The regulation of hunger is greatly influenced by stomach hormones like ghrelin. The enteric nervous system, which regulates emotions of nausea, fullness, and appetite, contains the specialized endocrine cells that produce these hormones. MIT researchers have shown in a ground-breaking study published in Science Robotics that ingestible electroceutical capsules have the ability to stimulate these endocrine cells, increasing the synthesis of ghrelin. This cutting-edge technique has the potential to cure nauseating and vomiting-related illnesses including cachexia, which are frequently seen in cancer patients and other chronically ill people.
Electrical Stimulation and the Enteric Nervous System
The whole digestive process, including the passage of food through the gastrointestinal (GI) tract, is controlled by the enteric nervous system. Previous studies have demonstrated that electrical stimulation using implanted pacemaker-like devices relieved symptoms in patients with gastroparesis, a condition marked by delayed stomach emptying. At first, it was thought that the electrical stimulation encouraged stomach contractions, which aided in the movement of food. Researchers found that although being successful, the therapy had little influence on motility. The MIT researchers followed up on this finding by examining whether electrical stimulation may cause the hormone ghrelin, which is known to increase hunger and reduce motion sickness, to be released.
Probing Ghrelin Release
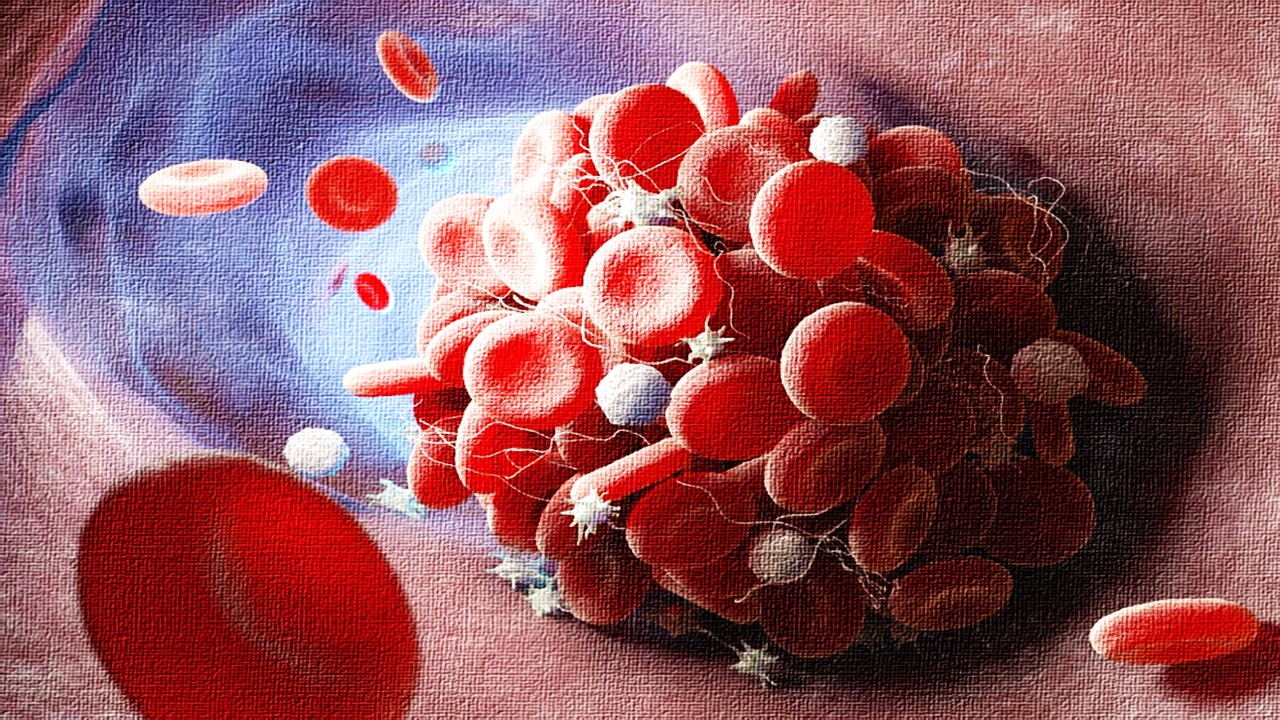
The researchers used an electrical probe to fire up the guts of animal models in order to test their theory. They saw a significant rise in circulating ghrelin levels after just a twenty-minute period of electrical stimulation. It’s important to note that the stimulation had no discernible negative effects or inflammation. The scientists decided to investigate the idea of deploying an ingestible device that may transitorily reside in the stomach and mimic the physiological effects of electrical stimulation as a result of these discoveries.
