CAR-T therapy represents the next exciting step for immunotherapy to address many unmet clinical challenges in cancer research. From aggressive cancer types with poor prognosis, to high relapse rates – many patients fail to access effective treatment. The latest innovations in CAR-T therapy methods demonstrate the importance of precision treatment, and offer hope for refractory patients and potentially rare cancer types.
Introduction
Adoptive T cell (ACT) therapy is a type of cancer immunotherapy which uses the specificity of T cells, to selectively target tumour antigens. Initially, tumour-specific T samples are harvested from resected tumours, to which the sample is expanded via in-vitro methods.
This original method of ACT was relatively limited, as not all tumours could be targeted. This method is typically dependent on location – meaning that many patients were not eligible for this type of therapy. However, expansions in genetic engineering technology have seen ACT develop into a number of options for many cancer types. The two main methods which fall under ACT in oncology are chimeric antigen receptor (CAR-T) therapy and T cell receptor (TCR) therapy.
CAR-T cell therapy allows the production of T cells that can target almost any naturally occurring protein structure on any cell. T cells are engineered to express a chimeric antigen receptor (CAR), a type of receptor protein that can recognise and bind to specific antigens on cancer cells.
To avoid damaging healthy tissue, which could cause detrimental consequences, the specificity of the target tumour antigens is crucial to ensure T cell-driven mechanisms occur only in the cancer cells. Viral-based vectors are the main method of producing CAR-T cells in the transferring of genetic information.
Lentiviral vectors specifically, are a popular choice due to their ability to “target nondividing cells with relative ease, whereas in gamma retroviral vectors, the transduction rates into nondividing cells are significantly lower.” Non-viral vectors are emerging as a popular alternative to viral vectors, which continue to pose a risk for oncogenic mutation.
Despite ongoing challenges (like the risk of Cytokine release syndrome), CAR-T has shown significant success across a number of clinical trials over recent years. Developing a safe, effective method of immunotherapy which can be tailored to a specific tumor profile, is of paramount importance to support the development of precision therapeutics.
Kite receives FDA approval for CAR-T therapy for adult leukaemia
On October 1 2021, the FDA approved Kite Pharma’s Tecartus as the first and only CAR-T therapy for adults with relapsed, or refractory B-cell precursor acute lymphoblastic leukaemia (ALL). This represents a significant breakthrough as it is the first CAR-T therapy available for an entirely new group of patients.
The therapy was approved by the regulator for the new indication, following a review of the ZUMA-3 trial. The data demonstrated that 65% of patients treated with Tecartus went into remission from the cancer present.
The biotech company emphasised the importance of addressing the high number of relapsing patients in this age category – which is 18 years and older. Rival therapy Kymriah, developed by Novartis, is also approved to treat this indication, but only for patients up to the age of 25 (however, it has been noted that this age group accounts for the majority of ALL cases).
In a recent press release, CEO of Kite Pharma Christi Shaw said “Today marks Kite’s fourth FDA approved indication in cell therapy in under four years, demonstrating our commitment to advancing CAR T for patients across many different hematologic malignancies. Tecartus has already transformed outcomes for adults living with mantle cell lymphoma, and we look forward to offering the hope for a cure to patients with ALL.”
This is a huge step forwards for addressing the wide variety of unmet clinical needs, across the spectrum of cancer types. Up until now, older patients with ALL were unable to access a therapy which could offer long-term remission, other than a stem cell transplant. This was a significant issue, especially so because as much as half of this patient population will relapse, and the median overall survival is only approximately eight months with current standard treatment of care.
The approval of tecartus has demonstrated the benefits of CAR-T therapy across a huge age range for a specific indication. It allows a greater number of patients to seek precision treatment which will not only be more effective in terms of reducing the chance of remission, but for overall survival.
