The term “heart disease” is used to describe a wide range of disorders that have an impact on the structure and function of the heart. Ischemic heart disease or coronary artery disease are other names for coronary heart disease (CHD). CHD is a form of cardiac disease in which the heart’s arteries are unable to supply the cardiac tissue with adequate oxygen-rich blood. According to the Centers for Disease Control and Prevention, coronary heart disease affects 18.2 million American adults, and it is the leading cause of death for those 65 and over. Some fatalities can happen gradually over the course of weeks to years as a result of the progressive weakening of the heart’s pumping mechanism, whilst other deaths take place immediately as a consequence of acute coronary occlusion or heart fibrillation.
Cardiac Syndrome X
The bigger coronary arteries on the surface of the heart are affected by coronary heart disease. The microscopic arteries in the heart muscle are affected by coronary microvascular illness, sometimes referred to as microvascular angina or cardiac syndrome X. Although the underlying etiology of microvascular angina is uncertain, endothelial dysfunction and decreased flow, perhaps as a result of spasm, in the tiny resistance blood arteries of the heart are thought to have a role. It is more difficult to identify and diagnose microvascular angina since it is not characterized by significant arterial obstructions. Women are more likely to have coronary microvascular disease.
Atherosclerosis
Atherosclerosis is a prominent culprit in decreased coronary perfusion. Succinctly, large amounts of cholesterol gradually accumulate beneath the endothelium at numerous locations in arteries all throughout body in individuals who have a genetic propensity for atherosclerosis, are overweight or obese and lead unhealthy lives, or have conditions such as high blood pressure and injury to the endothelial cells of the coronary vasculature. These deposit sites progressively become infiltrated by fibrous tissue and eventually calcify. Atherosclerotic plaques end up developing as a direct consequence, and when they do, they actually obstruct or partially obstruct blood flow by actually obtruding into the vessel lumens. The first few millimeters of the main coronary arteries are frequently where atherosclerotic plaques begin.
CHD-Associated Pain
The heart cannot normally be “felt,” however hypoxic cardiac muscle frequently creates a discomfort feeling that can be quite strong. Although the underlying cause of this pain is unknown, it is thought that ischemia causes the muscle to generate nociceptive substances like kinins, histamine, or cellular proteinases which cannot be cleared quickly enough through the low velocity coronary perfusion. These substances also include acidic components like lactic acid. The heart muscle’s pain nerve endings are then stimulated by the large doses of these aberrant metabolites, which causes pain impulses to go to the central nervous system via sensory afferent nerve fibers.
Angina Pectoris
As the strain on the heart exceeds the amount of coronary blood flow that is available, angina pectoris, a type of cardiac pain, starts to manifest in the majority of patients who have progressive narrowing of their coronary arteries. The phrase means “a strangling feeling in the chest” and is derived from the Latin words angere, “to strangle”, and pectus, “chest”. Above the heart, this ache is typically felt beneath the upper sternum. Also, the discomfort frequently refers to far-off portions of the body’s surface, typically the left arm and shoulder, but also occasionally the neck and even the sides of the face. The origin of the heart and the arms during embryonic life is in the neck, which explains why pain is distributed in this way. Thus, the same spinal cord segments supply pain nerve fibers to the heart and these body surfaces.
The majority of persons with chronic angina pectoris experience discomfort during exercise or when they are having emotional states that briefly constrict the coronary arteries or increase heart metabolism due to signals from sympathetic vasoconstrictor nerves. Having a full stomach or being chilly, which both increase the heart’s workload, can also make angina worse. Usually, the discomfort only lasts a short while. But in other people, the ischemia is so severe and pervasive that the discomfort never goes away. The patient often stops all unnecessary bodily activity because of the pain, which is generally described as intense, crushing, and immobilizing.
Summarized Pharmacologic Approach
When given during an acute anginal attack, a number of vasodilator medications can offer instant pain relief. Nitroglycerin and other nitrate medications are often used short-acting vasodilators. Treatment for chronic stable angina pectoris, also known as effort angina, may be aided by other medications that act on the cardiovascular system, such as angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, calcium channel blockers, and the persistent or late inward sodium current inhibitor ranolazine.
