In the intricate world of diabetes mellitus, the body’s ability to regulate blood glucose levels is disrupted, leading to significant health challenges. With different types and underlying mechanisms, understanding diabetes is crucial for effective management and prevention of complications. Let’s delve into the realms of Type 1 and Type 2 diabetes, as well as the severe condition known as diabetic ketoacidosis (DKA).
The Basics: Glucose Regulation and Hormonal Balance
Diabetes mellitus is a metabolic disorder characterized by impaired glucose metabolism. Glucose, a vital source of energy for cells, needs to be transported from the bloodstream into cells to fuel various physiological processes. However, in diabetes mellitus, this process is disrupted, leading to elevated blood glucose levels and inadequate glucose supply to the cells.
To maintain glucose homeostasis, the body relies on the coordinated actions of two key hormones: insulin and glucagon. These hormones play opposing roles in regulating blood glucose levels. Insulin, primarily secreted by beta cells located in the islets of Langerhans in the pancreas, functions to decrease blood glucose levels. It acts as a key that unlocks the cells, allowing glucose to enter.
When blood glucose levels rise, beta cells in the pancreas sense this increase and respond by releasing insulin into the bloodstream. Insulin then binds to specific receptors on the surface of target cells, such as muscle cells, adipose tissue cells, and liver cells. This binding triggers a cascade of intracellular events that facilitate the translocation of glucose transporters, such as GLUT4, from intracellular vesicles to the cell membrane. As a result, glucose transporters become embedded in the cell membrane, enabling glucose to enter the cells.
In contrast to insulin, glucagon, secreted by alpha cells in the islets of Langerhans, acts to increase blood glucose levels. Glucagon is released when blood glucose levels drop, such as during fasting or between meals. It stimulates processes in the liver, promoting the breakdown of stored glycogen (glycogenolysis) and the synthesis of glucose from non-carbohydrate sources, such as amino acids and fats (gluconeogenesis). These actions lead to an increase in blood glucose levels, ensuring a steady supply of glucose to the cells.
The islets of Langerhans, small clusters of hormone-secreting cells within the pancreas, are responsible for the production and regulation of insulin and glucagon. These islets contain beta cells, which secrete insulin, and alpha cells, which secrete glucagon. The tight coordination between these cells within the islets is essential for maintaining glucose balance in the body.
In diabetes mellitus, the dysfunction of either insulin or glucagon secretion, or the impaired response of target cells to these hormones, disrupts the delicate balance of glucose regulation. In Type 1 diabetes, the immune system mistakenly attacks and destroys beta cells, leading to a severe deficiency of insulin. In Type 2 diabetes, there is a combination of insulin resistance in target tissues and impaired insulin secretion by beta cells.
Type 1 Diabetes Mellitus: Unveiling Autoimmune Attack
Type 1 diabetes, also known as insulin-dependent diabetes mellitus (IDDM), is a chronic autoimmune disease characterized by a deficiency in insulin production. Insulin is a hormone produced by the beta cells located in the islets of Langerhans in the pancreas. It plays a crucial role in regulating blood glucose levels by facilitating the entry of glucose into cells.
In individuals with Type 1 diabetes, an autoimmune response occurs, wherein the immune system mistakenly identifies the body’s own beta cells as foreign and launches an attack on them. This loss of self-tolerance leads to the activation of T cells, a type of immune cell, which specifically targets the antigens present on the surface of beta cells.
The process begins with the activation of T cells that recognize beta-cell antigens as foreign or harmful. These activated T cells, along with other immune cells, initiate an inflammatory response and coordinate an attack on the beta cells in the islets of Langerhans. This immune-mediated destruction of beta cells is referred to as insulitis.
As the attack progresses, the number of functional beta cells gradually decreases, resulting in inadequate insulin production. With fewer beta cells available to produce insulin, the overall production and secretion of insulin decline significantly. Consequently, the insulin supply becomes insufficient to facilitate the movement of glucose from the bloodstream into cells.
