invasive urothelial carcinoma.
Signatera is a customised ctDNA test that monitors treatment and also assesses molecular residual disease (MRD) in patients with previous cancer diagnoses. According to the article, the companion diagnostic requires only a blood sample with blood tests that are personalised to each individual relative to the genetic signature of mutations found in a tumour.
This is an example of the exciting developments in invasive companion diagnostics techniques which maintains accurate detection of disease as well as creating a procedure better tolerated by patients. This particular diagnostic test has been used to “detect recurrence earlier and to help optimize treatment decisions.” The test awaits FDA approval.
Liquid biopsies and next-generation sequencing
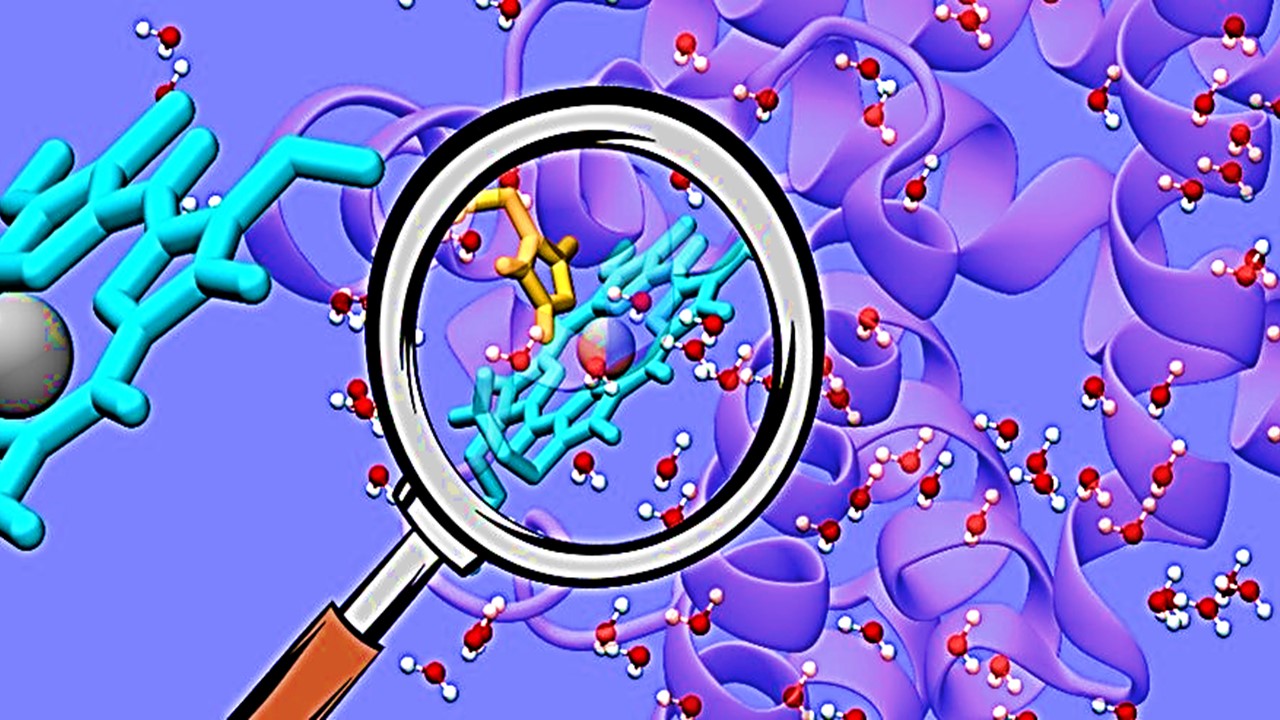
In August 2020, the FDA approved the first liquid biopsy companion diagnostic – Guardant360 CDx assay. According to an FDA press release, this test uses next-generation sequencing (NGS) to recognise patients which present specific mutations of the epidermal growth factor gene. This specific type of mutation is expressed in a deadly form of metastatic non-small lung cancer. It is the first approval for NGS and liquid biopsy in one diagnostic test.
NGS is a DNA-sequencing technique which can sequence the entire human genome in a day. According to a review of NGS platforms and applications, “each of the three billion bases in the human genome is sequenced multiple times, providing high depth to deliver accurate data and an insight into unexpected DNA variation”. In the context of companion diagnostics, NGS is used for high-throughput tumour profiling. In one test, NGS allowed clinicians to detect mutations in 55 tumorous genes, instead of assessing one gene at a time.
In addition to utilising NGS, the Guardant360 CDx assay also uses liquid biopsy. In comparison to solid biopsies, the procedure is less invasive for patients and can also be repeated easily, which could have a considerable number of clinical applications.
It appears that companion diagnostics are diversifying. In addition to their application in matching therapy to patients, they are becoming increasingly used to identify the presence of residual disease in order to intervene with treatment before it is incurable. This was a point raised in the 2020 Nature article, in which the author states that “during treatment, regular liquid biopsies could reveal the persistence or increase of CTCs or ctDNA — which would indicate resistance to the chosen therapy. People could then be offered a more effective treatment before the tumour burden becomes excessive and incurable”.
Charlotte Di Salvo, Lead Medical Writer
PharmaFeatures
Subscribe
to get our
LATEST NEWS
Related Posts

Immunology & Oncology
Forging a Hopeful Outlook on Cancer Drug Development
The core of oncotherapy is still about reducing human suffering and facing the many challenges of this disease together.

Immunology & Oncology
Patterns, Profiles, and Patient Outcomes: AI in Oncotherapeutics
AI presents a beacon of hope in revolutionizing cancer management across various stages.
Read More Articles
Synthetic Chemistry’s Potential in Deciphering Antimicrobial Peptides
The saga of antimicrobial peptides unfolds as a testament to scientific ingenuity and therapeutic resilience.