In the fast-evolving landscape of modern healthcare, the role of health information technology (HIT) has become increasingly pivotal. This technology spans a spectrum of applications, from the basic electronic charting to sophisticated decision support systems and integration with medical devices. The integration of HIT has opened up a multitude of avenues for transforming healthcare, with the promise of reduced human errors, enhanced clinical outcomes, efficient care coordination, improved practice efficiencies, and the ability to track data over time. As the realm of HIT continues to expand, it becomes vital to explore the evidence-based impact of these technologies on patient safety.
Medication Safety and Computerized Physician Order Entry (CPOE)
One of the cornerstones of health information technology is Computerized Physician Order Entry (CPOE). This system involves the use of electronic or computer-based platforms for entering physician orders, including medication orders. Initially designed to enhance the safety of medication orders, CPOE systems have evolved to facilitate electronic ordering of tests, procedures, and consultations. Crucially, they are integrated with Clinical Decision Support (CDS) systems, which serve as a protective shield against medication errors by guiding prescribers on preferred drug doses, routes, and frequencies, considering patient allergies, drug interactions, and clinical guidelines.
A meta-analysis investigating the effectiveness of CPOE with CDS found significant reductions in medication errors and adverse drug reactions in hospitals. However, the use of “hard stops” to prevent errors resulted in treatment delays. Notably, stand-alone CPOE systems, devoid of CDS, did not demonstrate a reduction in medication errors, underscoring the importance of this combined approach.
Clinical Decision Support: Guiding the Way
Clinical Decision Support (CDS) systems provide healthcare professionals with patient-specific information to enhance their decision-making process. These systems encompass an array of tools, including notifications, alerts, clinical guidelines, and patient-specific clinical summaries. Research has shown that on-screen reminders for physicians lead to improvements in process adherence, medication ordering, vaccination, laboratory ordering, and clinical outcomes. However, physicians often tend to overlook these alerts.
Successful CDS systems tend to be those that demand justification for overriding recommendations and provide advice simultaneously to patients and practitioners. Moreover, systems developed by the healthcare provider have a higher likelihood of success. Nevertheless, it’s crucial to acknowledge that the efficacy of CDS systems can vary based on design and implementation methods.
Enhancing Hand-Offs with Electronic Sign-Out Tools
The seamless transition of patient care from one healthcare provider to another, often termed “hand-offs,” is a crucial aspect of healthcare delivery. Ensuring effective communication during these transitions is paramount to maintaining patient care continuity and safety. Electronic sign-out applications have emerged as valuable tools in this context, offering structured methods for transferring vital patient information. Research findings by Davis, et al. and Li, et al. indicate that these digital solutions hold the potential to enhance the handover process significantly. They not only help reduce the risk of omitting critical patient information but also minimize the time required for these transitions. However, it’s essential to note that while the existing research provides promising insights into the benefits of electronic sign-out applications, the quality of these studies warrants further examination. As healthcare systems increasingly integrate technology into patient hand-offs, a more in-depth investigation is necessary to comprehensively understand the extent of their impact on patient safety and care continuity.
Barcode Medication Administration: A Promising Safeguard
Barcode Medication Administration (BCMA) systems represent a promising frontier in the quest to enhance medication safety within healthcare settings. By marrying electronic medication administration records with barcode technology, BCMA aims to ensure that the precise patient receives the correct medication at the designated time. Observational studies by Leung, et al. and Khammarnia, et al. have offered compelling evidence that BCMA systems contribute to a substantial reduction in medication errors, thus underscoring their potential to revolutionize medication administration. Nevertheless, the field is marked by varying outcomes across different studies, indicating a need for more extensive and rigorous investigations. Moreover, the impact of BCMA in pediatric and outpatient healthcare environments remains a relatively uncharted territory, leaving room for future research to ascertain the breadth of its effectiveness and adaptability to diverse clinical settings.
Smart Pumps and Medication Safety
Smart pumps, integrated with advanced medication error-prevention software, play a critical role in enhancing medication safety within healthcare settings. These smart devices are designed to actively alert operators when the infusion settings deviate from predefined safety limits, acting as a safeguard against potential medication errors. However, the effectiveness of these smart pumps is a subject of ongoing debate. In a randomized controlled trial aimed at assessing their impact, the results were inconclusive. One contributing factor to this uncertainty was the inadequate compliance of healthcare providers with the system. This suggests that the full potential of smart pumps may not be realized unless there is greater alignment between technology and clinical practice. Nonetheless, a systematic review offered a glimmer of hope, indicating that these pumps may indeed reduce programming errors, especially when strict “hard limits” are enforced, emphasizing the importance of integrating these devices into clinical workflows with due diligence and care to maximize their efficacy in medication safety.
