For most of the world, the Omicron variant of COVID-19 has largely come and gone – with severe spikes in infection, but overall showing a lower capacity for hospitalization and mortality. With the coming of spring in 2022 however, we have seen new outbreaks, providing cause for concern. Great Britain has reported surges in cases, while China has enforced unprecedented measures not seen since the first year of the pandemic. Amidst this growth in cases, observers ask whether the alarm should once again be raised – while research and innovation on all aspects of the disease continues, hoping to stave off future waves.
Delayed Outbreaks
After the spread of the novel coronavirus from Wuhan in 2019, China adopted a stringent policy to eliminate the virus from its territory – dubbed the Zero Tolerance approach. The strategy involves isolation, targeted testing and tracing of contacts, as well as movement restrictions. Strict punishments are implemented against not only individuals who fail to adhere to these guidelines, but also authorities that do not enforce them effectively. This approach worked for the last two years – if Chinese figures are to be believed. That was up until now, with the Jilin province reporting the country’s first two deaths from coronavirus since January last year.This Omicron-driven outbreak is expected to test the feasibility of the zero tolerance policy to its limit. Chinese academics predict that the outbreak will be brought back in control in early April, if stringent curbs are enforced.
Yet cracks have begun to show in the political appetite for zero tolerance, with Xi Jinping already saying that the country should seek to have the maximum effect in lowering infections at the minimum cost – which is not the principle that has guided Chinese policy so far. The zero tolerance policy has already failed in Hong Kong, with Chinese medics having to be sent in to reinforce the city-state’s healthcare infrastructure. Horrific scenes of patients lying in wait outside hospitals show the challenges ahead. China’s policy of admitting every positive case to hospital – whether asymptomatic or mild – has already become unviable. Further changes in policy seem to be on the horizon in the face of these pressures.
The lesson from China and Hong Kong is singular: even the most stringent of measures do not prevent large outbreaks – instead, they delay them. This is similar to what was observed in Australia and New Zealand, countries better positioned to control the influx of people due to their lack of land borders. It is hard to disconnect a populous country with a market economy from outside contact, and new variants will eventually make their way there. Low rates of prior infection, compounded by low rates of vaccination among the elderly and extremely high population densities have resulted in a staggeringly high death rate in Hong Kong.
Waning Immunity
Meanwhile, Western countries are seeing subsequent waves of infection as the virus evolves while vaccine-induced immunity wanes. Great Britain has recorded substantial increases in infection rates – while Scotland expects to see a peak in hospital admissions. Similar patterns are observed across the world in South Korea, Italy, France, Germany, and others. This rise is attributed to the BA.2 variant of Omicron, which has also been detected in wastewater in the United States. This was previously utilized as an early indicator of Omicron, which may be predictive of an incoming outbreak – the magnitude of which cannot be estimated.
In the face of these challenges, many countries are pivoting towards further vaccination – with the UK announcing spring boosters for the vulnerable segments of its population. The BA.2 sub-variant of Omicron is up to 30% more infectious. This is combined with a widespread trend of relaxing non-pharmaceutical intervention policies, which may reinforce transmission. Even those not worried about the severity of Omicron warn against being too lax, with the ever-present potential for the emergence of a deadlier variant. While the West is preoccupied with the rising cost of living and the war in Ukraine, these observations encourage caution.
