In the evolving field of drug discovery, the pursuit of more efficient, targeted, and sustainable solutions has always been a central goal. Traditional drug discovery methods – while pivotal – are often hampered by significant challenges, especially when it comes to the development and application of antibodies. In recent decades, nanobodies, a novel form of single-domain antibody fragments, have emerged as transformative agents, offering profound advantages over conventional antibodies, particularly in the diagnosis and treatment of cardiovascular diseases (CVDs).
As cardiovascular diseases continue to be the leading cause of mortality worldwide, the medical and scientific communities are in constant search of more precise, accessible, and scalable therapeutic solutions. Nanobodies, originally discovered in camelids, hold promise due to their small size, high stability, and specificity. This innovation is poised to redefine our approach to not only diagnostics but also therapeutic interventions for CVDs.
Cardiovascular Disease: The Global Burden
Cardiovascular diseases are responsible for a staggering number of deaths annually, with the trend showing little sign of decline. The United States and Europe both report high mortality rates linked to CVDs, driven by factors including aging populations, lifestyle choices, and rising comorbidities such as obesity, hypertension, and diabetes. Smoking, particularly among adolescents using flavored electronic cigarettes, is a growing concern, as is the increasing prevalence of congenital heart diseases in younger populations. These factors contribute to the ongoing challenge of managing CVD risk and health outcomes globally.
In 2020, the global CVD-related mortality rate reached alarming levels. In some European countries, such as Romania and Bulgaria, the prevalence of cardiovascular disease affects over half of the population. Furthermore, obesity and poor nutritional habits have exacerbated the situation, with higher body mass index (BMI) correlating to increased risks of conditions like atrial fibrillation, heart failure, and hypertension. This ever-growing burden highlights the need for innovation in both prevention and treatment strategies.
Diagnostic Challenges in Cardiovascular Disease
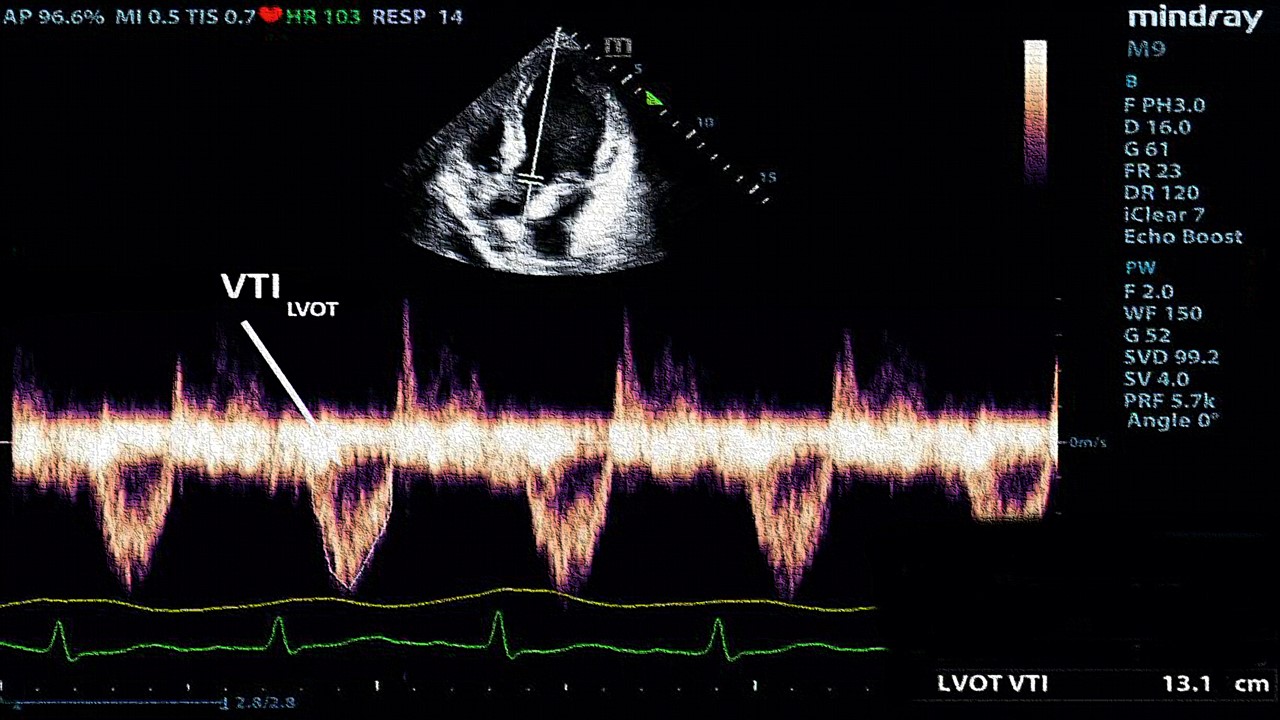
The diagnosis of cardiovascular disease has become more complex as the number of patients – and the range of diagnostic tools -continues to grow. Traditional methods, such as electrocardiograms (ECG), echocardiograms, and cardiac catheterization, have long been the standard, but they are often time-consuming, require specialized equipment, and depend on highly trained personnel. Moreover, these techniques do not always offer the sensitivity or specificity needed to detect early-stage or subtle manifestations of CVDs.