Gel enhances CAR-T immunotherapy benefits in brains surgically treated for glioblastoma
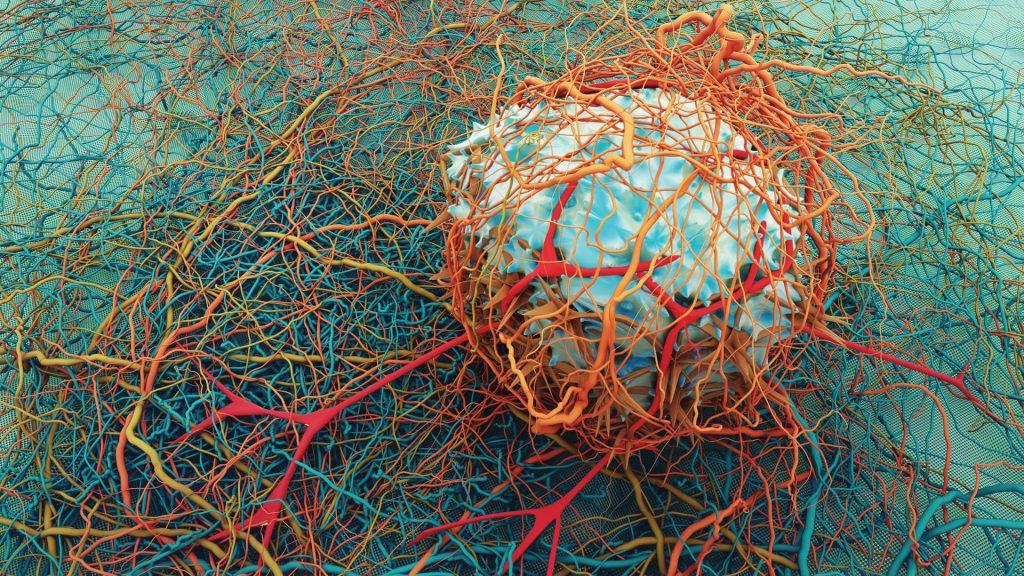
Gliomas refers to tumour formation originating from glial cells of the central nervous system (CNS). Glial cells are non-neuronal cells present in the CNS and peripheral nervous system (PNS) which act to support and protect neurons.
Glioblastoma (GBM) is a grade IV glioma subtype and accounts for almost half of all primary malignant brain tumours. According to National Brain Tumor Society, the five-year survival rate for glioblastoma patients is only 6.8%, and the average length of survival for glioblastoma patients is estimated to be only 12 to 18 months.
The key takeaway is that the survival rates and mortality statistics for these aggressive brain tumours, which accounts for a huge proportion of brain tumour cases, have remained virtually unchanged for decades. This represents a significant unmet clinical need for effective treatment options and focus on drug development.
CAR-T therapy has demonstrated success for many cancer indications, and has been under investigation for its efficacy against the highly malignant and deadly cancer glioblastoma.
It was reported recently, that researchers and colleagues from the University of North Carolina Lineberger Comprehensive Cancer Center, found that the pairing of a newly developed fibrin gel with CAR-T therapy, showed an improvement in the immunotherapy’s effectiveness in rodent glioblastoma. Fibrin is a protein most often found associated with supporting blood clot development.
The treatment was delivered to post-surgical mouse brains, to which it was observed that “the gel aided CAR-T cell distribution in the brain by acclimating the T cells to the post-surgical wound environment while also stopping the tumor from recurring.”
It was found that “nine of 14 (64%) mice that received the gel and T cells were tumor free 94 days after treatment, compared to two of 10 (20%) mice who only received T cells.”
This is an important step forward in developing an effective treatment for aggressive cancer types like glioblastoma, where approximately 40 percent of patients live for only one year after diagnosis. While surgery is an option, it can cause a number of serious complications given the location of the tumour, during resection and in the recovery period.
Charlotte Di Salvo, Editor & Lead Medical Writer
PharmaFeatures
Subscribe
to get our
LATEST NEWS
Related Posts

Immunology & Oncology
Forging a Hopeful Outlook on Cancer Drug Development
The core of oncotherapy is still about reducing human suffering and facing the many challenges of this disease together.

Immunology & Oncology
Patterns, Profiles, and Patient Outcomes: AI in Oncotherapeutics
AI presents a beacon of hope in revolutionizing cancer management across various stages.
Read More Articles
Synthetic Chemistry’s Potential in Deciphering Antimicrobial Peptides
The saga of antimicrobial peptides unfolds as a testament to scientific ingenuity and therapeutic resilience.