Continued Innovation
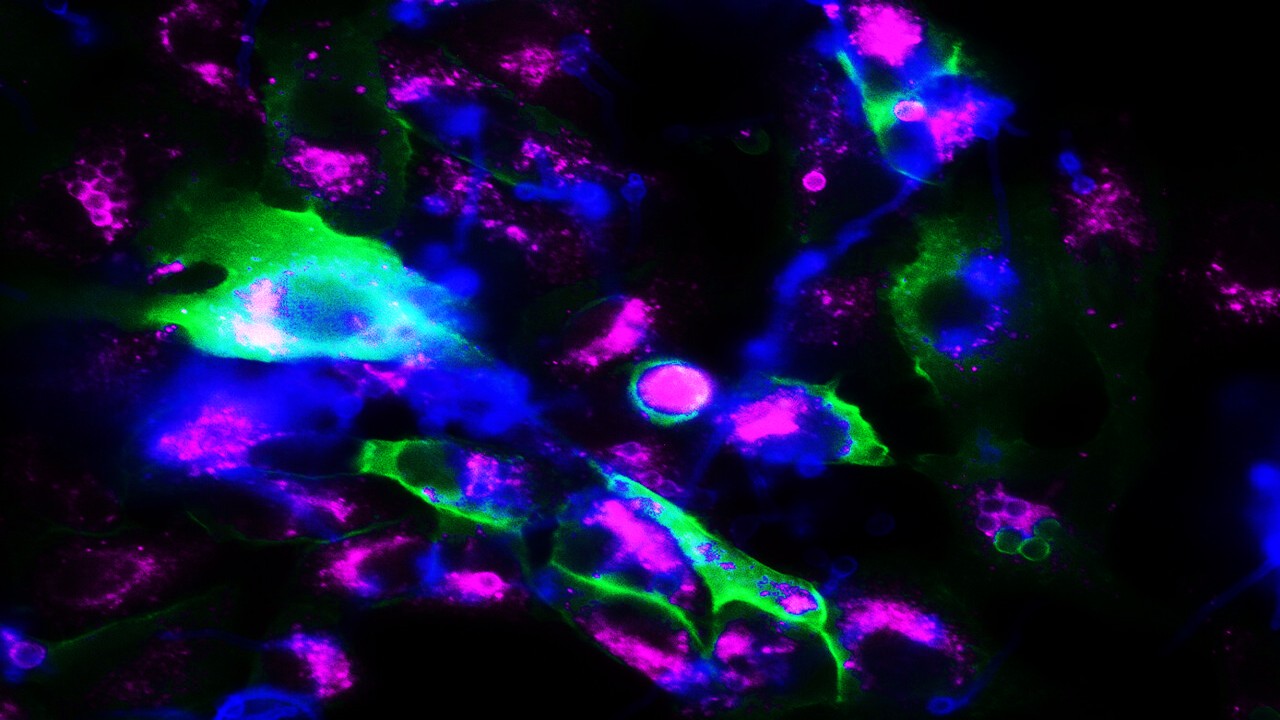
The importance of pharmaceutical interventions is only expected to increase as the world attempts to progress to a society with fewer social distancing measures. Research on all fronts is continuing. On monoclonal antibodies, AstraZeneca released new promising findings last week. Their combination therapy, Evusheld – made up of tixagevimab and cilgavimab, has shown effectiveness in lowering viral burden and lung inflammation in vivo. This activity was retained across all Omicron sub-variants. With monoclonal treatments in short supply, Evusheld can provide both prophylactic and therapeutic value to individuals who cannot be vaccinated – or are unlikely to respond well to infection.
The development of lower cost protein-technology vaccines continues, in hopes of increasing vaccine coverage in middle and lower income countries. New research has shown that a new protein vaccine produced in yeast can be effective in vivo models, with the potential to include a mosaic vaccine that can provide protection against multiple variants. This would allow the vaccine platform to rapidly keep pace with the changing nature of the COVID-19 pandemic, while the production in yeast can make use of existing infrastructure across the world, unlike novel, mRNA-based technologies.
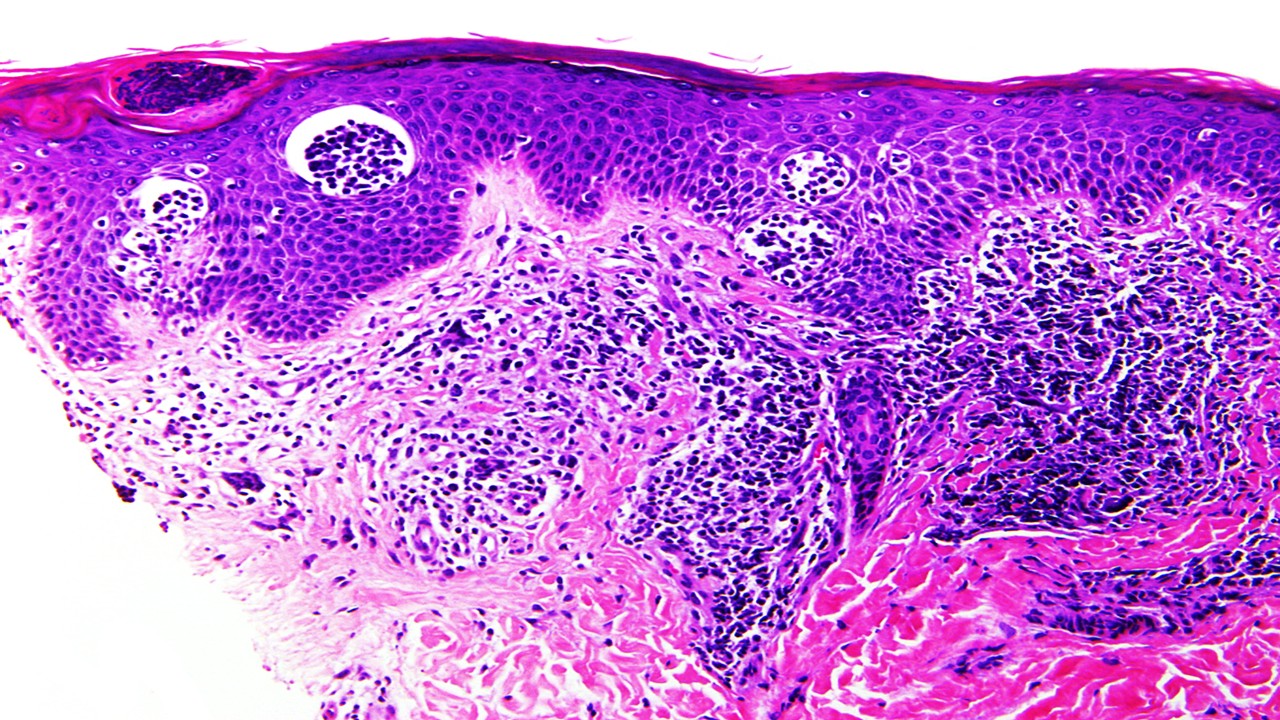
One of the constant worries in living with COVID is tackling long COVID efficiently. While some treatment options are being developed, our understanding of the syndrome is not yet complete. New research shows that immune dysfunction during infection can cause long-lasting, direct nerve damage in the peripheral nervous system. Such findings are congruent with symptoms such as muscle aches and pains reported by sufferers. Studies also previously showed the vaccinated are less likely to develop long COVID symptoms, suggesting that immune overreaction due to primary infection may be part of the reason for symptoms.
As our outlook on COVID changes, we must remain vigilant in our approach to neutralizing the pandemic. The zero tolerance, elimination-oriented strategies of countries such as China, Australia and New Zealand have been challenged – suggesting that living with COVID will be the new reality. Research and innovation will play a key part in making this reality liveable – with vaccines, treatments and continued investigations in understanding long COVID marking the three pillars that science is currently focusing on.
Nick Zoukas, Former Editor, PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts

Infectious Diseases & Vaccinology