The accumulation of glucose in the bloodstream, coupled with the reduced ability of cells to take up glucose, leads to persistently elevated blood glucose levels. This condition is known as hyperglycemia. Without sufficient insulin, glucose cannot enter cells to be utilized as a source of energy. Consequently, despite high glucose levels in the blood, the cells are deprived of the energy they require for normal functioning.
The hallmark symptoms of Type 1 diabetes include polydipsia (excessive thirst), polyuria (frequent urination), polyphagia (increased hunger), and unexplained weight loss. These symptoms arise as a result of the body’s compensatory mechanisms to access alternative energy sources, such as breaking down fat and muscle tissue, due to the lack of glucose uptake by cells.
The destruction of beta cells in Type 1 diabetes is often a progressive process. It can occur over a variable timeframe, with some individuals experiencing a rapid loss of beta cells, while others may have a more gradual decline. However, by the time clinical symptoms become apparent, a significant portion of the beta cells may already be destroyed.
The precise cause of the autoimmune response in Type 1 diabetes is not fully understood. It is likely to involve a complex interplay of genetic and environmental factors. Certain genetic predispositions, such as specific human leukocyte antigen (HLA) genes, increase the risk of developing Type 1 diabetes. However, additional triggers, such as viral infections, may be necessary to initiate the autoimmune process in genetically susceptible individuals.
Managing Type 1 diabetes primarily involves lifelong insulin therapy to replace deficient insulin production. Individuals with Type 1 diabetes require regular insulin injections or use insulin pumps to ensure adequate insulin levels in the body. Additionally, close monitoring of blood glucose levels, following a balanced diet, regular physical activity, and ongoing medical care are essential to maintain optimal blood glucose control and prevent complications associated with the disease.
Type 2 Diabetes Mellitus: A Battle with Insulin Resistance
Type 2 diabetes, also known as non-insulin dependent diabetes mellitus (NIDDM), is a metabolic disorder characterized by a combination of insulin resistance and inadequate insulin secretion. Unlike Type 1 diabetes, in Type 2 diabetes, the body still produces insulin, but the tissues, such as muscle, fat, and liver cells, exhibit reduced responsiveness to its effects, a condition known as insulin resistance.
Insulin resistance is a complex and multifactorial phenomenon with various underlying mechanisms. Both genetic and environmental factors contribute to the development of insulin resistance. One of the primary risk factors is obesity, particularly excess adipose tissue, which releases fatty acids and certain inflammatory molecules that interfere with insulin signaling pathways. Lack of physical activity and a sedentary lifestyle also contribute to the development of insulin resistance.
Additionally, other factors like genetic predisposition, hormonal imbalances, chronic inflammation, and certain medications can influence insulin resistance. Hypertension, high blood pressure, is also closely associated with insulin resistance, forming a part of a cluster of conditions called metabolic syndrome.
In response to insulin resistance, the pancreatic beta cells compensate by increasing insulin production and secretion. This initially helps maintain normal blood glucose levels. Beta cells undergo hyperplasia, which involves an increase in the number of beta cells, and hypertrophy, which refers to an enlargement of individual beta cells. These adaptive changes aim to meet the increased demand for insulin.
However, over time, the constant demand placed on beta cells can lead to their exhaustion and dysfunction. The beta cells become unable to maintain the increased insulin production, and insulin secretion may decline. As a result, blood glucose levels gradually rise, leading to hyperglycemia.
The elevated blood glucose levels characteristic of Type 2 diabetes can have adverse effects on various organs and tissues. Over time, persistent hyperglycemia can damage small blood vessels, leading to microvascular complications. This includes damage to the eyes (diabetic retinopathy), kidneys (diabetic nephropathy), and nerves (diabetic neuropathy).
