The success of innovative vaccination developments with COVID-19 has renewed interest in tackling long-standing problems faced by vaccines for other diseases. Of particular interest are this week’s developments in Ebolavirus vaccines, as well as the progress made by T-cell priming vaccine candidates for COVID-19 and other diseases.
Double Acting Ebolavirus Vaccine Candidate
Ebola is a disease characterised by high fatality rates, owing to its life-threatening haemorrhagic fever symptoms. It is largely restricted to West Africa, with semi-frequent outbreaks. The virus does not persist in humans – indeed, that would be unsustainable given its mortality rate. Instead, the virus lives on in natural reservoir populations, such as fruit bats. Outbreaks only happen when a human population contracts the disease from its natural reservoir.
The disease is caused by six viruses in the Ebolavirus genus, with Zaire ebolavirus and Sudan ebolavirus being the most significant. Despite multiple outbreaks in the last decade, a vaccine that works for both the Zaire (Zaire ebolavirus) & Sudan (Sudan ebolavirus) species, has yet to be developed. Part of the reason development has been slow is due to the self-limiting nature of Ebola, and the speed with which it kills its victims, in addition to it being endemic to less developed parts of the world whose financial priorities are already stretched thin across myriads of other health concerns.
Nevertheless, multiple vaccination models are currently in development, with the rVSV-ZEBOV vaccine being the first to have obtained approval for use. However, the rVSV-ZEBOV vaccine, which is traded as ERVEBO, is primarily effective against the Zaire species of Ebola. The other vaccination which has been approved for use, Zabdeno/Mvabea, also only offers protection against Zaire ebolavirus and requires two doses. While the Zaire species is the most lethal, the Sudan species of Ebola is also of concern.
Researchers at the Jenner Institute of the University of Oxford, are currently commencing Phase I trials on a new vaccine which is hoped will be efficacious against both species of Ebola. The vaccine comes on the coat-tails of the COVID-19 vaccine (the AstraZeneca vaccine) developed at the University, which used similar technology. The new vaccine, ChAdOx1 biEBOV, will utilise a similar adenovirus vector to deliver the genetic material responsible for producing immunity against the two ebolaviruses.
Due to the regions Ebola is found in, the vaccine not only has to be effective biologically but also has to be able to work within the logistical framework and infrastructure of the area. As such, its storage requirements, shelf-life and cost of manufacture will be crucial in any endeavour to make a dent on the overall burden produced by Ebola. Considering these logistical challenges, the importance of a vaccine which is able to generate immunity against two species of ebola virus, rather than just one, cannot be understated.
T-Cell Based COVID Vaccines
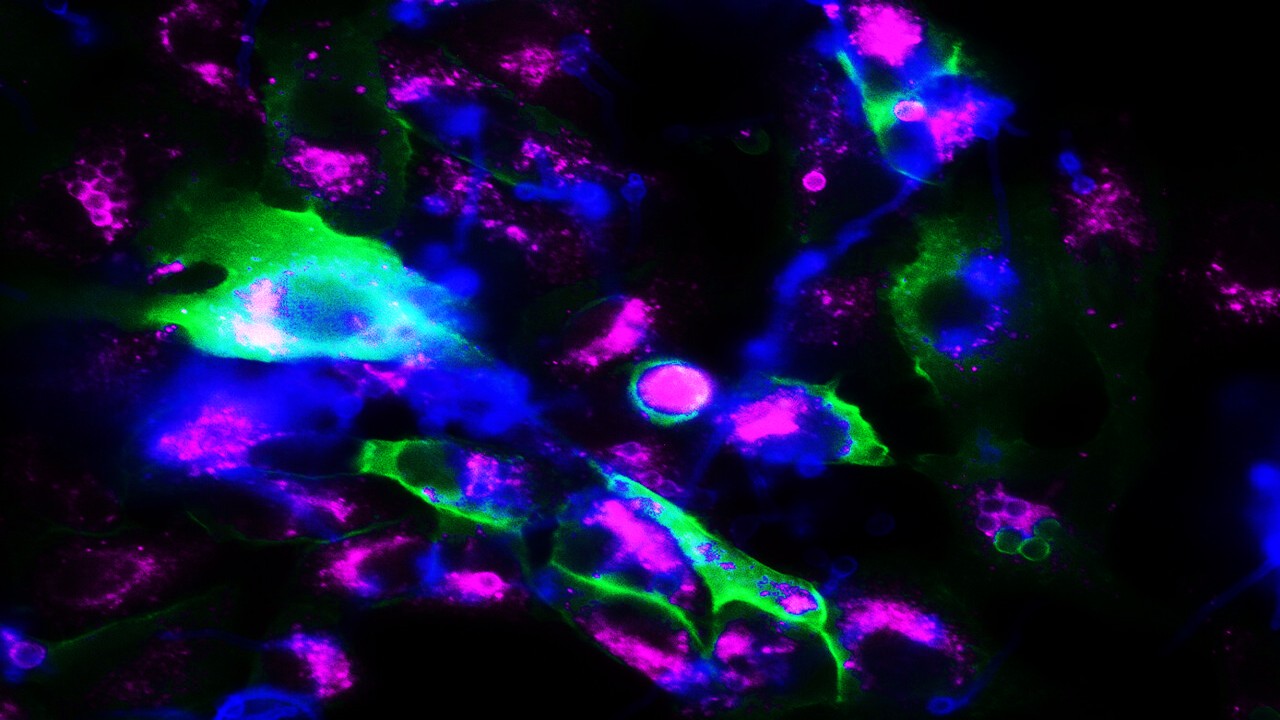
Continuing the trend of vaccine innovation sparked by COVID-19, British firm Emergex has commenced Phase I trials for T-cell priming vaccine candidates for COVID-19. Their proposed vaccines would function by priming the CD8+ T-cells to eliminate infected cells, rather than relying on antibodies as traditional vaccines do.