Beta blockers, including atenolol, metoprolol, and propranolol, are another class of medications used to treat angina pectoris for an extended period of time. By inhibiting sympathetic beta-adrenergic receptors, these medications stop the sympathetic stimulation of the heart rate and cardiac metabolism throughout physical activity or emotional crises. As a result, beta blocker medication reduces the heart’s need for supplemental metabolic oxygen under stressful circumstances. This treatment can, for precisely this reason, lessen both the frequency and the severity of anginal crises.
By thinning your blood and keeping it from clotting, blood thinners, such as clopidogrel, rivaroxaban, and low-dose aspirin, are a group of drugs that can help lower your risk of having a heart attack.
Statins, which reduce cholesterol, may be administered if you have high cholesterol. Statins, also referred to as 3-hydroxy-3-methyl-glutaryl-coenzyme A reductase inhibitors or just HMG-CoA reductase inhibitors, function by preventing the production of cholesterol and augmenting the number of low-density lipoprotein (LDL) receptors in the liver. This lessens the likelihood of a heart attack by assisting with the removal of LDL cholesterol from your bloodstream and into the hepatic organ.
Surgical Treatment of CHD
Interventional techniques or surgery may be required to open up or bypass clogged arteries if the blood vessels are narrow due to the buildup of atheroma (fatty deposits) or if the symptoms are uncontrollable by medication. The main methods for treating clogged arteries are listed below.
Aortic-Coronary Bypass Surgery
Many people with myocardial ischemia only have a few distinct spots where the coronary arteries are narrowed due to atherosclerotic disease, with the remaining coronary vessels being normal or almost normal. Aortic-coronary bypass surgery, also known as coronary artery bypass grafting (CABG), was developed in the 1960s. During this procedure, a section of a subcutaneous vein is detached from an arm or leg and grafted from the aorta to the edge of a peripheral coronary artery further than the atherosclerotic blockage point. It is typical to conduct one to five of these grafts, each of which provides a peripheral coronary artery past a block.
The majority of patients experience angina pain relief following coronary bypass surgery. Furthermore, in patients whose hearts had not already sustained too much damage prior to receiving the treatment, the coronary bypass surgery may give the patient a normal life expectancy. However, if the heart has already suffered significant harm, the bypass surgery may not be very beneficial.
Coronary Angioplasty
A technique has been utilized to unblock partially blocked coronary veins since the 1980s in order to prevent them from becoming completely occluded. The following is how the procedure known as coronary artery angioplasty is carried out. Under radiological guidance, a tiny balloon-tipped catheter with a diameter of about 1 millimeter is inserted into the coronary system and advanced into the partially occluded artery until the balloon section of the catheter crosses the partially occluded site. The problematic artery would then be noticeably stretched after the balloon has been inflated under high pressure. More than 75% of patients who undergo this procedure experience relief from the signs and symptoms of coronary ischemia for at least several years well after procedure, though many of the patients subsequently need coronary bypass surgery. After this procedure, the blood flow through the vessel frequently increases three to four times.
When a coronary artery has been dilated by angioplasty, little stainless steel mesh tubes known as stents are occasionally inserted into the artery to keep it open and avoid restenosis. The endothelium typically covers the metal surface of the stent after a few weeks that followed its implantation in the coronary artery, allowing blood to flow freely through it. Yet, between 25% and 40% of patients who receive angioplasty experience reclosure (restenosis) of the occluded coronary artery, typically within 6 months of the initial surgery. Restenosis generally results from an excessive amount of scar tissue under the replacement, healthy endothelium that has developed over the stent. Drug-eluting stents, which slowly release medications, could be able to stop excessive scar tissue formation.
The development of newer techniques for opening atherosclerotic coronary arteries is ongoing. In one of these techniques, a laser beam is directed towards the atherosclerotic lesion from the tip of a coronary artery catheter. Without seriously affecting the remaining artery wall, the laser practically dissolves the lesion.
Recovering From Effects of CHD
It is possible to return to a regular life after a heart attack, angioplasty, or heart surgery. You can get assistance in dealing with parts of your life that may have been impacted by coronary heart disease by asking for guidance and support.
A specialist of the cardiac rehabilitation team may stop by your hospital room after heart surgery to talk to you about your health and the operation you’re having. Usually, this care will continue even after you leave the hospital. A member of the cardiac care team may contact or visit you at home during the initial weeks following your operation to monitor your recovery.
Self-care is, in the end, the mother of all preventative medicine. Self-care is an essential component of daily living and entails taking charge of your health and wellness with the help of others who are responsible for your care. Self-care refers to the daily actions you do to look after your physical and mental health and stay active. Also, it enables you to avoid illnesses or accidents and treat small injuries and chronic problems more skillfully.