Enduring Blockade: Five-Year Functional Antibody Persistence Against Emerging GII.4 and GII.17 Noroviruses
Natural infection with dominant GII noroviruses elicits long-lived functional antibodies, redefining immune durability in viral gastroenteritis.
Infectious Diseases & Vaccinology
Resistant Mycosis: Reimagining Antifungal Therapy Through Mechanistic Innovation and Molecular Disruption
Emerging antifungal strategies are redefining treatment by targeting fungal physiology through diversified, mechanism-driven approaches that overcome entrenched drug resistance.
Infectious Diseases & Vaccinology
Fungal Refractory States: Deciphering Pathobiology and Therapeutic Weaknesses in the Era of Rising Antifungal Resistance
Rising antifungal resistance reflects a multidimensional biological challenge that demands mechanistically innovative, host-integrated therapeutic strategies.

Infectious Diseases & Vaccinology
Epigenetic Parasite Vulnerabilities: Repurposing Histone Deacetylase Inhibitors for Complex Multispecies Therapeutics
Repurposed HDAC inhibitors target essential parasite epigenetic machinery, offering a powerful but complex frontier for next-generation antiparasitic therapy.
Read More Articles
Spatial Collapse: Pharmacologic Degradation of PDEδ to Disrupt Oncogenic KRAS Membrane Localization
PDEδ degradation disrupts KRAS membrane localization to collapse oncogenic signaling through spatial pharmacology rather than direct enzymatic inhibition.
Neumedics’ Integrated Innovation Model: Dr. Mark Nelson on Translating Drug Discovery into API Synthesis
Dr. Mark Nelson of Neumedics outlines how integrating medicinal chemistry with scalable API synthesis from the earliest design stages defines the next evolution of pharmaceutical development.
Zentalis Pharmaceuticals’ Clinical Strategy Architecture: Dr. Stalder on Data Foresight and Oncology Execution
Dr. Joseph Stalder of Zentalis Pharmaceuticals examines how predictive data integration and disciplined program governance are redefining the future of late-stage oncology development.
Exelixis Clinical Bioanalysis Leadership, Translational DMPK Craft, and the Kirkovsky Playbook
Senior Director Dr. Leo Kirkovsky brings a rare cross-modality perspective—spanning physical organic chemistry, clinical assay leadership, and ADC bioanalysis—to show how ADME mastery becomes the decision engine that turns complex drug systems into scalable oncology development programs.
Policy Ignition: How Institutional Experiments Become Durable Global Evidence for Pharmaceutical Access
Global pharmaceutical access improves when IP, payment, and real-world evidence systems are engineered as interoperable feedback loops rather than isolated reforms.







