Artificial Intelligence promises to revolutionize countless fields within the life sciences – from diagnostics to drug discovery, the applications are vast and significant. The field of immuno-oncology stands to greatly benefit from adopting AI, which promises to solve some long-standing challenges in the field – particularly the prediction of responses to treatment, which is known to require gargantuan amounts of data. There remain a number of obstacles to be overcome for AI to deliver its full potential in the healthcare setting on oncology – both in regards to technical advancements, as well as organizational and human barriers.
Predicting Treatment Response
Immunotherapies have transformed multiple areas of oncology – particularly hematological malignancies. However, only 20-40% of patients respond positively to immunotherapeutic treatment. Additionally, they can trigger severe autoimmune side effects; it therefore becomes critical to improve our predictive capabilities for determining responders when beginning trials or offering treatment.
Predictive analysis for treatment response typically involves the examination of as many biomarkers as possible. In immune checkpoint blockade, these are combined to form immunoscore and immunophenoscores – composite values which estimate the probability of treatment response. However, arriving at such estimates is riddled with uncertainties: different biomarkers do not always have simply additive or subtractive effects to the chance of treatment response.
Machine Learning
Harnessing machine learning to compute the complex interactions between different biomarkers – as well as collecting as much data as possible about them, seems a natural application. This is already happening in multiple ways. Studies have shown that well-trained machine learning algorithms can identify Major Histocompatibility Complexes with high accuracy, a development of high importance to immunotherapy. Analyses such as these can predict the binding efficiency of novel agents to MHC antigens, including possible neoantigens, which can prove critical in improving patient selection.
Additionally, machine learning has also shown potential in predicting lung adenocarcinoma prognosis based on genetic mutations – as well as identifying new genes and mutations that may be important for disease and treatment outcomes. Groundbreaking research published in Cell’s Patterns used RNA sequences to extract useful data which was developed into predictive biomarkers, to characterize the Tumour Microenvironment (TME), and determine immune checkpoint blockade responses using machine learning models. RNA-sequence data is more readily available than individual biological and visual assays, making this a promising approach for the future.
Imaging-based Predictions
Artificial Intelligence has also made incredible advances in providing both unsupervised and supervised solutions for imaging-based judgments throughout the field of medicine. This can also be exploited to provide implementations for predicting immunotherapy responsiveness. Cancer patients will generally receive detailed imaging diagnostics throughout the development of their disease, making this a highly available source of data for training AI – this is known as radiomics, which takes advantage of AI to provide characterization of imaging.
A research group working on Non-Small Cell Lung Cancers (NSCLCs) did just that, developing non-invasive radiomic biomarkers and using AI to predict the responsiveness of metastatic NSCLCs to immunotherapy. The study found some clear links for responsiveness, such as morphological heterogeneity and spherical lesions. Another study utilized machine learning to differentiate between metastases to the pituitary gland and autoimmune hypophisitis (a side-effect of immune checkpoint blockade therapy affecting the pituitary gland), establishing AI as a critical tool in other decision-making points of immunotherapy. Radiomic biomarkers can be developed further, utilising CT, MRI and RNAseq data – and AI can provide an increasingly detailed examination of high-resolution data generated by them.
Another avenue of investigation that can be pursued would be the characterization of the white blood cells in the tumour microenvironment – which can also have strong implications for immunotherapies. Research has already tested CIBERSORT, a tool developed at Stanford using machine learning to characterize cell populations from complex tissue samples, to demonstrate its efficiency at profiling Tumor Infiltrating Leukocytes.
Barriers for Adoption
There are countless other examples of AI in predictive immuno-oncology that could be outlined here, but we consider it more important to broach the subject of the barriers for its wider implementation – many of which can be gleaned and anticipated from AI usage in other fields of medicine. Naturally, the first obstacle is always the availability and heterogeneity of data – Artificial Intelligence methods perform best with humongous datasets. Even when these exist, data sharing may not be widespread between different institutions; and when it is, the data can often be in different formats or structures. Not only is more data a constant need for improving AIs – data fragmentation is also a problem that needs to be addressed through stakeholder cooperation and standardization.
