Congenital Diaphragmatic Hernia (CDH) is a rare birth defect that occurs when the diaphragm, a muscle that separates the chest and abdomen, does not fully form during fetal development. CDH occurs in approximately 1 in 2,500-4,000 births worldwide, with a mortality rate of up to 60%. This makes it a serious condition that requires immediate medical attention.
Classification
There are three classifications of CDH: Bochdalek hernia, Morgagni hernia, and diaphragmatic eventration.
Bochdalek hernia is the most common type of CDH, accounting for 85-90% of cases. It occurs when the posterolateral aspect of the diaphragm fails to form properly, creating an opening through which abdominal organs can enter the chest cavity. This type of CDH typically affects the left side of the diaphragm, but it can also affect the right side or both sides.
Morgagni hernia is a less common type of CDH, accounting for only 2-4% of cases. It occurs when the anterior aspect of the diaphragm fails to form properly, creating a smaller opening through which abdominal organs can enter the chest cavity. This type of CDH typically affects the right side of the diaphragm.
Diaphragmatic eventration is a rare form of CDH in which the diaphragm is abnormally thin and weak, allowing the abdominal organs to push into the chest cavity. Unlike Bochdalek and Morgagni hernias, the diaphragm is present and intact, but it is unable to properly support the organs within the abdomen. This can lead to respiratory distress and other complications, and surgical intervention may be necessary to repair the diaphragm and restore its proper function.
While Bochdalek hernia is the most common type of CDH, it is important to note that each type can present with varying degrees of severity and associated medical issues. In some cases, CDH may be accompanied by other congenital anomalies or genetic syndromes, further complicating diagnosis and treatment. Therefore, a thorough evaluation and management plan tailored to each individual case is essential for achieving the best possible outcomes for infants with CDH.
Pathophysiology
The pathophysiology of congenital diaphragmatic hernia (CDH) is complex and involves several factors that can affect fetal development and the function of the respiratory system after birth.
Normally, the diaphragm forms as a flat muscle that separates the chest and abdomen during fetal development. However, in cases of CDH, the diaphragm fails to fully form, leaving a hole or opening in the muscle. This opening can vary in size and location, depending on the type and severity of CDH.
The migration of abdominal organs into the chest cavity can have a significant impact on lung development and function. As the abdominal organs enter the chest cavity, they can compress and displace the developing lungs, preventing them from fully expanding and functioning properly. This can lead to respiratory distress after birth and other associated medical issues, such as pulmonary hypertension, pulmonary hypoplasia, and persistent pulmonary hypertension of the newborn (PPHN).
In addition to the physical displacement of the lungs, the presence of the abdominal organs in the chest cavity can also lead to compression of the heart and blood vessels, further complicating cardiovascular function in affected infants.
Furthermore, the pathophysiology of CDH can also involve genetic factors and signaling pathways that influence diaphragm development and function. Recent research has suggested that mutations or variations in certain genes, such as FOG2 and ZFPM2, may contribute to the development of CDH. These genes play a role in the regulation of key developmental pathways, such as the Wnt signaling pathway, which is essential for proper diaphragm formation.
A better understanding of these factors is essential for improving diagnosis, treatment, and management of this challenging condition.
Diagnosis
Diagnosis of congenital diaphragmatic hernia (CDH) is typically made through a combination of prenatal and postnatal diagnostic procedures. Prenatal diagnosis is becoming increasingly common due to routine prenatal ultrasound screening during pregnancy. During a routine ultrasound examination, a doctor can identify an abnormality in the fetal chest or abdomen that may suggest the presence of CDH.
If CDH is suspected, additional prenatal testing, such as fetal MRI or fetal echocardiography, may be recommended to confirm the diagnosis and assess the severity of the condition. These tests can provide more detailed images of the fetal chest and abdomen, allowing doctors to better evaluate the extent of the hernia and assess the impact on fetal development.
Following birth, a physical examination will be conducted to confirm the presence of CDH. A chest x-ray is typically the first imaging test used to evaluate the extent of the hernia and assess the impact on lung function. The x-ray can also reveal other associated medical issues, such as lung hypoplasia or pulmonary hypertension. Echocardiography may also be used to assess cardiovascular function and identify any associated heart defects.