One of the most promising advancements in this field is the use of nanobodies. Nanobodies provide a more accessible, cost-effective alternative that offers significant advantages over conventional diagnostic methods. Their smaller size and ability to penetrate tissue more effectively make them ideal candidates for advanced imaging techniques. Nanobodies can be utilized for highly sensitive and specific detection of molecular targets associated with CVDs, potentially transforming how we approach early diagnosis and monitoring of disease progression.
Nanobodies: A Breakthrough in Cardiovascular Diagnostics
The discovery of nanobodies has been revolutionary. These single-domain antibody fragments possess unique properties that distinguish them from traditional antibodies, such as their ability to bind antigens with high affinity despite their smaller molecular size. First identified in camelids, nanobodies are approximately one-tenth the size of conventional antibodies, making them highly adaptable for diagnostic and therapeutic applications.
In contrast to traditional antibodies, which are produced in large mammals like mice or rabbits, nanobodies can be generated using simpler, more efficient systems such as yeast or bacterial expression systems. This not only lowers the cost of production but also eliminates the ethical concerns associated with animal use. Their smaller size enables nanobodies to penetrate tissue more effectively and bind to targets with greater precision. These qualities make them particularly valuable in the field of CVD diagnostics, where early detection of disease markers can be life-saving.
Nanobodies have shown potential in targeting specific biomarkers for conditions like coronary artery disease (CAD) and heart failure, enabling physicians to diagnose these conditions more rapidly and accurately than ever before. Their ability to bind to even the smallest molecular changes within the cardiovascular system provides a level of sensitivity that conventional antibodies cannot match.
Nanobodies in Cardiovascular Therapies
Beyond diagnostics, nanobodies offer exciting possibilities for treating cardiovascular diseases. Traditional antibodies, while effective, often suffer from limitations such as poor tissue penetration and prolonged circulation times, which can lead to adverse side effects. Nanobodies, on the other hand, have much faster pharmacokinetics due to their smaller size, reducing the risk of accumulation in non-target tissues and minimizing the likelihood of off-target effects.
In therapeutic applications, nanobodies can be engineered to guide drug-loaded vesicles or inhibitors directly to the site of disease, significantly improving the efficacy of treatments while reducing systemic exposure. This precision is particularly important in the treatment of diseases such as CAD, where targeted drug delivery can make the difference between managing symptoms and halting disease progression.
Moreover, nanobodies are being explored as potential therapeutic agents in inflammation and infectious diseases, in addition to their role in treating cardiovascular conditions. Their stability, water solubility, and ability to be produced in large quantities make them ideal candidates for both research and clinical applications. Nanobody-based therapies are already showing promise in preclinical studies, with several candidates moving toward clinical trials for a variety of cardiovascular conditions.
The Future of Nanobody Research in Cardiovascular Medicine
Despite their many advantages, nanobody technology is still in its infancy, particularly in the field of cardiovascular medicine. As research continues, it is crucial to address some of the challenges associated with their production and application. While yeast and bacterial expression systems offer a low-cost alternative to traditional methods, there are still technical hurdles to overcome, such as ensuring the proper folding and stability of nanobodies in vivo.
Recent advances in yeast surface display (YSD) technologies have provided new avenues for improving nanobody production. By fusing nanobodies to surface proteins on yeast cells, researchers can rapidly evaluate the binding activity of nanobodies and optimize their properties for diagnostic or therapeutic use. These techniques are paving the way for the development of next-generation nanobodies that are more effective and easier to produce.
Furthermore, efforts to engineer nanobodies for specific cardiovascular targets, such as G protein-coupled receptors (GPCRs), are opening up new possibilities for personalized medicine. By tailoring nanobodies to bind specific proteins associated with an individual’s cardiovascular risk profile, it may soon be possible to develop highly targeted therapies that offer better outcomes with fewer side effects.
Nanobodies as the Future of Cardiovascular Medicine
The introduction of nanobodies into the field of cardiovascular medicine represents a paradigm shift in both diagnostics and therapy. Their small size, high specificity, and ease of production make them an attractive alternative to traditional antibodies, with the potential to revolutionize how we detect and treat cardiovascular diseases. As research progresses, nanobodies may become a cornerstone of personalized medicine, offering new hope for millions of patients worldwide who suffer from heart disease. Their application in drug delivery, diagnostics, and therapy will undoubtedly shape the future of cardiovascular medicine, bringing us closer to more effective and accessible solutions for one of the world’s most pressing health challenges.
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts

Chronic & Debilitating Diseases
Renopathology Tipping Point: Deciphering the Molecular Code of Stage 2 Chronic Kidney Disease
The molecular events of Stage 2 CKD, from inflammation to lipid metabolism, offer insights for diagnosis and treatment.
Chronic & Debilitating Diseases
A New Lens on Shock: Hemodynamic Insights Through Critical Care Ultrasound
CCU has transformed the hemodynamic assessment of shock, delivering a reliable, reproducible, and non-invasive tool for ICU clinicians.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.