There are also multiple social and human-based challenges. Whilst Artificial Intelligence can not only improve outcomes, while saving time and lowering costs, if implemented properly, it is not an absolute replacement for human-based diagnostics. Supervision will frequently be required, and opposition from medical professionals that may see AI as their replacement can be anticipated. These can be resolved through better education of staff and focused strategies for the integration of Artificial Intelligence in the diagnostic process. However, AI is not flawless – and the question of liability in the event where erroneous diagnoses or predictions are made cannot be avoided. This presents a challenge that can only be solved through cooperation with regulatory bodies, and will need to be addressed as AI grows in prominence across various fields.
Artificial Intelligence has the potential to revolutionize the greatest challenge faced by immunotherapies – patient selection and predictive tumour characterization. Additionally, with the increasing adoption of AI, we can also expect a greater degree of regularization in terms and definitions in the field – as we have seen in the past with tumour mutational burden (TMB), which is another challenge faced in oncology. The technology is still at a young stage where models and practices require further refinement, but we can already see multiple moral quandaries that will need to enter the wider medical discourse before AI can see far-reaching adoption.
Join Proventa International’s Oncology Strategy Meeting in 2022 for further insights on the potential of Artificial Intelligence and the future opportunities for the technology, as well as the barriers that need to be overcome, delivered by world-renowned researchers and stakeholders.

Subscribe
to get our
LATEST NEWS
Related Posts
Bioinformatics & Multiomics
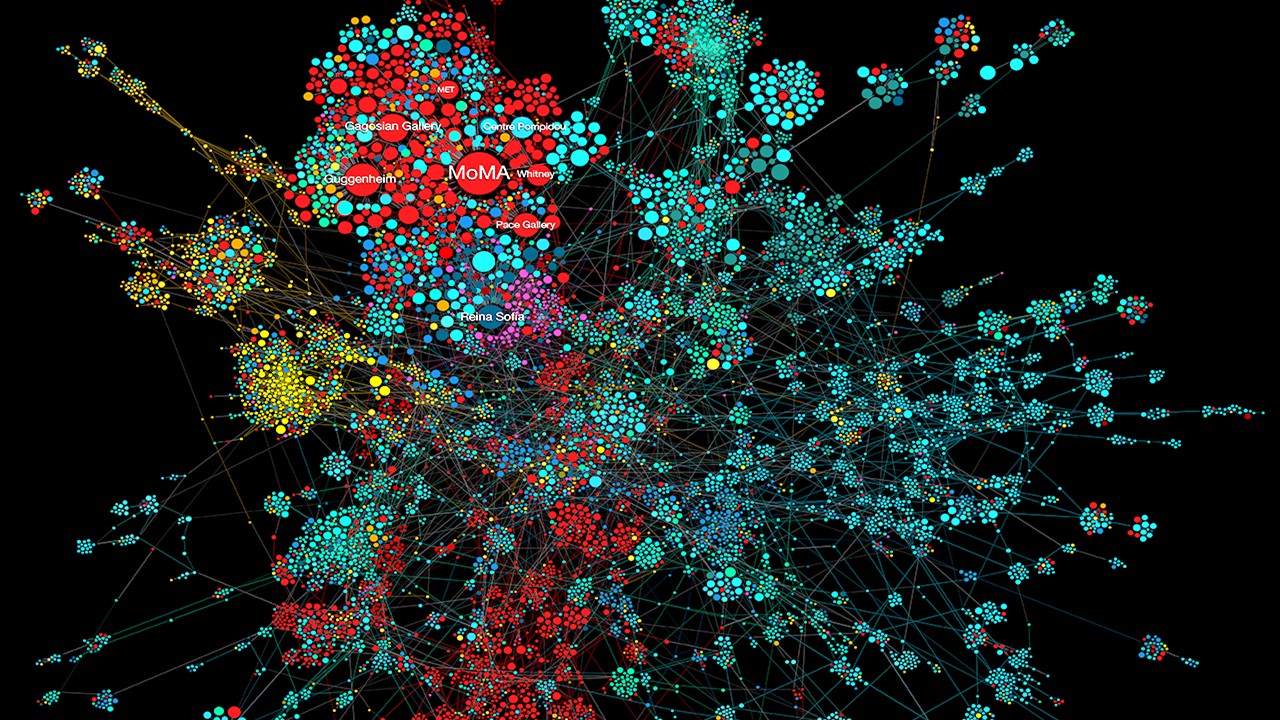
Mapping the Invisible Arrows: Unraveling Disease Causality Through Network Biology
What began as a methodological proposition—constructing causality through three structured networks—has evolved into a vision for the future of systems medicine.