In some cases, additional imaging tests, such as CT scans or MRI, may be needed to confirm the diagnosis and assess the extent of the hernia. CT scans can provide more detailed images of the chest and abdomen, while MRI can provide detailed images of soft tissue structures, such as the diaphragm and surrounding organs.
Management
Treatment and management options for congenital diaphragmatic hernia (CDH) depend on the severity of the condition and the presence of associated medical issues. In general, the main goals of treatment are to repair the diaphragmatic hernia, restore proper organ placement, and optimize respiratory and cardiovascular function.
In severe cases of CDH, immediate surgical intervention may be necessary to repair the diaphragm and reposition the abdominal organs. This procedure, known as a diaphragmatic hernia repair, typically involves a combination of surgical techniques to close the hole in the diaphragm and reposition the abdominal organs. The timing of the surgery depends on various factors, including the stability of the infant’s respiratory and cardiovascular function and the severity of the hernia.
In less severe cases of CDH, supportive measures may be used to help the infant breathe and manage associated medical issues. Mechanical ventilation, or the use of a breathing machine, is often necessary to support respiratory function and may be needed for several weeks or even months. High-frequency oscillatory ventilation (HFOV), a type of mechanical ventilation that uses high-frequency pressure waves to support lung function, may also be used in some cases.
In addition to mechanical ventilation, medications may be used to manage associated medical issues, such as pulmonary hypertension or infections. Pulmonary hypertension is a common complication of CDH and can be managed with medications that relax the blood vessels in the lungs. Antibiotics may also be used to treat or prevent infections, which can be a significant risk in infants with CDH.
Once the infant’s respiratory and cardiovascular function is stable, feeding and nutritional support may be initiated. In some cases, a gastrostomy tube, a small tube that is inserted into the stomach through the skin of the abdomen, may be used to deliver nutrition directly to the infant’s stomach.
Long-term management of CDH may involve ongoing respiratory and cardiovascular monitoring, nutritional support, and developmental assessments. Infants with CDH are at increased risk for developmental delays and other medical issues, and may require ongoing medical management and support as they grow and develop.
Prognosis
The prognosis for infants with congenital diaphragmatic hernia (CDH) can vary greatly depending on the severity of the condition and the presence of associated medical issues. CDH can cause significant respiratory and cardiovascular distress, and infants with this condition are at increased risk for a number of complications, including lung infections, pulmonary hypertension, and developmental delays.
The survival rate for infants with CDH has improved over time due to advances in neonatal intensive care and surgical techniques. However, the prognosis remains guarded for severe cases of CDH, particularly those associated with significant lung and cardiovascular dysfunction. In some cases, despite aggressive treatment and management, infants with CDH may not survive.
Several factors can impact the prognosis for infants with CDH, including the size and location of the diaphragmatic hernia, the degree of lung hypoplasia, the presence of associated medical issues, and the infant’s overall health and response to treatment. Infants with large or bilateral diaphragmatic hernias are generally at higher risk for respiratory and cardiovascular complications and may have a poorer prognosis than those with smaller or unilateral hernias.
Long-term outcomes for infants with CDH can also be variable, with some infants experiencing ongoing respiratory or developmental issues. Infants with CDH may require ongoing respiratory and cardiovascular monitoring, nutritional support, and developmental assessments to optimize their long-term outcomes.
In general, early diagnosis and prompt, effective treatment are key factors in improving the prognosis for infants with CDH. A multidisciplinary approach to care, involving neonatologists, pediatric surgeons, respiratory therapists, and other specialists, can help to optimize outcomes for these vulnerable infants.
Conclusion
In conclusion, CDH is a rare and serious birth defect that requires immediate medical attention. With proper diagnosis and treatment, many infants with CDH are able to overcome the challenges associated with this condition and lead healthy, happy lives. Increased awareness and advocacy efforts can help to support those affected by CDH and promote ongoing research into effective treatments and management options.