Designing the Ingestible Electroceutical Capsule
There were many difficulties in developing a device that could deliver electrical stimulation to the stomach. Making sure that the electrodes on the capsule could directly contact the stomach tissue notwithstanding an abundance of fluids was a crucial factor. The Australian prickly devil lizard uses scales with ridges to collect water, and this is how the researchers designed the capsule’s serrated surface. This surface draws moisture away from the electrodes, making the area dryer and better suited for reliable electrical stimulation. The fluid is moved out from the stomach tissue by channels that resemble those on a lizard’s skin, maintaining electrode contact. The prototype capsule additionally had battery-operated electronics that continuously generated an electric current. Future versions might include wireless control, enabling on-demand triggering.
Unlocking Hormonal Potential
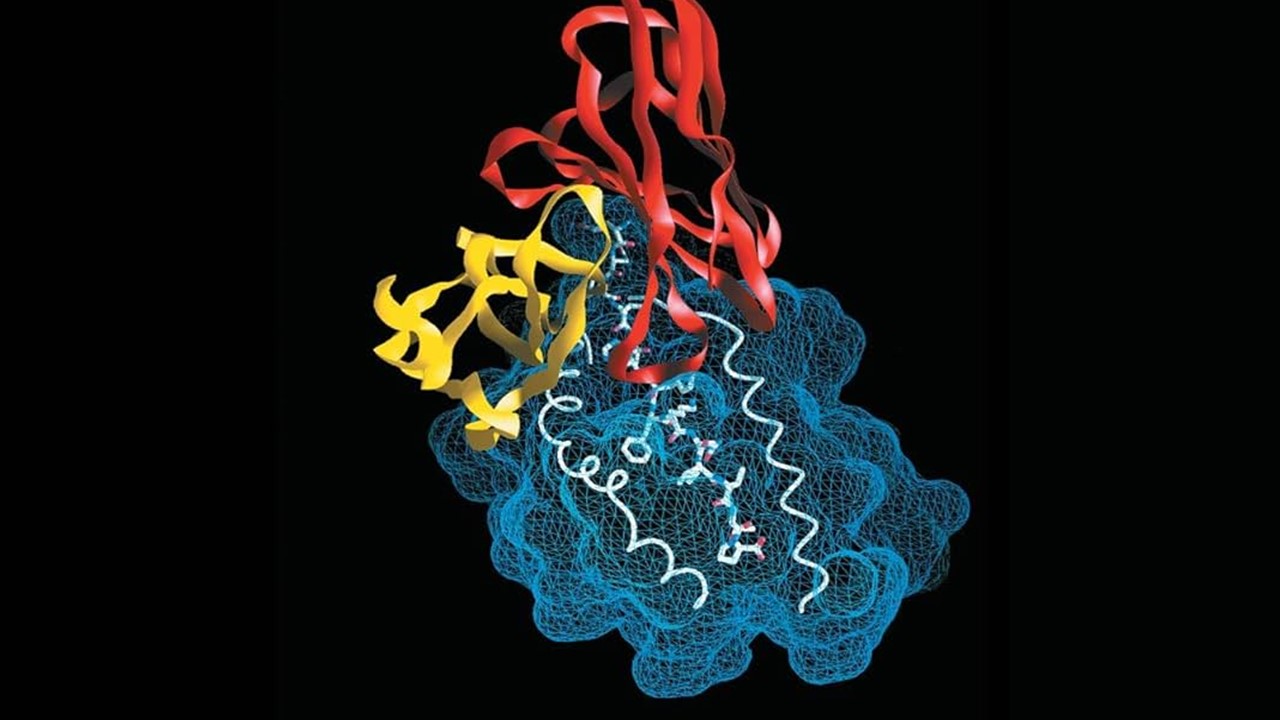
In animal experiments, the capsule was given to huge animals and a substantial increase in blood plasma ghrelin levels was observed. This revolutionary technique is the first time electrical stimulation delivered by an ingestible device has been used to boost endogenous hormone levels, using the body’s own mechanisms without incorporating xenobiotics. The researchers also found that the vagus nerve, which regulates digestion, is very important in this mechanism of stimulation. The brain is thought to receive the electrical pulses via the vagus nerve, which then activates the endocrine cells in the stomach to create ghrelin.