Moreover, high blood glucose levels can also contribute to macrovascular complications, such as atherosclerosis, which increases the risk of cardiovascular diseases like heart attacks and strokes. The combination of hyperglycemia, insulin resistance, dyslipidemia, and hypertension can further promote the development of these cardiovascular complications.
The management of Type 2 diabetes involves lifestyle modifications and, in some cases, medication. Lifestyle changes include adopting a healthy diet, engaging in regular physical activity, achieving and maintaining a healthy weight, and controlling blood pressure and cholesterol levels. These measures aim to improve insulin sensitivity and reduce the demand on beta cells.
When lifestyle modifications alone are insufficient to control blood glucose levels, various medications may be prescribed. These medications work in different ways to improve insulin action, increase insulin secretion, or reduce glucose production in the liver. Some common classes of medications include metformin, sulfonylureas, thiazolidinediones, DPP-4 inhibitors, GLP-1 receptor agonists, and SGLT2 inhibitors.
Regular monitoring of blood glucose levels, as well as periodic assessment of kidney function, lipid levels, and blood pressure, is essential for effectively managing Type 2 diabetes. By maintaining optimal blood glucose control and addressing associated risk factors, individuals with Type 2 diabetes can reduce the risk of complications and improve their overall health outcomes.
Diabetic Ketoacidosis (DKA): A Dangerous Complication
Diabetic ketoacidosis (DKA) is a severe and potentially life-threatening complication that can occur in individuals with diabetes, particularly those with Type 1 diabetes. However, it can also occur in individuals with Type 2 diabetes under certain circumstances, although it is less common.
DKA typically develops when there is a profound deficiency of insulin in the body. Insulin is responsible for facilitating the uptake of glucose from the bloodstream into cells, where it is used as a source of energy. In the absence of sufficient insulin, the body’s cells cannot take up glucose effectively, resulting in high blood glucose levels (hyperglycemia).
In response to the lack of insulin, the body starts to break down stored fats for energy in a process called lipolysis. This breakdown of fats leads to the release of fatty acids into the bloodstream. The liver then converts these fatty acids into ketone bodies, including acetoacetic acid and beta-hydroxybutyric acid.
Under normal circumstances, ketone bodies are produced in small amounts and are readily utilized by the body’s tissues as an alternative source of energy. However, in DKA, the excessive production of ketone bodies overwhelms the body’s capacity to use them efficiently.
The accumulation of ketone bodies in the blood leads to an increase in blood acidity, a condition known as metabolic acidosis. This acidosis occurs because ketone bodies are acidic substances. As their levels rise, they disrupt the body’s acid-base balance, resulting in a decrease in blood pH.
The symptoms of DKA can vary in severity but typically include:
Deep and labored breathing. This is known as Kussmaul respiration and is the body’s attempt to eliminate excess carbon dioxide and reduce blood acidity.
Dehydration. The high blood glucose levels and subsequent increase in urination cause significant fluid loss, leading to dehydration. Dehydration can manifest as excessive thirst, dry mouth, and decreased urine output.
Increased urination. The kidneys attempt to remove excess glucose from the blood by excreting it in the urine. This leads to increased urine production, a condition known as polyuria.
Other symptoms of DKA can include nausea, vomiting, abdominal pain, fatigue, confusion, and fruity-smelling breath. If left untreated, DKA can progress to a life-threatening condition, causing severe electrolyte imbalances and potentially leading to coma or even death.
Prompt medical attention is crucial when DKA is suspected. Treatment typically involves hospitalization for intensive monitoring and management. The primary goals of DKA treatment are to restore fluid balance, correct electrolyte abnormalities, normalize blood glucose levels, and reverse metabolic acidosis. This is achieved through a combination of intravenous fluids, insulin administration, and close monitoring of blood glucose, electrolyte levels, and acid-base status.
Prevention of DKA involves careful diabetes management, including regular monitoring of blood glucose levels, adherence to prescribed insulin regimens, timely adjustments of insulin doses, and prompt medical intervention during periods of illness or other stressors that can trigger DKA.