Subscribe
to get our
LATEST NEWS
Related Posts

Pathophysiology & Experimental Medicine
Autism Disentangled: FOXG1 Drives Neural Imbalance in the Developing Brain
If FOXG1 overexpression can be modulated, either genetically or pharmacologically, it may be possible to correct the neurodevelopmental imbalances underlying ASD.
Pathophysiology & Experimental Medicine
Adaptive Interactions: How Stimuli-Responsive Materials Revolutionize Cellular Studies
Stimuli-responsive materials revolutionize cellular dynamics research by replicating ECM adaptability, unlocking insights into cell behavior and regulation.

Pathophysiology & Experimental Medicine
Eternal Lip Layers: Unlocking the Human Keratinocyte Potential
The lips, long celebrated for their role in communication and aesthetics, now stand at the forefront of scientific innovation.
Pathophysiology & Experimental Medicine
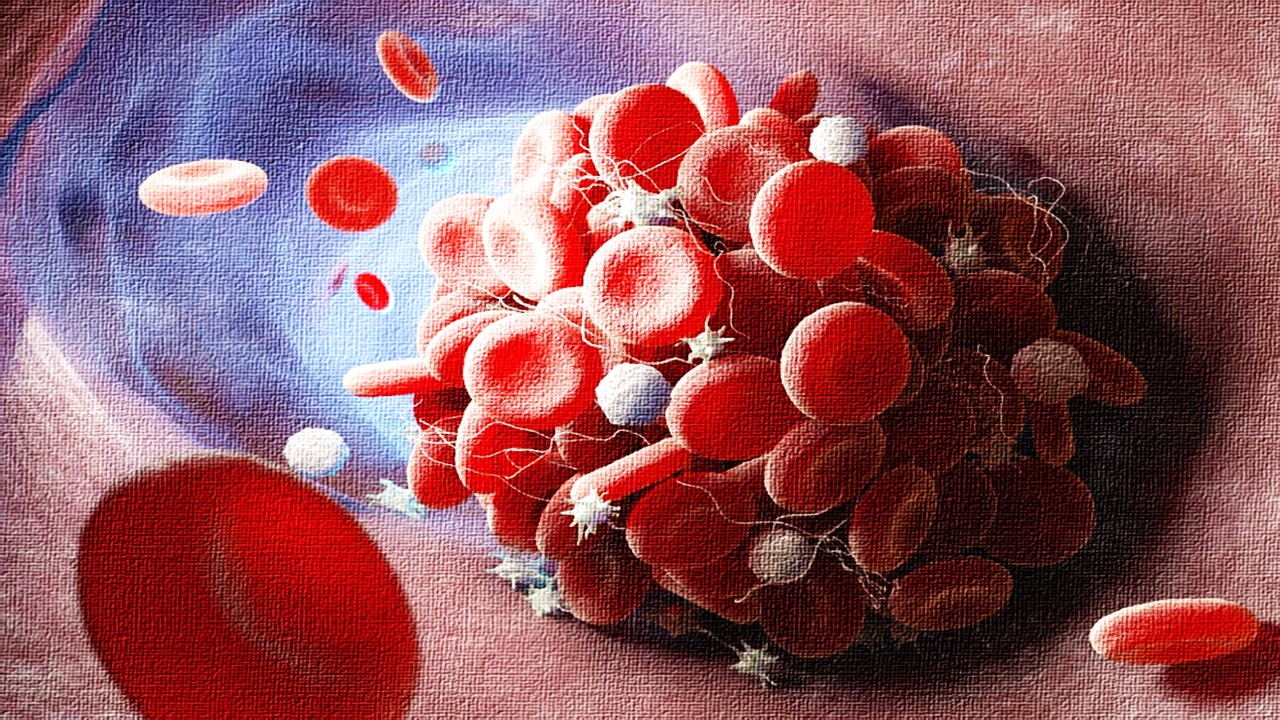
Thrombosis-Free Surfaces: Preventing Blood Clot Formation on Medical Implants Through Selective Protein Interactions
The synthesis and mechanisms of SPI coating are explored, evaluating its potential to overcome the limitations of traditional antifouling surfaces.











