Biomarkers have shown significant potential across oncology clinical studies, especially in precision medicine for immunotherapy. Therefore, it is important that biomarker discovery and validation is optimised to produce the most effective drugs for patient populations. False positives and experimental bias are a few of the hurdles that arise during these stages.
Biomarker discovery
Biomarkers have become an important tool in precision medicine across a number of therapeutic areas. In oncology, genetic profiling technology and targeted cell therapies have seen biomarkers play an important role in disease management for cancer patients.
A cancer biomarker refers to a “tumor characteristic or a response of the body in the presence of cancer that can be objectively measured and evaluated”. Cancer biomarkers can be used to measure the risk of developing the disease; response to therapy; and/or disease progression. This information is typically used to guide clinical decisions regarding choice and timeline of treatment relative to the pathogenesis of the cancer type.
Cancer biomarkers can be classified into two categories: predictive and prognostic biomarkers.
Predictive biomarkers are typically used to predict the response to specific therapeutic interventions such as positivity/activation of HER2 that predicts response to trastuzumab in breast cancer. Overexpression of HER2, a human growth factor, results in a clinically aggressive subtype of breast cancer.
Prognostic biomarkers, on the other hand, aim to inform doctors regarding the likely patient outcome i.e. risk of disease recurrence or potential progression in the future. The 21-gene recurrence score is an example of a prognostic cancer biomarker which was predictive of breast cancer recurrence and overall survival in node-negative, tamoxifen-treated breast cancer. Pharmacokinetic/dynamic/genomic biomarkers can also be used to evaluate drug interaction with the patient.
The discovery study for biomarkers typically involves pre-clinical investigations of a pool of candidate biomarkers. The objective of this is to identify “a short list of promising markers that are associated with clinical outcome of interests for further investigation”.
The discovery of potential biomarkers, however, is a difficult task with a number of challenges that compromise the reliability of a new marker.
Challenges
One of the main challenges in biomarker discovery is the high number of false discoveries. This occurs when initial scientific findings associated with a new biomarker cannot be reproduced by other laboratories or independent samples. A number of factors can contribute to false discovery including execution errors, poor study design and bioinformatic shortcomings.
As discussed in a recent review, false discovery is closely related to the problem of scientific irreproducibility. If a biomarker discovery cannot be reproduced by a number of external sources, then it is not suitable for validation. This not only costs pharmaceutical companies significant amounts of money in funding experiments for an invalid biomarker; it also slows down the progression of biomarkers in drug development for precision medicine.
One potential solution to this problem is shifting from “the orthodox discovery of biomarkers that are common for a cancer type to screening of serum samples of each patient”. By identifying markers unique for specific tumour types, it could potentially reduce the chance of biomarkers failing to demonstrate specificity and sensitivity for a number of patients.
Bias is one of the greatest causes of failure in biomarker discovery and validation studies. The study design, through which biospecimens are analysed, is a significant source for bias. Bias occurs when “systematic error [is] introduced into sampling or testing by selecting or encouraging one outcome or answer over others”.
According to a review, it is ideal to prospectively collect biospecimens based on a succinct inclusion and exclusion criteria “pre-specified in the study protocol”. Therefore, the chance of false positives arising is theoretically lower as the discovered biomarker must meet both criteria before proceeding for validation studies.
Next-generation sequencing (NGS) is a valuable genomic tool used in cancer biomarker discovery. While the high-resolution data achieved with NGS is useful for the identifying large numbers of genomic alterations, it results in a considerable increase in computational analysis and bioinformatics support needed to interpret data. This can present an issue to smaller biotech companies with limited funding and experimental capacity.
Biomarker validation
Following discovery studies, candidate biomarker assays must undergo validation – this is split into two types. Analytic validation determines “how accurately and reliably the test measures the analyte(s) of interest in the patient specimen”. Clinical validation, on the other hand, investigates “how robustly and reliably is the test result correlated with the clinical phenotype or the outcome of interest”.
There are a number of different assay technologies available for biomarker validation depending on the specimen. For analysis of gene expression and DNA mutations, real-time polymerase chain reaction (PCR) is a popular in vitro method that can amplify small samples large enough to study. Assessing protein expression, on the other hand, often falls to immunohistochemistry.
There are two key statistical approaches for clinical validation of an assay. Internal validation divides a study population into two independent groups. For clarification, the study population “reflects the target population in which the test will be used”. One sample group, defined as the training set, is used to identify and characterise the biomarker. The second group, known as the validation set, is used to assess whether the “external validity of the biomarker/model is maintained in a sample cohort – independent from the training set”.