Long-Term Effects and Treatment Strategies
Uncontrolled diabetes can have significant implications for various organ systems in the body, leading to a wide range of complications. These complications primarily result from the long-term effects of sustained high blood glucose levels and the associated vascular damage.
One of the major areas affected by uncontrolled diabetes is the microvasculature, which consists of small blood vessels throughout the body. Persistent high blood glucose levels can lead to damage to the walls of these vessels. In arterioles, this damage manifests as a condition called hyaline arteriolosclerosis, characterized by the accumulation of hyaline deposits in the vessel walls. These deposits, primarily made up of proteins, cause the arterioles to become hard and inflexible, compromising blood flow to various tissues and organs.
In capillaries, the tiny blood vessels responsible for oxygen and nutrient exchange with tissues, the basement membranes that support and regulate the passage of substances can thicken. This thickening can impair the efficient exchange of oxygen and nutrients, resulting in tissue hypoxia, or inadequate oxygen supply. The impaired oxygenation can have detrimental effects on various organs, including the eyes, kidneys, and nerves.
One of the most well-known complications of diabetes is diabetic retinopathy, which affects the eyes. Prolonged exposure of the retinal blood vessels to high blood glucose levels can lead to damage and the development of abnormal blood vessels in the retina. These abnormalities can cause vision impairment and, if left untreated, may progress to blindness.
Diabetic nephropathy, or kidney damage, is another common complication. The increased blood glucose levels and the resulting vascular changes can affect the small blood vessels in the kidneys. Over time, this can lead to impaired kidney function and the development of a condition called nephrotic syndrome. Nephrotic syndrome is characterized by proteinuria (excessive protein in the urine), reduced urine output, and progressive decline in kidney function. If left untreated, it can ultimately progress to end-stage renal disease, requiring dialysis or kidney transplantation.
Neuropathy, or nerve damage, is a prevalent complication of diabetes. The exact mechanisms underlying diabetic neuropathy are not fully understood, but prolonged exposure to high blood glucose levels is thought to contribute to nerve damage. This can lead to a range of symptoms, including decreased sensation, particularly in the feet and hands, known as peripheral neuropathy. Autonomic neuropathy, affecting the nerves that control involuntary body functions, can also occur, leading to various issues such as gastrointestinal problems, sexual dysfunction, and impaired regulation of blood pressure and heart rate.
Uncontrolled diabetes also increases the risk of developing atherosclerosis, a condition characterized by the build-up of plaque within medium and large arteries. The chronic inflammation and vascular damage caused by diabetes contribute to the formation of fatty deposits within the arterial walls. Over time, these deposits can lead to narrowing and hardening of the arteries, reducing blood flow and potentially resulting in serious complications such as heart attacks and strokes.
The management of diabetes aims to prevent or minimize the development of complications. Treatment approaches may involve lifestyle modifications, including adopting a healthy diet, regular physical activity, and weight management. Oral antidiabetic medications, such as metformin and other classes of drugs, can be prescribed to improve blood glucose control. In cases where oral medications are insufficient, insulin therapy may be necessary to maintain optimal blood glucose levels.
It is essential to carefully monitor blood glucose levels and adhere to the prescribed treatment plan to prevent hypoglycemia, a condition characterized by low blood glucose levels. Hypoglycemia can have immediate adverse effects on the body and can be life-threatening if not promptly addressed.
Regular medical check-ups and ongoing management of diabetes, including comprehensive eye exams, kidney function tests, and foot examinations, are crucial for early detection and intervention to minimize the risk of complications. With proper management and control of blood glucose levels, individuals with diabetes can reduce the risk and severity of complications, leading to improved overall health and quality of life.