The most significant advantage of T-cell mediated immunity is that it is able to target highly conserved antigens, i.e. viral structures that do not change much as the virus evolves. In contrast, antibody-based vaccines can be rendered ineffectual against rapidly mutating viruses. Emergex hopes that this could lead to long-lasting immunity, that would confer robust protection against multiple variants of COVID-19. There has been a particularly acute need for innovation in this area, as the rapid evolution of COVID-19 over the course of the pandemic has been leading to worries about reduced vaccine efficacy.
Challenges in Dengue Fever (DENV) Vaccination
Emergex hopes to also develop vaccines based on similar technology for other diseases such as Influenza, Zika, Ebola & Dengue fever. Their Dengue fever candidate, naNO-DENGUE, will commence Phase I trials this January. Dengue fever is a disease caused by Dengue fever virus (DENV), which can be categorised into five serotypes. Infection with DENV provides lifelong immunity against the serotype an individual has been exposed to, but only short term immunity for any of the others.
This could be particularly useful as the sole Dengue fever vaccine currently in use (Dengvaxia) is only recommended for populations which have already had Dengue fever. In naive populations, the vaccine actually increases the risk of developing severe Dengue disease.Because Dengvaxia leads to the generation of antibodies that can react with multiple serotypes of DENV without necessarily neutralising the virus, it can lead to Antibody-Dependent Enhancement in individuals without prior exposure to DENV.
Antibody-Dependent Enhancement (ADE) is the phenomenon whereby non-neutralising levels of antibodies, generated by the immune system, could actually enhance the development of the disease in individuals without a history of exposure. DENV vaccine research has long been characterised by the struggle to find a balance between a vaccine being effective against all serotypes of DENV, while avoiding ADE. The technology proposed by Emergex may help overcome that, as it is not reliant on antibodies to begin with.
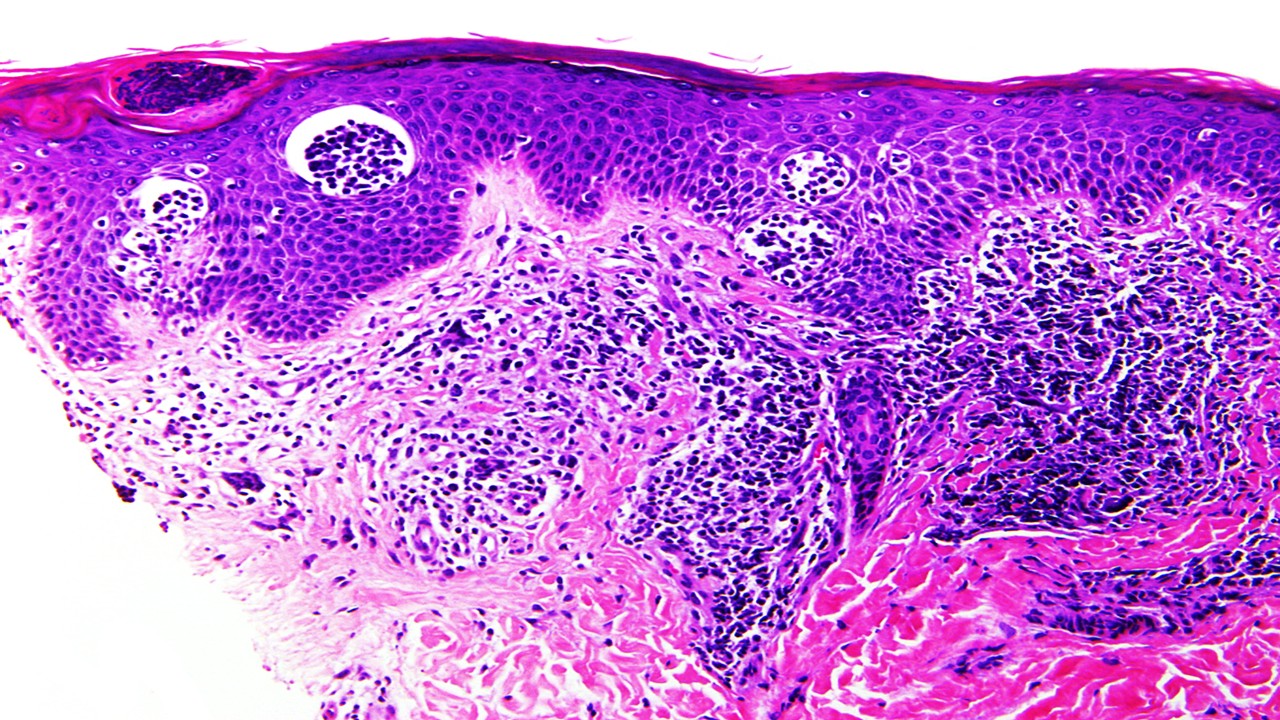
The mode of delivery for the T-cell priming vaccines by Emergex would also make administration much simpler. The proposed mechanism would be a skin-patch with microneedles that would deliver microparticles coated in peptides, which would generate the immune response. The skin patch would also have a shelf-life of months at room temperature, which would simplify logistics tremendously, particularly for the developing world.
