Ulcerative colitis is a chronic inflammatory disease that affects the large intestine, causing symptoms such as diarrhea, bleeding, and urgency. Current treatment options for this condition are limited, leaving many patients with inadequate responses or intolerances to available therapies. However, there is hope on the horizon as Eli Lilly and Company recently announced that their drug, mirikizumab (OMVOH ®), has received marketing authorization from the Medicines and Healthcare products Regulatory Agency (MHRA) in Great Britain for the treatment of eligible adults with moderately to severely active ulcerative colitis.
UC & mAbs: Immune Response and Immunobiologics
Ulcerative colitis (UC) is a chronic inflammatory bowel disease that primarily affects the colon and rectum. The exact cause of UC is not yet fully understood, but it is believed to result from an abnormal immune response in genetically susceptible individuals triggered by environmental factors.
The pathophysiology of UC involves an exaggerated immune response in the gastrointestinal tract, leading to chronic inflammation and damage to the intestinal lining. The immune system mistakenly recognizes harmless substances, such as food or normal gut bacteria, as threats and initiates an immune response. This immune response involves the activation of various immune cells, including T cells and inflammatory cytokines.
In UC, the intestinal epithelium becomes compromised, allowing the entry of luminal antigens and bacteria. This breach in the epithelial barrier triggers an immune response, leading to the recruitment of immune cells to the affected area. The immune cells release pro-inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), and interleukin-23 (IL-23), which further perpetuate the inflammatory response. This chronic inflammation results in the characteristic symptoms of UC, including diarrhea, rectal bleeding, abdominal pain, and urgency.
Monoclonal antibodies (mAbs) have revolutionized the management of UC by specifically targeting key molecules involved in the inflammatory cascade. These biologic therapies offer a targeted approach to modulating the immune response and reducing inflammation.
One class of mAbs used in UC management targets TNF-α, a pro-inflammatory cytokine that plays a crucial role in the pathogenesis of UC. Anti-TNF mAbs, such as infliximab, adalimumab, and golimumab, bind to TNF-α and inhibit its activity, thereby reducing inflammation and improving symptoms in patients with moderate to severe UC.
Another class of mAbs targets IL-12 and IL-23, cytokines involved in the activation of T cells and the production of other inflammatory mediators. By blocking these cytokines, IL-12/23 inhibitors, such as ustekinumab and mirikizumab, help modulate the immune response and reduce inflammation in UC.
These monoclonal antibodies are typically administered via intravenous infusion or subcutaneous injection and are used in patients who have had an inadequate response or intolerance to conventional therapies, such as corticosteroids or immunomodulators.
The use of mAbs in UC management has shown significant efficacy in inducing and maintaining remission, reducing the need for corticosteroids, and improving patients’ quality of life. However, it’s important to note that these biologic therapies may have potential side effects, including increased susceptibility to infections and infusion reactions. Close monitoring and regular follow-up with healthcare providers are necessary to ensure optimal management and safety.
Monoclonal antibodies have emerged as a valuable treatment option for ulcerative colitis. By specifically targeting key molecules involved in the inflammatory response, these biologic therapies offer a targeted approach to reducing inflammation and improving symptoms in patients with UC. Continued research and development in this field hold promise for further advancements in the management of this chronic inflammatory bowel disease.
Mechanism of Action & Pharmacologic Effects
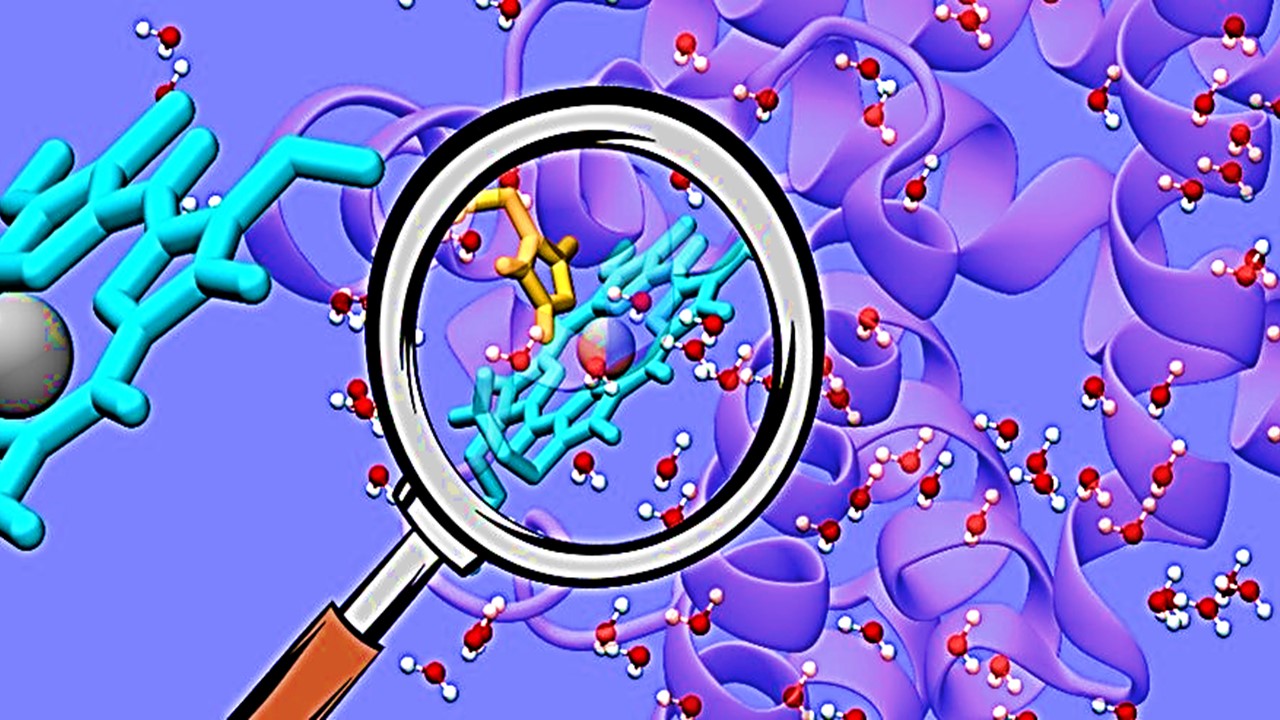