Bioinformatics & Multiomics
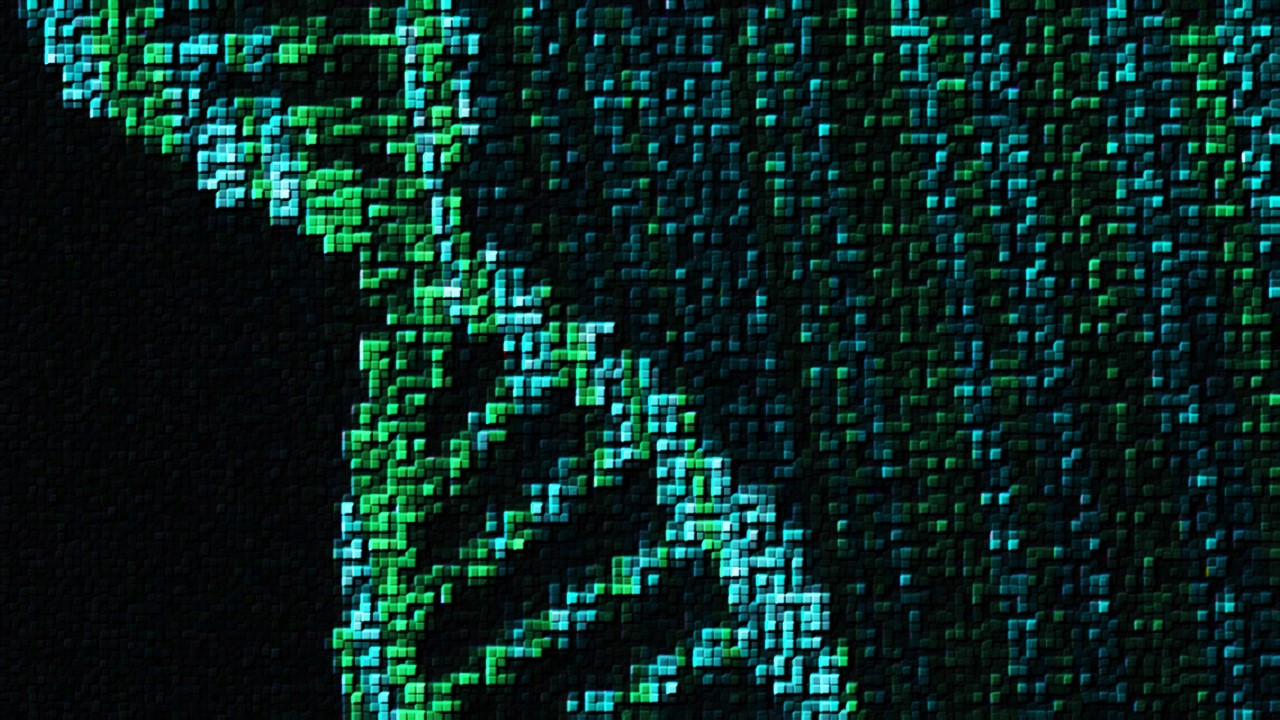
Open-Source Bioinformatics: High-Resolution Analysis of Combinatorial Selection Dynamics
Combinatorial selection technologies are pivotal in molecular biology, facilitating biomolecule discovery through iterative enrichment and depletion.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.
Designing Better Sugar Stoppers: Engineering Selective α-Glucosidase Inhibitors via Fragment-Based Dynamic Chemistry
One of the most pressing challenges in anti-diabetic therapy is reducing the unpleasant and often debilitating gastrointestinal side effects that accompany α-amylase inhibition.













