The General Practice Data for Planning and Research (GPDPR) is a proposed central NHS digital database collating patient data from GP records in England. Originally 1 July 2021, the date for launch has been pushed back to 1 September after the NHS called for a delay to allow patients to learn more about the system and consent regulations.
Introduction
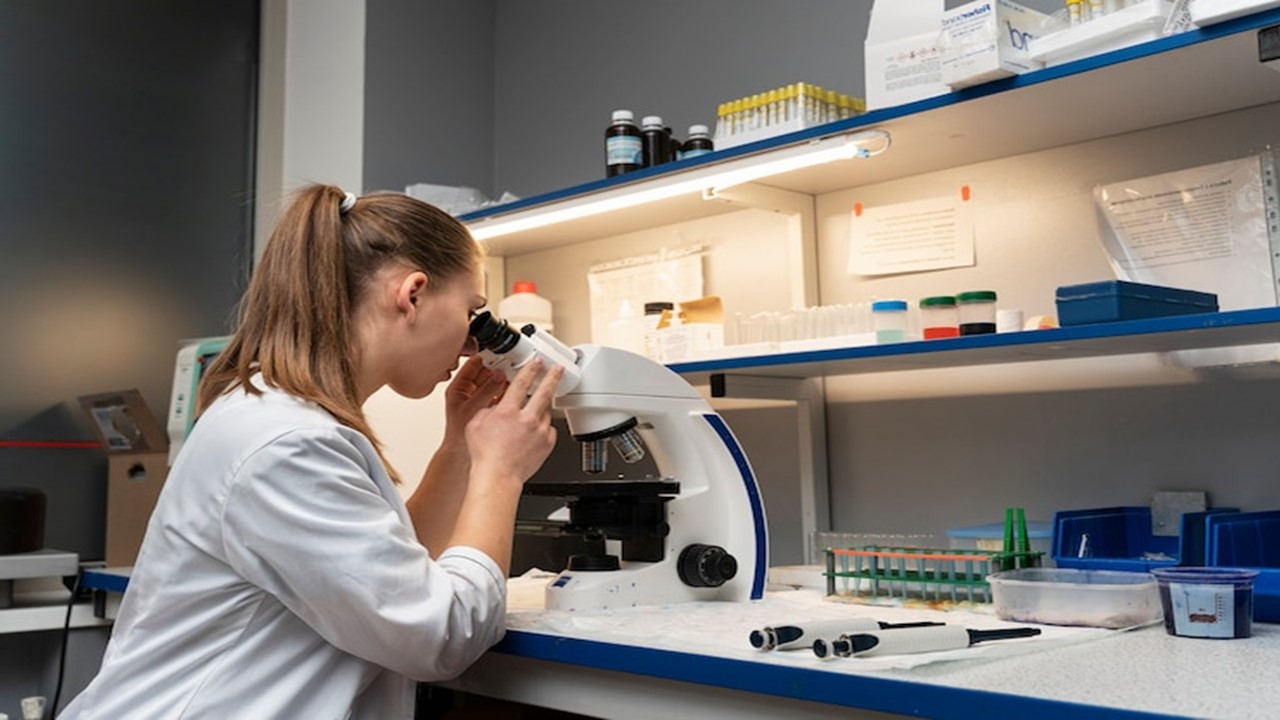
The system is based on the collection of data from GP practices “so that it can be used for health and social care purposes including policy, planning, commissioning, public health and research”.
According to the BBC the collected data will include sex, ethnicity, sexual orientation, diagnoses, medications and information about a patients’ physical, mental and sexual health.
Patient data collection from GPs is needed to support everything from scientific research to healthcare settings and services. One example is analysis of national medical data which can often reveal trends within certain populations, linking specific diseases to gender/ethnicity and other factors. This links with one of the areas the government hopes to utilise GPDPR for, specifically researching the long-term health impact of COVID-19 on the population.
Another target for the system is analysing data for healthcare inequalities. For example, understanding “how people of different ethnicities access healthcare and how the outcomes of particular groups compare to the rest of the population”.
Research and development is another area which the NHS digital platform aims to support. For example, analysis of data from cancer patients may reveal a trend between type and family history, which is useful in directing genomic cancer research.
For this digital database, NHS digital will not collect names, addresses, written notes, documents, and coded data that GPs are not permitted to share by law (e.g. IVF).