Anti-interleukin-23 (anti-IL-23) antibody mirikizumab is a humanized IgG4 monoclonal that binds specifically to the p19 subunit of the human IL-23 cytokine and prevents it from interacting with the IL-23 receptor. The differentiation, growth, and survival of T cell subsets (such as Th17 cells and Tc17 cells) and innate immune cell subsets, which serve as sources of effector cytokines like IL-17A, IL-17F, and IL-22 that promote inflammatory illness, are influenced by the regulatory cytokine IL-23. It has been demonstrated that in people, specific IL-23 inhibition restores normal production of these cytokines.
The phase 3 ulcerative colitis investigations examined inflammatory biomarkers. During induction dosage, mirikizumab delivered intravenously every four weeks dramatically decreased fecal calprotectin and C-reactive protein levels from baseline to week 12. Additionally, through 40 weeks of maintenance dose, mirikizumab delivered subcutaneously every 4 weeks maintained significantly lower levels of fecal calprotectin and C-reactive protein.
The Efficacy of Mirikizumab
Mirikizumab is the first IL-23p19 targeted biologic to demonstrate efficacy for both induction and maintenance therapy of moderately to severely active ulcerative colitis. This breakthrough was based on the positive results from two phase 3 clinical trials, LUCENT-1 and LUCENT-2. In these trials, mirikizumab not only achieved primary and key secondary endpoints but also demonstrated sustained clinical remission.
Induction Study: LUCENT-1
The LUCENT-1 study involved 1,162 patients who were randomly assigned to receive either mirikizumab (300 mg) intravenous (IV) or placebo IV every 4 weeks for 12 weeks. After 12 weeks of treatment, mirikizumab showed a significant improvement, with 24.2% of patients achieving clinical remission compared to only 13.3% in the placebo group.
Maintenance Study: LUCENT-2
Following the successful induction study, 544 patients who responded to mirikizumab in LUCENT-1 were re-randomized to receive either mirikizumab (200 mg) subcutaneous injection or placebo subcutaneous injection every 4 weeks for another 40 weeks in LUCENT-2. At one year, 49.9% of patients in the mirikizumab group achieved clinical remission, compared to 25.1% in the placebo group. Additionally, 43.3% of patients in the mirikizumab group achieved histologic-endoscopic mucosal remission, compared to 21.8% in the placebo group.
Early Improvement and Bowel Urgency
One of the remarkable findings in the LUCENT studies was the early improvement observed in patients treated with mirikizumab. As early as two weeks, these patients experienced a greater reduction in rectal bleeding and stool frequency subscores. Furthermore, mirikizumab demonstrated a significant decrease in bowel urgency severity, as measured by the validated Urgency Numeric Rating Scale. At one year, 42.9% of patients treated with mirikizumab achieved bowel urgency remission, compared to 25% in the placebo group.
Safety Profile
The safety profile of mirikizumab was evaluated during the LUCENT clinical program. The most frequently reported adverse reactions included upper respiratory tract infections, headache, rash, and injection site reactions. These side effects were generally mild to moderate in severity.
Pharmacokinetic Profile
When administered subcutaneously every 4 weeks, there was no obvious building up of serum mirikizumab levels over time.
After induction dose (300 mg given intravenously every 4 weeks), the mean (coefficient variation [CV%]) Cmax and area under the curve (AUC) were 99.7 (22.7) g/mL and 538 (34.4) gday/mL, respectively, in individuals with ulcerative colitis. Following a maintenance dosage of 200 mg by subcutaneous injection every four weeks, the mean (CV%) Cmax and AUC were 10.1 (52.1) g/mL and 160 (57.6) gday/mL, respectively.
Absorption. Peak serum concentrations were reached 2-3 days after subcutaneous administration with mirikizumab, with an estimated absolute bioavailability of 44%. The location of the injection site had no discernible impact on mirikizumab absorption.
Distribution. 4.83 L was the average distributional total volume.
