The landscape of drug discovery and biomedical innovation has long been shaped by the promise of nanoparticle technology, heralded as a transformative tool for disease diagnosis, imaging, and targeted drug delivery. Nanoparticles offer the potential to precisely navigate the body’s biological pathways, aiming to release therapeutic payloads directly at the disease site, thereby maximizing efficacy while minimizing systemic toxicity. However, despite their increasing prevalence in preclinical research, the clinical translation of nanoparticle-based drug delivery systems remains limited. There is a growing realization within the medical and scientific communities that current methodologies, while highly innovative, often fail to account for the complex interplay between nanoparticles and the human immune system. The gap between laboratory-based successes and real-world clinical outcomes persists, necessitating a shift in focus toward developing strategies that ensure nanoparticles can reliably perform in the unpredictable environment of human biology.
Nanoparticles in Clinical Applications: A Critical Overview
In clinical settings, nanoparticle drug delivery systems are designed to accomplish four primary goals: extend circulation time, enhance targeting of diseased tissues, increase retention within target regions, and release therapeutic payloads in a controlled manner. To achieve these, nanoparticles are often modified with surface chemistries that incorporate biologically relevant molecules, such as polyethylene glycol (PEG), tumor-targeting ligands, and environment-sensitive linkers. These functionalizations aim to tailor the particles’ pharmacokinetic profiles, improving biodistribution while avoiding premature clearance.
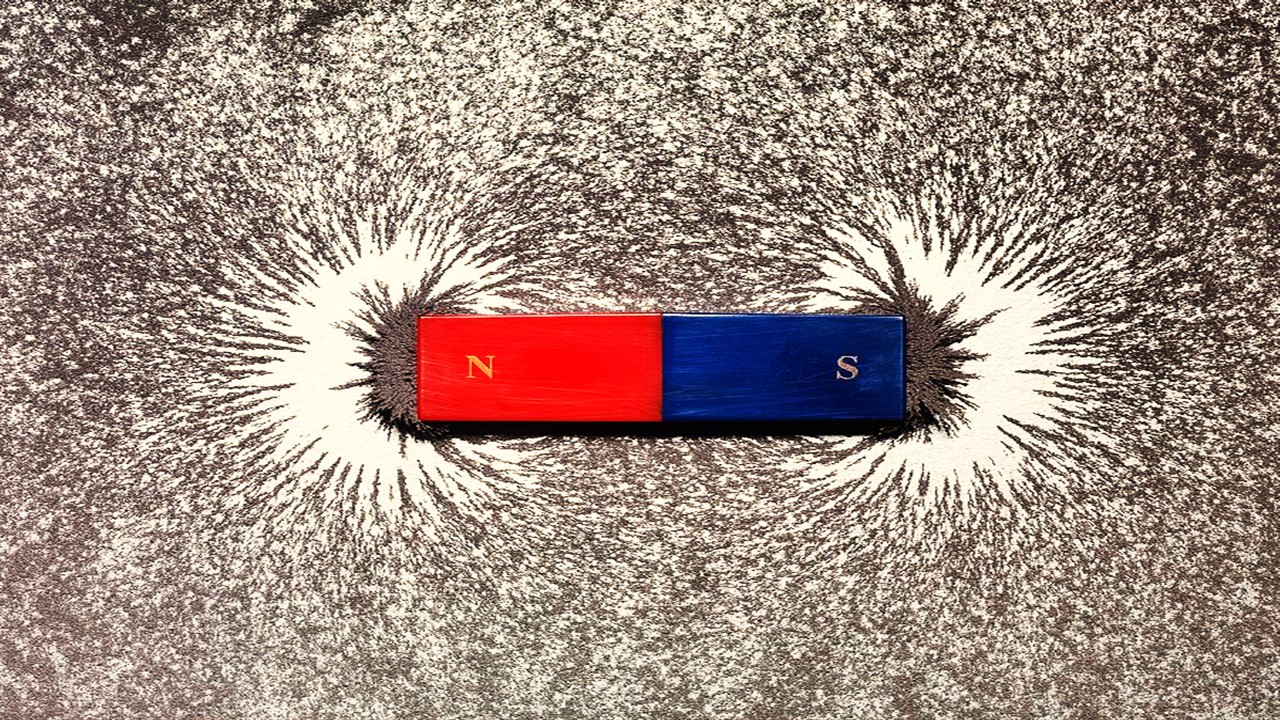
Yet, despite these efforts, significant barriers remain. Chief among them is the formation of the protein corona—a layer of proteins that adhere to the nanoparticle surface upon entry into the bloodstream. The presence of this corona dramatically alters the intended pharmacokinetics and biodistribution of the particles, often accelerating their clearance from circulation and reducing their ability to target disease sites effectively. The phenomenon, combined with the process of opsonization, which marks particles for immune clearance, presents a formidable challenge to nanoparticle persistence in the human body.