Concerns regarding implementation
Despite assurance from the government regarding data use, there are obvious concerns surrounding data privacy and security.
Firstly, many patients do not wish for sensitive data like mental illness or sexual orientation to be shared outside of the appropriate practices. Fears about employment implication and social stigma are a few of the concerns with the sharing of such data. The Guardian commented on this particular point inferring that the identification of individuals from medical records is still feasible even with limited data.
Secondly, there are a number of concerns regarding data security due to the concept of a centralised datastore. In comparison to systems spread out over a number of platforms, a central datastore is more vulnerable to cyber attacks. The obvious impact of this is potential sharing of data with third parties for profit.
Recent applications of healthcare data
Identifying disparities in care
According to the BBC, GP data has been used to identify disparities in care for individuals with learning disabilities. This is an example of the positive impact analysing healthcare data can have for tackling inequality in healthcare settings.
A 2016 public health report details the findings of GP data collection from this patient population, and the potential impact it could have with regards to improving access to healthcare.
Based on estimates from collected data, the report suggested that “only 23% of adults with learning disabilities in England are identified as such on GP registers, the most comprehensive identification source within health or social services in England. The remaining 77% have been referred to as the ‘hidden majority’ of adults with learning disabilities who typically remain invisible in data collections used in this publication”.
Furthermore, in comparison to “expected death rates in the general population, there were 2.8 times the expected number of deaths from circulatory diseases and 4.9 times the number of deaths from respiratory diseases in individuals with learning difficulties”. Preventable deaths like epilepsy also contributed to 3.9% of the death statistics.
It highlights an obvious flaw in the healthcare system, whereby vulnerable populations are not receiving the appropriate care and attention they require. Without collection and analysis of GP data, it would not only be harder to be aware of the inequalities but it also supports governing bodies in addressing these challenges.
COVID-19
More recently, healthcare data has proven to be a useful tool in the fight against COVID-19. The University of Oxford RECOVERY clinical trial uses patient data to “identify treatments that may be beneficial for people hospitalised with suspected or confirmed COVID-19”.
During this trial, a range of potential treatments including corticosteroids were tested for improvement in the condition of patients hospitalised with the virus. The results from this trial, i.e. patient data, are continuously collected, analysed and compared against each other to assess the success of each treatment type.
In addition to drug efficacy, data analysis may reveal whether a specific form of treatment is potentially more beneficial for certain ethnic groups of patients with specific pre-existing health conditions.
Patient data is also important in this context in terms of identifying whether specific sub-groups of the population are more likely to be hospitalised from COVID-19. A 2021 study recently revealed how COVID-19 has disproportionately affected minority ethnic populations in the UK.
The observational cohort study analysed the electronic health records of adults registered with primary care practices “for whom electronic health records were available through the OpenSAFELY platform”.
In general, the results highlighted that minority ethnic groups in the UK have had disproportionately high levels of poor COVID-19 outcomes. This focused on the risk of COVID-19-related hospitalisation, ICU admission, and death after accounting for clinical comorbidities in England.
Capturing healthcare data seen for this study has enabled healthcare professionals to gain real-time insights into the ethnic disparities across different severities of COVID-19 infection. This data is an important part of improving the quality of, and access to, care for minority ethnic groups across England and the UK in general.
While the aforementioned studies support the collection of medical data, it is important to take into account patient concerns regarding the upcoming ‘NHS data grab’ with regards to cybersecurity, data protection, and data privacy. Addressing these concerns remains an important part of this shift in healthcare data use, and further engagement with the public about this is another area for improvement.
Charlotte Di Salvo, Lead Medical Writer
PharmaFeatures
Subscribe
to get our
LATEST NEWS
Related Posts

Clinical Operations
Supervised Learning: Harnessing Data to Revolutionize Patient Care
As healthcare enters a new era, the integration of ML promises to revolutionize oncology and medicine.

Bioinformatics & Multiomics
Harnessing Computational Ingenuity for Tomorrow’s Therapeutics
Leverage computational power to navigate modern drug design.
Read More Articles
Synthetic Chemistry’s Potential in Deciphering Antimicrobial Peptides
The saga of antimicrobial peptides unfolds as a testament to scientific ingenuity and therapeutic resilience.