As the industry develops more precise and complex drugs and treatments, the data generated regarding safety and adverse events, as well as individual case safety reports, also rises exponentially. Finding innovative and novel ways to handle the increased volumes of data is one of the challenges facing the wider field of pharmacovigilance. Cutting-edge technologies based on Artificial Intelligence (AI) promise to revolutionize how we handle this data, as well as overhaul the typical work and career paths for pharmacovigilance professionals. In this article, we will briefly explore the possible applications, and impacts, of increased AI adoption on pharmacovigilance.
The Nature of Pharmacovigilance
The building block of ensuring drug safety is the reporting and handling of Adverse Event (AE) reactions to treatments – these can be recorded from a diverse array of sources, such as patients presenting AEs in clinical trials or hospitals, or even reporting side effects on social media. The management of AEs involves a great deal of repetitive tasks – which can be well suited for AI to handle. These include multiple stages of the AE handling process: from the intake of reports, to patient followup, reviewing and reporting results to regulatory authorities. While the processing of AEs may involve a great deal of repetitive, administrative tasks, it still requires significant decision-making capabilities in assessing each adverse event, which makes automating the process more challenging. AI with decision-making capabilities holds the potential to change this.
Applications of AI in Pharmacovigilance
Deep learning (DL), machine learning (ML) and natural language processing (NLP) models have been the aspects of AI that have been the most investigated for applications in pharmacovigilance so far. NLP remains particularly important in pharmacovigilance due to the variability of case reports for AEs – unlike other areas of the life sciences which may exhibit much more standardized terminology. Celgene, a Bristol-Myers Squibb subsidiary, developed ten cognitive services which scored over 75% in evaluating spontaneous individual case reports, which it hopes will enable a more proactive stance to drug safety. Celgene went to great lengths to reassure pharmacovigilance professionals that the models will support their decision-making, rather than replace them. This belies the worries that often come with AI taking over any processes that were previously carried out by humans, in any field.
Pfizer has also innovated a pilot study for the use of AI in AE case processing, limited to Italy. The study focused on extracting AE information from report document sources, as well as the use of databases rather than the direct and expensive annotation of source documents. The study confirmed the feasibility of AI in these applications, while also noting that larger training datasets would better improve quality. The pilot run by Pfizer only demonstrated the possibility of automating AE case processing rather than identifying cases for regulatory submission. While the pilot was successful in demonstrating how AI can support pharmacovigilance, further improvements will be needed for implementations that can carry out regulatory functions.
Regulatory Applications of AI
The implementation of AI in pharmacovigilance need not be limited to drug developers – regulators can also make extensive use of the technologies. For example, the American FDA is carrying out extensive work on machine learning models that can predict adverse events for new drugs based on post-market data for marketed drugs. This is done through the known safety profiles of previously approved drugs, using chemical similarity scores for the novel treatments.
Predicting AE profiles for novel drugs also holds promise for drug developers themselves; clinical trials often fail to capture the full breadth and depth of a drug’s safety profile. However, current models remain somewhat limited in their capabilities to predict secondary AEs which do not have a well-characterized causative basis. Better target prediction and drug binding data will naturally improve any such model, providing more mechanisms of action to draw upon to predict effects.
Obstacles for Adoption
The key obstacles for further AI uptake in pharmacovigilance are similar to other areas of the life sciences. One of the defining features of AI, and ML in particular, is that it does not truly provide explanations or interpretations for its reasonings – often operating as a “black box”. While this may be acceptable in other industries, healthcare decision-making must come with justifications – particularly when we consider that patients may have to provide their consent for their data to be used by AI.
This also shows the legal questions that greater adoption of AI will raise; questions of liability for wrong decisions and data management failures will need to be addressed, and regulators must establish frameworks within which AI technologies will operate in the field. Training new algorithms is also not without its difficulties – particularly when we consider the heterogeneity and fragmentation of AE and healthcare datasets that are needed to train them. Greater standardization and data sharing would enable further success in this area – although privacy and consent issues arise from data sharing, as well.
Pharmacovigilance also requires greater versatility than other applications that AI may be implemented in. While AI algorithms can excel at solving narrow problems, advancements will need to be made in their general capabilities before wider use of the technologies truly happens in vaccine and drug safety. This is particularly important when we consider the noisy and often randomly incomplete data that will be encountered in pharmacovigilance scenarios, although improvements in data collection and curation will likely alleviate some of this.