Biotransformation or Metabolism. Mirikizumab, an IgG4 monoclonal antibody that has been humanized, is anticipated to undergo the same catabolic processes as endogenous IgGs to break down into amino acids and short peptides.
Elimination. For individuals with ulcerative colitis, the mean apparent clearance in the population pharmacokinetic analysis was 0.0229 L/hr, and the mean elimination half-life was practically 9.3 days. Mirikizumab’s clearance is found to be dose-independent.
Dose Proportionality. In patients with ulcerative colitis or in healthy volunteers, mirikizumab showed linear pharmacokinetics with a dosage-proportional rise in exposure across a dose range of 5 to 2 400 mg administered intravenously or over a dose range of 120 to 400 mg administered subcutaneously.
Improving the Future of Gastroenterology
The marketing authorization granted to mirikizumab by the MHRA for the treatment of adults with moderate to severe ulcerative colitis marks a significant scientific advance in the field. With its unique mechanism of action as an IL-23p19 inhibitor, mirikizumab offers new hope for eligible individuals living with this challenging disease. The positive results from the LUCENT trials, demonstrating efficacy in both induction and maintenance therapy, along with its favorable safety profile, make mirikizumab an important addition to the treatment landscape for ulcerative colitis. This breakthrough treatment provides a promising step forward in improving the lives of patients and is a testament to the commitment of researchers and medical professionals in the field of gastroenterology.
About Eli Lilly & Company
Eli Lilly and Company is a renowned American pharmaceutical company with a rich history and global presence. Founded in 1876 by Colonel Eli Lilly, a pharmaceutical chemist and war veteran, the company has its headquarters in Indianapolis, Indiana, and operates offices in 18 countries, reaching customers in approximately 125 countries worldwide.
Throughout its history, Lilly has made significant contributions to the pharmaceutical industry. Notable achievements include being the first company to mass-produce the polio vaccine developed by Jonas Salk and being a pioneer in the production of insulin. Lilly was among the first pharmaceutical companies to utilize recombinant DNA technology to manufacture human insulin, introducing groundbreaking medications such as Humulin, Humalog, and Basaglar, the first approved biosimilar insulin product in the United States.
While Lilly is recognized for a range of medications, including clinical depression drugs such as Prozac and Cymbalta, as well as antipsychotic medication Zyprexa, its primary revenue drivers are the diabetes drugs Humalog and Trulicity. The company’s commitment to innovation, research, and development has positioned it as a prominent player in the pharmaceutical industry.
Eli Lilly and Company’s contributions extend beyond its products and commercial success. The company has been a significant philanthropic force, holding the distinction of being the largest corporation and charitable benefactor in Indiana in 1997. Its commitment to corporate social responsibility and employee welfare has earned Lilly a place on the Forbes list of America’s Best Employers.
As a full member of the Pharmaceutical Research and Manufacturers of America and the European Federation of Pharmaceutical Industries and Associations, Lilly is an active participant in shaping the future of the pharmaceutical landscape. With its global reach, commitment to innovation, and dedication to improving healthcare, Eli Lilly and Company continues to make a lasting impact in the field of medicine.
Learn more at www.lilly.com.
About the MHRA
The Medicines and Healthcare products Regulatory Agency (MHRA) is a subsidiary of the Department of Health and Social Care in the United Kingdom, tasked with the crucial responsibility of ensuring the efficacy and safety of medicines and medical devices.
Established in 2003 through the merger of the Medicines Control Agency (MCA) and the Medical Devices Agency (MDA), the MHRA plays a vital role in safeguarding public health. In April 2013, the agency further expanded its scope by incorporating the National Institute for Biological Standards and Control (NIBSC), solidifying its position as a comprehensive regulatory authority. While the MHRA serves as the regulatory center within the group, its operations span across multiple locations, including London, York, and South Mimms, Hertfordshire, employing a dedicated workforce of over 1,200 individuals.
With its expert staff and comprehensive regulatory framework, the MHRA diligently assesses the efficacy, safety, and quality of medicines and medical devices in the UK. This scrutiny ensures that these products meet the necessary standards and are suitable for use by healthcare professionals and the general public alike. By maintaining robust regulatory oversight, the MHRA fosters public confidence in the healthcare sector and supports the government’s commitment to providing safe and effective treatments and devices for the people of the United Kingdom.
Learn more from gov.uk/government/organisations/medicines-and-healthcare-products-regulatory-agency.
Subscribe
to get our
LATEST NEWS
Related Posts

Regulatory Affairs
Navigating the Depths of Drug Approval: The FDA’s Crucial Role in Clinical Trials
In the realm of pharmaceuticals, ensuring the safety and efficacy of drugs is paramount.

Regulatory Affairs
Decoding Drug Prices: Unraveling the Intricate Puzzle of Pharmaceutical Pricing
Only by untangling the web of pharmaceutical pricing can we pave the way for a more affordable and equitable healthcare system.
Read More Articles
Synthetic Chemistry’s Potential in Deciphering Antimicrobial Peptides
The saga of antimicrobial peptides unfolds as a testament to scientific ingenuity and therapeutic resilience.