Smart pumps, with their medication error-prevention capabilities, indubitably hold promise in minimizing medication-related mistakes. However, their full potential remains contingent on improved provider compliance and the implementation of rigorous safety protocols, including the enforcement of hard limits, to ensure they effectively contribute to the overarching goal of patient safety.
Automated Medication Dispensing Cabinets: A Critical Care Innovation
Automated dispensing cabinets (ADCs) represent a significant advancement in healthcare technology, primarily designed to optimize medication distribution and inventory management, particularly in the demanding environment of critical care settings. These high-tech cabinets offer a structured and automated approach to medication management, significantly reducing the likelihood of medication preparation errors. Within critical care units, where precision and speed are paramount, ADCs have been shown to effectively minimize errors associated with medication preparation, leading to enhanced patient safety and care quality. Having been afforded these advantages, it is still essential to acknowledge that the available evidence largely revolves around the critical care context. The potential of ADCs in other healthcare settings, where medication distribution and inventory management complexities may differ, remains largely unexplored, highlighting the need for further research to assess their broader impact on medication safety and error reduction across diverse healthcare environments.
Preventing Retained Surgical Items: The Role of Technology
The integration of technology, such as barcoding and radiofrequency tagging of surgical items, presents a promising avenue for the prevention of retained surgical items, a potentially life-threatening medical error. These advanced systems aim to enhance the tracking and accountability of surgical instruments and sponges, thereby reducing the risk of leaving items behind in a patient’s body after surgery. Nevertheless, despite the considerable potential of these technologies, existing studies by Hempel, et al.and Shekelle, et al. have yielded inconclusive results. This inconclusiveness underscores the imperative need for further comprehensive research to robustly evaluate the efficacy and safety of these innovative tools.
Patient Electronic Portals: Empowering Patients
Patient portals represent a crucial facet of modern healthcare by granting individuals secure access to their personal health information and fostering direct electronic communication with their care providers. These portals have shown their mettle in enhancing preventive care and empowering patients to self-manage their health conditions more effectively. Patients can access their medical records, review test results, and even schedule appointments with ease, contributing to a more proactive and informed approach to their healthcare. Additionally from the studies done by Nagykaldi, et al., Fiks, et al., and Kruse, et al., the convenience of electronic communication facilitates discussions with healthcare providers, enabling timely inquiries and clarifications regarding health concerns. However, the impact of patient portals on patient safety outcomes remains a topic of ongoing research and debate. While they undeniably empower patients, their influence on safety metrics, such as reducing medical errors or adverse events, is less clear. Further studies are essential to ascertain the precise relationship between patient portal usage and patient safety, ensuring that these promising tools evolve in ways that bolster overall healthcare quality while safeguarding patients.
Telemedicine: Bridging Gaps in Healthcare
Telemedicine is emerging as a transformative force in healthcare, with virtual visits and remote patient monitoring at the forefront of this revolution. Research suggests that virtual visits can deliver clinical outcomes on par with traditional face-to-face care, emphasizing their potential to expand access and convenience for patients. However, the impact of telemedicine on patient safety remains a subject for ongoing investigation, as the unique challenges and opportunities presented by virtual care are not yet fully understood. Additionally, e-consultations, a component of telemedicine, have shown promise in reducing patient wait times for specialist appointments. Yet, their efficacy and safety profile also require further scrutiny, highlighting the need for rigorous studies to unlock the full potential of telemedicine in ensuring both accessibility and patient safety within the evolving healthcare landscape.
Electronic Incident Reporting: The Path to Improvement
Electronic incident reporting systems serve as invaluable tools in healthcare, streamlining the process of reporting incidents and standardizing workflows. These systems enable the rapid identification of incidents, a crucial step towards addressing and rectifying potential safety issues within clinical settings. By providing a structured framework for reporting, they help ensure that critical information is captured, documented, and shared efficiently among healthcare professionals.
However, it’s important to note that while these systems enhance the frequency and consistency of incident reporting, the evidence supporting their direct impact on reducing medical errors is still limited. The focus has primarily been on improving the reporting process itself and not necessarily on the subsequent actions taken to prevent or mitigate errors. As healthcare organizations continue to embrace electronic incident reporting, it becomes imperative to not only refine reporting mechanisms but also to rigorously assess their effectiveness in driving substantial improvements in patient safety and clinical outcomes.
The Comprehensive Impact of Electronic Medical Records (EMR)
The widespread adoption of electronic medical records (EMR) has become a focal point in the healthcare industry, attracting substantial attention due to its potential to transform patient care. An array of research findings indicates that organizations embracing EMR systems benefit from improved adherence to clinical guidelines, a tangible reduction in medication errors, and fewer adverse drug reactions. These digital repositories streamline healthcare data, making it readily accessible and facilitating better coordination among healthcare providers, ultimately enhancing the quality of care delivered to patients.