Unfortunately, internal validation is not sufficient to clinically validify biomarkers. Hence, external validation is required to be performed on an independent dataset. Any predictive biomarkers must undergo external validation in order to test clinical performance for regulatory approval.
According to a 2019 review, one of the primary challenges in clinical validation for biomarkers is that there is no institution responsible for monitoring the evidence for or against particular biomarker uses (at the time of publication). As a result, there is no governing body with the authority “to revoke the use of a biomarker in clinical practice if it has been shown to be invalid”. This presents a significant cause for concern with regards to the safety and efficacy biomarkers in drug development.
Clinical validation is a crucial part of biomarker development, which, if not performed correctly, could cause harm in patients. Despite innovations improving the multiple stages of validation, there are a number of challenges which need to be addressed. Continued research into optimising biomarker discovery and validation will no doubt improve the drug development process, producing more effective and safer drugs for patients.
Charlotte Di Salvo, Former Editor & Chief Medical Writer
PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts

Immunology & Oncology
The Silent Guardian: How GAS1 Shapes the Landscape of Metastatic Melanoma
GAS1’s discovery represents a beacon of hope in the fight against metastatic disease.
Immunology & Oncology
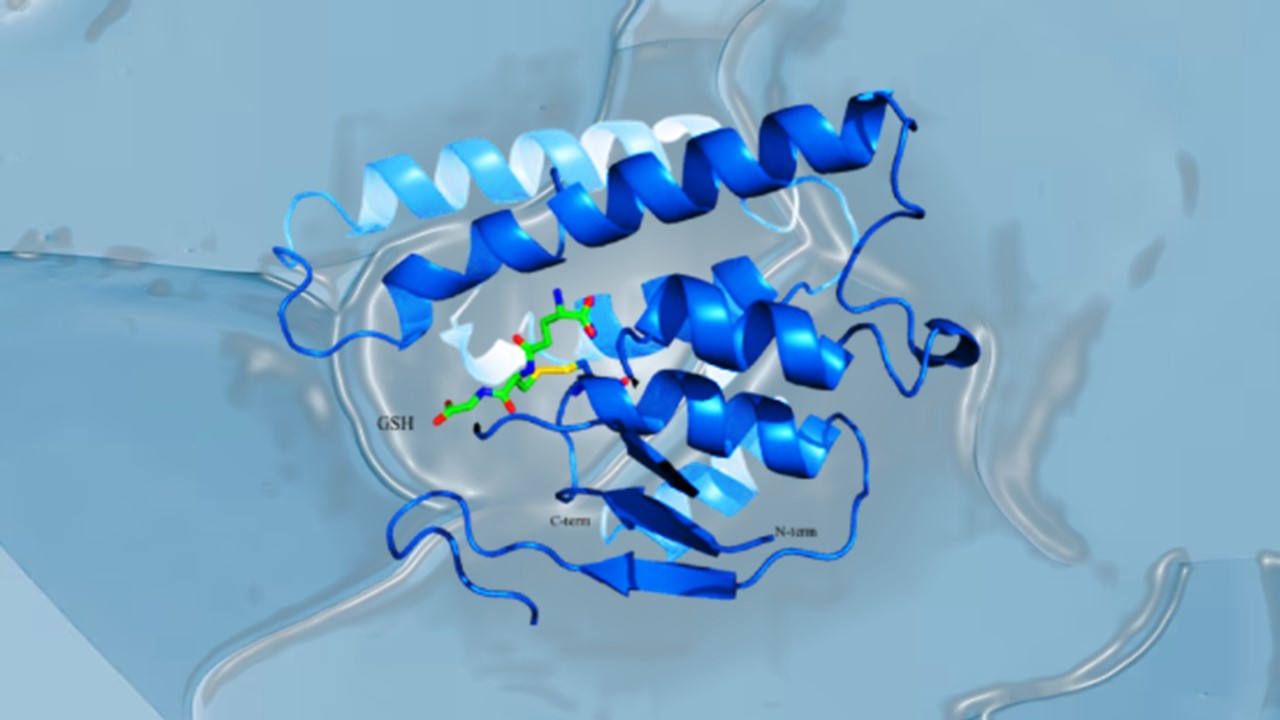
Resistance Mechanisms Unveiled: The Role of Glutathione S-Transferase in Cancer Therapy Failures
Understanding this dual role of GSTs as both protectors and accomplices to malignancies is central to tackling drug resistance.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.
Designing Better Sugar Stoppers: Engineering Selective α-Glucosidase Inhibitors via Fragment-Based Dynamic Chemistry
One of the most pressing challenges in anti-diabetic therapy is reducing the unpleasant and often debilitating gastrointestinal side effects that accompany α-amylase inhibition.