We see that AI holds deep potential for improving drug safety – not only through monitoring adverse events, but also predicting the safety profiles of novel drug candidates. While obstacles may be present on the path to adopting AI in pharmacovigilance, one could also see them as opportunities to rethink and modernize the field of pharmacovigilance as well. There is no longer much need to adhere to 20th century standards for individual case safety reports, or generate fragmented datasets.
Join Proventa International’s Pharmacovigilance Strategy Meeting in Boston to hear more about the developments of AI in drug safety, as well as participate in closed door roundtable format discussions on cutting edge topics in the field – led by world-renowned experts and key stakeholders.

Subscribe
to get our
LATEST NEWS
Related Posts
Bioinformatics & Multiomics
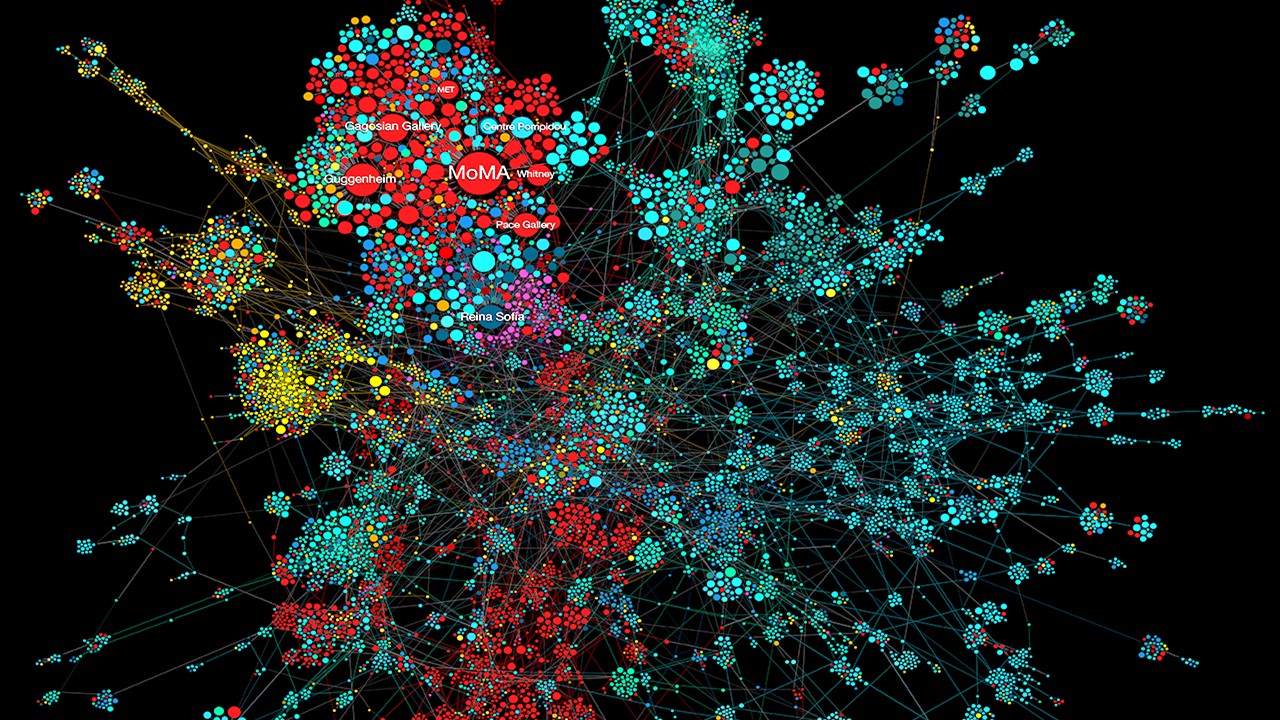
Mapping the Invisible Arrows: Unraveling Disease Causality Through Network Biology
What began as a methodological proposition—constructing causality through three structured networks—has evolved into a vision for the future of systems medicine.
Bioinformatics & Multiomics
Open-Source Bioinformatics: High-Resolution Analysis of Combinatorial Selection Dynamics
Combinatorial selection technologies are pivotal in molecular biology, facilitating biomolecule discovery through iterative enrichment and depletion.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.