Future Implications and Conclusion
The MIT team wants to see if this method can be used in other parts of the alimentary tract, which could broaden its application in therapy. The scientists want to test the device on people within the following three years. If effective, this therapy might possibly take the place of or work in conjunction with already prescribed drugs for treating nausea and promoting appetite for individuals with cachexia or anorexia. The device’s simplicity points to a rather quick transition into human trials, opening the door for a thrilling future in electroceutical therapies.
This study was supported by grants from the National Cancer Institute, the National Institute for Diabetes and Digestive and Kidney Diseases, the Division of Engineering at New York University Abu Dhabi, a National Science Foundation graduate research fellowship, Novo Nordisk, and the Department of Mechanical Engineering at MIT.
In a nutshell this ground-breaking study shows how ingestible electroceutical capsules can alter hormones that control hunger, opening up a new treatment option for diseases of the appetite. Electroceuticals show potential for changing the therapeutic approach paradigm and utilizing the body’s inherent mechanisms for better health outcomes with additional research and development.
Study DOI: 10.1126/scirobotics.ade9676
Subscribe
to get our
LATEST NEWS
Related Posts

Pathophysiology & Experimental Medicine
Autism Disentangled: FOXG1 Drives Neural Imbalance in the Developing Brain
If FOXG1 overexpression can be modulated, either genetically or pharmacologically, it may be possible to correct the neurodevelopmental imbalances underlying ASD.
Pathophysiology & Experimental Medicine
Adaptive Interactions: How Stimuli-Responsive Materials Revolutionize Cellular Studies
Stimuli-responsive materials revolutionize cellular dynamics research by replicating ECM adaptability, unlocking insights into cell behavior and regulation.

Pathophysiology & Experimental Medicine
Eternal Lip Layers: Unlocking the Human Keratinocyte Potential
The lips, long celebrated for their role in communication and aesthetics, now stand at the forefront of scientific innovation.
Pathophysiology & Experimental Medicine
Thrombosis-Free Surfaces: Preventing Blood Clot Formation on Medical Implants Through Selective Protein Interactions
The synthesis and mechanisms of SPI coating are explored, evaluating its potential to overcome the limitations of traditional antifouling surfaces.
Read More Articles
Aerogel Pharmaceutics Reimagined: How Chitosan-Based Aerogels and Hybrid Computational Models Are Reshaping Nasal Drug Delivery Systems
Simulating with precision and formulating with insight, the future of pharmacology becomes not just predictive but programmable, one cell at a time.
Coprocessed for Compression: Reengineering Metformin Hydrochloride with Hydroxypropyl Cellulose via Coprecipitation for Direct Compression Enhancement
In manufacturing, minimizing granulation lines, drying tunnels, and multiple milling stages reduces equipment costs, process footprint, and energy consumption.
Decoding Molecular Libraries: Error-Resilient Sequencing Analysis and Multidimensional Pattern Recognition
tagFinder exemplifies the convergence of computational innovation and chemical biology, offering a robust framework to navigate the complexities of DNA-encoded science