Future Possibilities
It is expected that the effects of the pandemic on vaccine development will be long-lasting and wide-ranging. Indeed, prior to COVID-19, no mRNA vaccine had been approved for human use despite the first developments in the area starting around 2001. Due to the flexibility of mRNA vaccines and their ease of development, the possibilities that could be explored for benefits across a range of other diseases are endless. A similar trend is seen with viral vectored vaccines, the only one of which to have been approved prior to COVID-19 was Ervebo.
The trickle-down effects this spark of innovation will have on efforts to tackle other, more neglected, diseases, through vaccination cannot be underestimated. This is shown unmistakably in the above double acting Ebola vaccine. A similar effect may be seen with T-cell priming vaccinations, although the technology is much more novel. Regardless, the insights that their trials will garner into the functionality of vaccinations not relying on antibody-mediated responses can only be valuable.
Nick Zoukas, Former Editor, PharmaFeatures
Subscribe
to get our
LATEST NEWS
Related Posts

Infectious Diseases & Vaccinology
Enduring Blockade: Five-Year Functional Antibody Persistence Against Emerging GII.4 and GII.17 Noroviruses
Natural infection with dominant GII noroviruses elicits long-lived functional antibodies, redefining immune durability in viral gastroenteritis.
Infectious Diseases & Vaccinology
Resistant Mycosis: Reimagining Antifungal Therapy Through Mechanistic Innovation and Molecular Disruption
Emerging antifungal strategies are redefining treatment by targeting fungal physiology through diversified, mechanism-driven approaches that overcome entrenched drug resistance.
Infectious Diseases & Vaccinology
Fungal Refractory States: Deciphering Pathobiology and Therapeutic Weaknesses in the Era of Rising Antifungal Resistance
Rising antifungal resistance reflects a multidimensional biological challenge that demands mechanistically innovative, host-integrated therapeutic strategies.

Infectious Diseases & Vaccinology
Epigenetic Parasite Vulnerabilities: Repurposing Histone Deacetylase Inhibitors for Complex Multispecies Therapeutics
Repurposed HDAC inhibitors target essential parasite epigenetic machinery, offering a powerful but complex frontier for next-generation antiparasitic therapy.
Read More Articles
Spatial Collapse: Pharmacologic Degradation of PDEδ to Disrupt Oncogenic KRAS Membrane Localization
PDEδ degradation disrupts KRAS membrane localization to collapse oncogenic signaling through spatial pharmacology rather than direct enzymatic inhibition.
Neumedics’ Integrated Innovation Model: Dr. Mark Nelson on Translating Drug Discovery into API Synthesis
Dr. Mark Nelson of Neumedics outlines how integrating medicinal chemistry with scalable API synthesis from the earliest design stages defines the next evolution of pharmaceutical development.
Zentalis Pharmaceuticals’ Clinical Strategy Architecture: Dr. Stalder on Data Foresight and Oncology Execution
Dr. Joseph Stalder of Zentalis Pharmaceuticals examines how predictive data integration and disciplined program governance are redefining the future of late-stage oncology development.
Exelixis Clinical Bioanalysis Leadership, Translational DMPK Craft, and the Kirkovsky Playbook
Senior Director Dr. Leo Kirkovsky brings a rare cross-modality perspective—spanning physical organic chemistry, clinical assay leadership, and ADC bioanalysis—to show how ADME mastery becomes the decision engine that turns complex drug systems into scalable oncology development programs.
Policy Ignition: How Institutional Experiments Become Durable Global Evidence for Pharmaceutical Access
Global pharmaceutical access improves when IP, payment, and real-world evidence systems are engineered as interoperable feedback loops rather than isolated reforms.