Supporting people with long-term diseases to develop self-care is extremely beneficial to them. People can have a higher quality of life, live longer, experience less pain, anxiety, sadness, and fatigue, and be more independent and productive.
In the end, whether one is genetically predisposed or not, the cliché catchphrase still stands the test of time – prevention is better, and obviously cheaper, than cure.
Subscribe
to get our
LATEST NEWS
Related Posts

Chronic & Debilitating Diseases
Renopathology Tipping Point: Deciphering the Molecular Code of Stage 2 Chronic Kidney Disease
The molecular events of Stage 2 CKD, from inflammation to lipid metabolism, offer insights for diagnosis and treatment.
Chronic & Debilitating Diseases
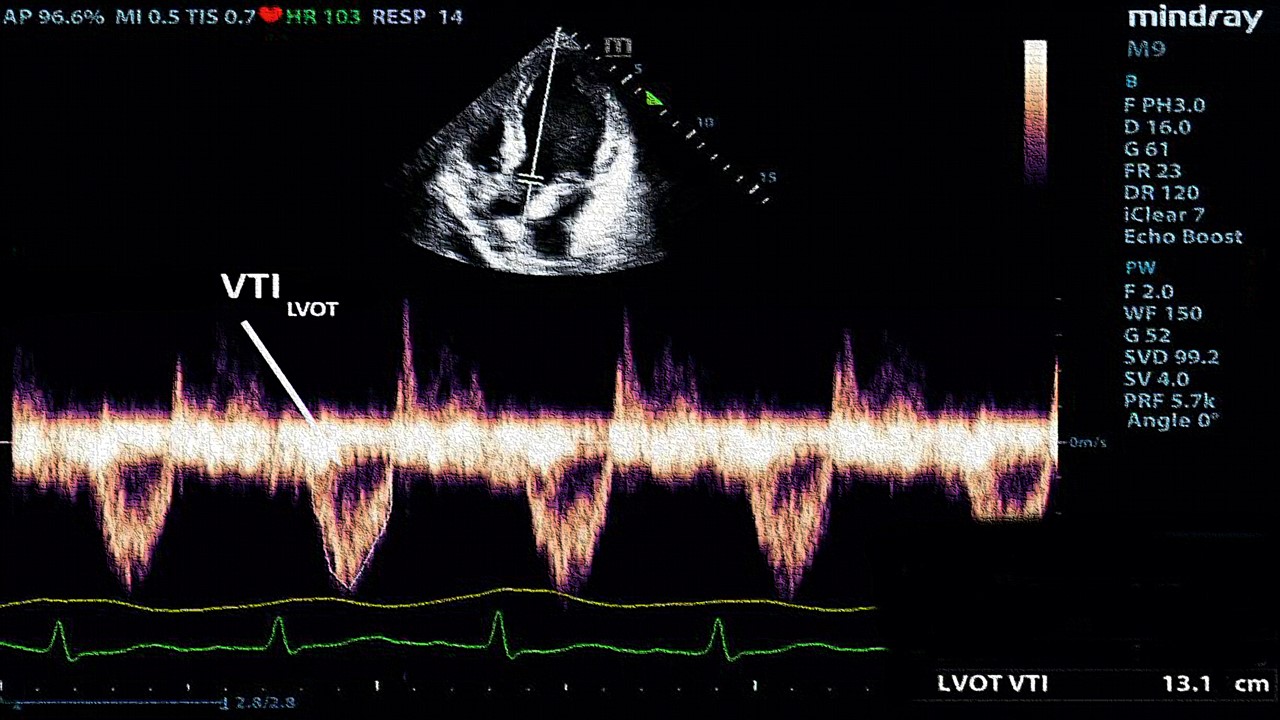
A New Lens on Shock: Hemodynamic Insights Through Critical Care Ultrasound
CCU has transformed the hemodynamic assessment of shock, delivering a reliable, reproducible, and non-invasive tool for ICU clinicians.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.
Designing Better Sugar Stoppers: Engineering Selective α-Glucosidase Inhibitors via Fragment-Based Dynamic Chemistry
One of the most pressing challenges in anti-diabetic therapy is reducing the unpleasant and often debilitating gastrointestinal side effects that accompany α-amylase inhibition.