Clinically, this underscores the need for a better understanding of how surface modifications can either exacerbate or mitigate these immunological interactions. It is critical to evaluate the performance of these nanoparticle modifications not only in controlled environments but also under the complex and variable conditions of human physiology, where factors such as patient-specific immune responses and disease states can significantly alter therapeutic outcomes.
Preclinical Models: Translating Data for Clinical Relevance
When advancing nanoparticle formulations toward clinical trials, selecting the appropriate preclinical models is paramount. The clinical relevance of nanoparticle pharmacodynamics—absorption, distribution, metabolism, and excretion (ADME)—hinges on how accurately animal models mimic human disease and immune responses. Current practice often involves a progression from lower-order vertebrates to more complex mammalian systems. However, the clinical utility of these models depends on their ability to predict the biodistribution, clearance kinetics, and therapeutic efficacy of nanoparticles in humans.
For initial toxicity and clearance studies, zebrafish models have gained traction due to their high throughput, low cost, and relevant immune system similarities with humans. The zebrafish’s transparent body enables real-time in vivo imaging, providing valuable insights into nanoparticle behavior post-administration. Studies have demonstrated that PEGylated nanoparticles exhibit extended circulation in zebrafish, echoing their performance in mammalian systems, suggesting their utility as a predictive model for early-stage preclinical screening.
However, once initial safety profiles are established, a transition to rodent models, particularly mice, is required for more clinically relevant insights into nanoparticle behavior in mammalian physiology. Despite their widespread use, careful selection of mouse strains is crucial, as immune-compromised strains like nude or NOD Skid Gamma (NSG) mice can introduce significant biases in nanoparticle clearance data. These strains, commonly employed in cancer models due to their susceptibility to tumor formation, lack key components of the adaptive immune system, thereby impairing nanoparticle clearance mechanisms that would otherwise be active in human patients. Immune-competent mouse models, particularly those that represent a balanced Th1/Th2 immune response, provide a more robust system for evaluating nanoparticle biodistribution and efficacy.
In the clinical context, these preclinical models serve as a bridge to human trials. However, the variability in immune system activity between species complicates the extrapolation of data from animal studies to human physiology. As such, nanoparticle performance in these models must be interpreted with caution, and clinical trial design should account for potential discrepancies in immune responses between humans and preclinical models.
Route of Administration: A Clinical Decision
The route of administration (ROA) for nanoparticles is a pivotal factor in determining their clinical success. Intravenous (IV) administration remains the most common delivery method, particularly for oncological therapies, where nanoparticles must traverse the circulatory system to reach tumor sites. For nanoparticles larger than 10 nanometers, renal clearance is minimized, allowing for extended circulation times. However, IV administration poses its own challenges, as the mononuclear phagocyte system (MPS) rapidly clears foreign particles from the bloodstream. This necessitates strategic surface modifications to evade immune detection and enhance retention at the target site.
Alternatively, pulmonary administration of nanoparticles has garnered attention for both local and systemic therapeutic purposes. The lungs offer a large surface area for drug absorption, making inhalation an attractive ROA for certain diseases. However, clinical use of this route presents distinct challenges, particularly in navigating the complex clearance mechanisms within the respiratory system. Mucociliary clearance and the activity of lung-associated macrophages (LAMs) represent significant obstacles to sustained nanoparticle retention in the lungs, reducing the efficacy of inhaled therapies.