Conclusion
Diabetes mellitus encompasses a complex interplay of mechanisms, with Type 1 and Type 2 diabetes presenting distinct characteristics. Understanding the underlying processes and complications associated with uncontrolled diabetes is crucial for effective management and prevention. By promoting awareness, early diagnosis, and comprehensive treatment strategies, we can strive for better control of blood glucose levels, reduce the risk of complications, and enhance the overall well-being of individuals living with diabetes.
Subscribe
to get our
LATEST NEWS
Related Posts

Chronic & Debilitating Diseases
Renopathology Tipping Point: Deciphering the Molecular Code of Stage 2 Chronic Kidney Disease
The molecular events of Stage 2 CKD, from inflammation to lipid metabolism, offer insights for diagnosis and treatment.
Chronic & Debilitating Diseases
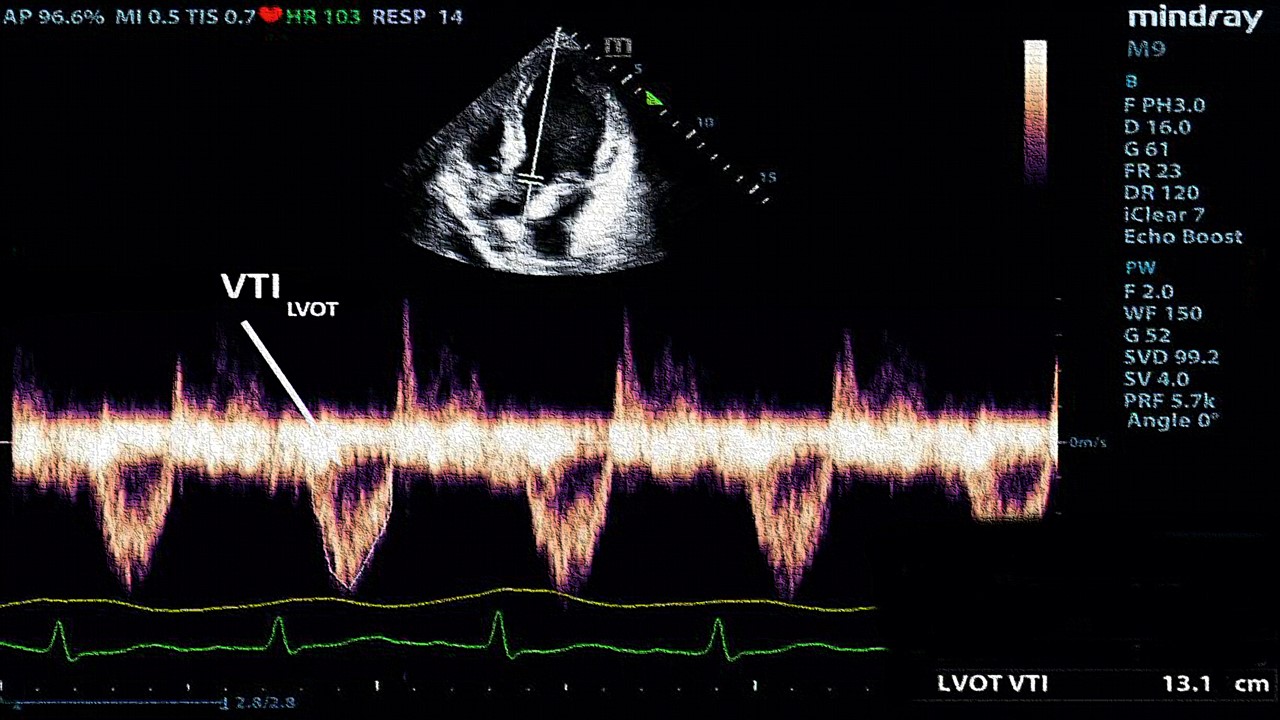
A New Lens on Shock: Hemodynamic Insights Through Critical Care Ultrasound
CCU has transformed the hemodynamic assessment of shock, delivering a reliable, reproducible, and non-invasive tool for ICU clinicians.