However, the introduction of EMR also unveils a complex and nuanced landscape in healthcare quality and safety. While the technology shows promise in enhancing patient safety, there are ongoing questions about the optimal ways to integrate EMR into various healthcare settings and ensure that its full potential is harnessed. Moreover, the implementation of EMR requires a careful balance between data security, usability, and clinical utility. Thus, the journey toward realizing the comprehensive benefits of EMR systems remains a subject of continual exploration, driving healthcare professionals and researchers to seek solutions that optimize patient safety and quality of care in the ever-evolving healthcare landscape.
As the evidence continues to accumulate, it’s clear that these technologies, when thoughtfully integrated into healthcare settings, hold the promise of a safer, more efficient, and patient-centered future. Further research and careful consideration are required to harness the full potential of these innovations for the benefit of all patients.
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Subscribe
to get our
LATEST NEWS
Related Posts

AI, Data & Technology
The Power of Unsupervised Learning in Healthcare
In healthcare’s dynamic landscape, the pursuit of deeper insights and precision interventions is paramount, where unsupervised learning emerges as a potent tool for revealing hidden data structures.

AI, Data & Technology
Unlocking Intelligence: A Journey through Machine Learning
ML stands as a cornerstone of technological advancement, permeating various facets of our daily lives.
Read More Articles
Synthetic Chemistry’s Potential in Deciphering Antimicrobial Peptides
The saga of antimicrobial peptides unfolds as a testament to scientific ingenuity and therapeutic resilience.
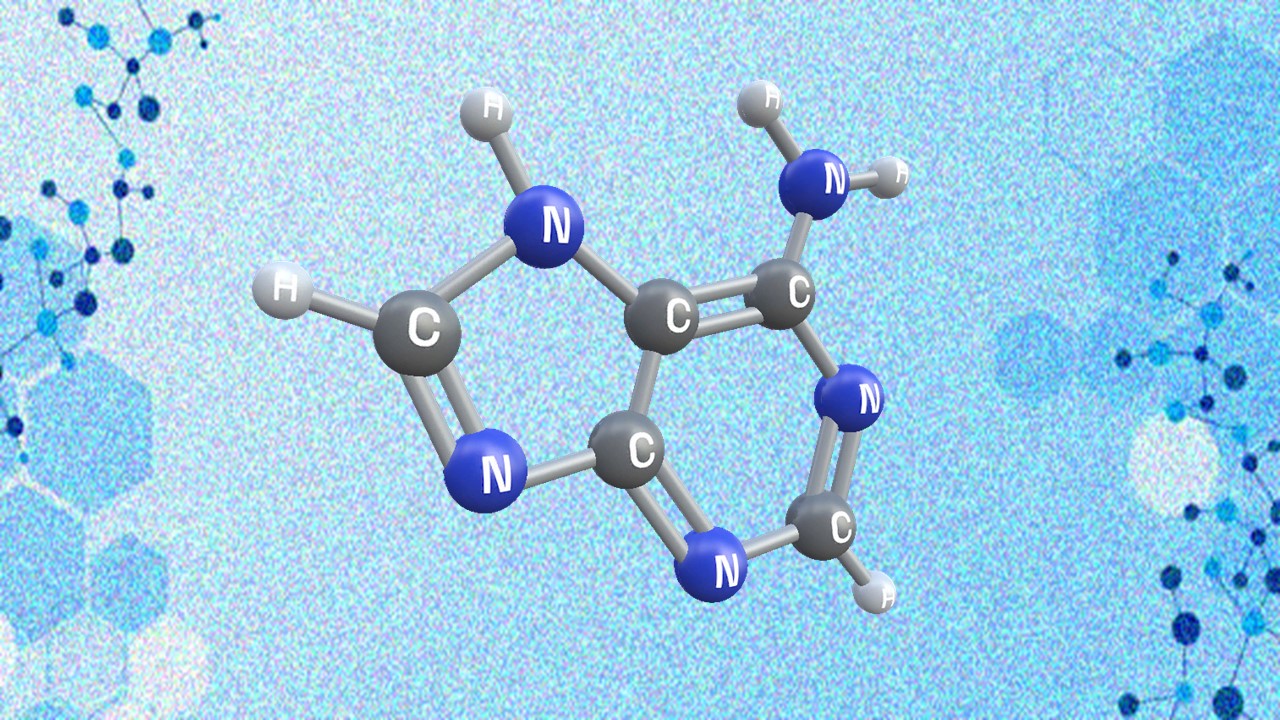
Appreciating the Therapeutic Versatility of the Adenine Scaffold: From Biological Signaling to Disease Treatment
Researchers are utilizing adenine analogs to create potent inhibitors and agonists, targeting vital cellular pathways from cancer to infectious diseases.