For intra-articular delivery, nanoparticles are being increasingly explored for treating diseases like osteoarthritis, where direct drug delivery to affected joints can improve therapeutic outcomes while minimizing systemic exposure. Clinical trials with intra-articular nanoparticles have shown promise in targeting joint inflammation and cartilage degradation, yet translating these successes into widespread clinical practice is contingent on overcoming the anatomical and mechanical challenges posed by joint physiology.
Each ROA introduces unique variables that must be accounted for when designing clinical trials and evaluating nanoparticle efficacy. Selecting the appropriate route based on disease state, nanoparticle design, and patient factors is essential for optimizing therapeutic outcomes.
The Clinical Roadblock: Immune System Interactions and FDA Hurdles
At the clinical level, the most significant obstacle for nanoparticle-based therapeutics remains their rapid clearance by the immune system, limiting their therapeutic window. The mononuclear phagocyte system, which includes macrophages and other phagocytic cells, plays a central role in recognizing and eliminating nanoparticles from circulation. While surface modifications such as PEGylation can delay opsonization, the immune system’s adaptability often leads to eventual nanoparticle clearance, reducing the therapeutic efficacy.
Moreover, despite significant research investment, only a few nanoparticle-based drugs have successfully navigated the stringent approval process of regulatory bodies like the FDA. The rigorous requirements for demonstrating safety, consistency in manufacturing, and clinical efficacy create substantial hurdles for developers. In particular, the lack of robust, predictive preclinical models that can reliably forecast human immune responses remains a critical bottleneck.
To overcome these challenges, the clinical development pipeline for nanoparticles must incorporate more sophisticated models for evaluating immune system interactions. Simultaneously, advancements in nanoparticle characterization and manufacturing must ensure that the therapeutic properties of these systems are maintained throughout the drug development process.
A Clinical Perspective on Nanoparticle Drug Delivery
The translation of nanoparticle technology from bench to bedside requires a nuanced understanding of both their physicochemical properties and their interactions with human biology. While preclinical models provide valuable insights into nanoparticle performance, their limitations highlight the need for clinical trials that can more accurately predict human responses. As nanoparticle technologies continue to evolve, it is critical to refine the design and evaluation of these systems to ensure their success in clinical settings. Bridging the gap between preclinical promise and clinical reality will ultimately determine the future of nanoparticles as a cornerstone of modern medicine.
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts

Medicinal Chemistry & Pharmacology
Aerogel Pharmaceutics Reimagined: How Chitosan-Based Aerogels and Hybrid Computational Models Are Reshaping Nasal Drug Delivery Systems
Simulating with precision and formulating with insight, the future of pharmacology becomes not just predictive but programmable, one cell at a time.

Medicinal Chemistry & Pharmacology
Coprocessed for Compression: Reengineering Metformin Hydrochloride with Hydroxypropyl Cellulose via Coprecipitation for Direct Compression Enhancement
In manufacturing, minimizing granulation lines, drying tunnels, and multiple milling stages reduces equipment costs, process footprint, and energy consumption.

Medicinal Chemistry & Pharmacology
Decoding Molecular Libraries: Error-Resilient Sequencing Analysis and Multidimensional Pattern Recognition
tagFinder exemplifies the convergence of computational innovation and chemical biology, offering a robust framework to navigate the complexities of DNA-encoded science
Read More Articles
Magnetic Nanoengineering: Overcoming Biological Variability and Enhancing Therapeutic Precision
The future of nanomedicine lies in harmonizing precision, accessibility, and ecological responsibility, ushering in an era where therapies are tailored to individual biological landscapes.
Trials, Triumphs, and Trials Ahead: Navigating the Landscape of Randomized Controlled Trials in Artificial Intelligence-Driven Healthcare
The adoption of artificial intelligence in clinical practice has prompted a surge in randomized controlled trials, highlighting a balance of enthusiasm and prudence.
Illuminating the Dark Genome: Uncharted Frontiers in Therapeutic Discovery
The dark genome is not a biological void but a frontier awaiting illumination.