Huntington’s disease, also known as Huntington’s chorea, is a progressive neurodegenerative disorder that affects the brain’s basal ganglia, leading to a wide range of motor, cognitive, and behavioral symptoms. The disease is named after George Huntington, who first described it in 1872. Huntington’s disease has a prevalence of 5-10 per 100,000 individuals worldwide, with a higher incidence in populations of European ancestry.
Symptomatology
Chorea (uncontrollable movements), dystonia (prolonged or twisting muscular contractions), rigidity, and bradykinesia (slowness of movement) are all symptoms of Huntington’s disease. Impaired executive function, attention, and working memory are examples of cognitive symptoms, while depression, anxiety, anger, and apathy are examples of behavioral symptoms. Patients may develop severe dementia as the condition worsens and need round-the-clock care.
Disease Genetics
The Huntingtin (HTT) gene, which is found on chromosome 4, is the source of the mutation that leads to Huntington’s disease. An aberrant form of the Huntingtin protein is produced as a result of the mutation, which entails the expansion of a CAG trinucleotide repeat in the gene.
The HTT gene typically contains between 10 and 35 CAG repeats. However, the number of CAG repeats in people with Huntington’s disease exceeds 36, and this excessive growth of the CAG repeat results in the development of a dangerous protein known as mutant Huntingtin (mHTT). The earlier the age of onset and more severe the symptoms of Huntington’s disease, the longer the CAG repeat.
In the brain, the mHTT protein builds up in neurons, causing malfunction and ultimately death. The distinctive physical and cognitive signs of Huntington’s disease are caused by the loss of neurons in specific areas of the brain, primarily the striatum. The mHTT protein accumulates in neurons in the brain, leading to their dysfunction and eventual death. The death of neurons in certain regions of the brain, particularly the striatum, leads to the characteristic motor and cognitive symptoms of Huntington’s disease.
The inherited form of Huntington’s disease is autosomal dominant. This means that regardless of whether they receive the healthy HTT gene from the other parent, a person with one copy of the mutant HTT gene will acquire Huntington’s disease. Therefore, there is a 50% probability that a kid of an affected parent will inherit the mutant HTT gene and get Huntington’s disease.
It is crucial to remember that not everyone with a mutated HTT gene will experience Huntington’s disease. Numerous variables, including the size of the CAG repeat, genetic modifiers, and environmental factors, can affect the development and course of the disease. These variables can affect the age of onset, severity, and progression of the disease in different people.
Molecular Pathophysiology
Huntington’s disease is a complex neurodegenerative disorder that involves multiple mechanisms leading to neuronal dysfunction and death. One of the key mechanisms involved in the development of the disease is the dysfunction of the Huntingtin protein, resulting from the expansion of the CAG trinucleotide repeat in the HTT gene. The mutant Huntingtin protein accumulates in neurons, forming aggregates and disrupting cellular processes, leading to neuronal dysfunction and death.
Cellular alterations, including oxidative stress, mitochondrial dysfunction, and inflammation, are a key factor in the development of Huntington’s disease. Reactive oxygen species (ROS) buildup, which can harm biological components like DNA, lipids, and proteins, is what leads to oxidative stress. Impaired energy metabolism, increased ROS generation, and apoptosis are all effects of mitochondrial malfunction. It involves the activation of immune cells and the release of pro-inflammatory cytokines, which can result in neuronal death. Inflammation is a reaction to tissue damage, infection, or injury.
Another important factor contributing to the onset of Huntington’s disease is transcriptional dysregulation, particularly when the CREB-binding protein (CBP) is involved. CBP is a transcriptional co-activator that interacts with DNA-binding transcription factors to control gene expression. In Huntington’s disease, the mutant Huntingtin protein prevents CBP from performing its job, which causes dysregulation of gene expression, particularly for genes essential for the survival and performance of neurons.
The combination of these mechanisms leads to the loss of neurons in the striatum, thalamus, and cerebral cortex, resulting in the characteristic clinical symptoms of Huntington’s disease, such as chorea, dystonia, rigidity, cognitive impairment, and psychiatric symptoms.
Diagnosing Huntington’s
Diagnosis of Huntington’s disease can be challenging, especially in the early stages, as the symptoms may be subtle and nonspecific. Diagnosis typically begins with a comprehensive medical history and neurological examination to assess the presence and severity of motor, cognitive, and psychiatric symptoms. Family history is also important, as a positive family history of Huntington’s disease increases the likelihood of an accurate diagnosis.
Huntington’s disease can be diagnosed via genetic testing for the CAG trinucleotide repeat expansion in the HTT gene. The genetic test has about 100% sensitivity and specificity, making it extremely accurate. In order to estimate a person’s likelihood of developing Huntington’s disease in the future, genetic testing can also be utilized on asymptomatic individuals who have a family history of the condition.
Preimplantation genetic diagnosis, which involves genetic testing of in vitro fertilized embryos to choose those without the disease-causing mutation for implantation, is one of the other diagnostic techniques. If a fetus has inherited the disease-causing mutation, prenatal diagnosis, which entails genetic testing of fetal cells acquired by amniocentesis or chorionic villus sampling, can be utilized to ascertain this.
Additionally, it’s crucial to rule out other diseases like Parkinson’s, Wilson’s, and spinocerebellar ataxias that might exhibit symptoms identical to those of Huntington’s disease. Additional testing may be required, including blood tests, specialized neurological examinations, and brain imaging. To guarantee an accurate diagnosis and suitable management, a multidisciplinary team approach combining neurologists, genetic counselors, and other medical experts is frequently required.
Pharmacologic Management and More
The management of Huntington’s disease is complex and requires a multidisciplinary approach. A range of strategies can be employed to manage symptoms and provide supportive care to patients with the disease.
The prevalence of chorea, which can be disabling and interfere with everyday activities, is one of the most critical obstacles in managing Huntington’s disease. Tetrabenazine is the most frequently prescribed prescription for the treatment of chorea, and it is normally used to manage the condition. Tetrabenazine is a reversible inhibitor of the solute carrier family 18 member 2 (SLC18A2) protein, sometimes referred to as the vesicular monoamine transporter 2 (VMAT2). It works by lowering dopamine levels in the brain, which can assist in chorea relief. Sedation, depression, and Parkinsonism are a few of the adverse effects that limit its use. Tetrabenazine’s effectiveness has been compared to that of deutetrabenazine, a more recently licensed medication with a superior side effect profile. Chemically speaking, deutetrabenazine is an isotopic isomer of tetrabenazine with six deuterium atoms in place of the hydrogen atoms. Deuterium’s presence decreases the degree at which drugs are metabolized, enabling less frequent dosage.
Additionally, benzodiazepines and antipsychotics can be used to lessen chorea, albeit they might have less pronounced impact on the signs and symptoms of Huntington’s disease. It has been demonstrated that atypical antipsychotics such risperidone and olanzapine can lessen chorea, but they also carry a higher risk of adverse effects like sleepiness, weight gain, and metabolic abnormalities. Although long-term usage of benzodiazepines, such as clonazepam, might result in tolerance, dependency and worsening of the depressive state, they may also be helpful for lowering chorea.
Levodopa or dopamine agonists are examples of antiparkinsonian drugs that may be helpful for patients with hypokinesia and stiffness. These drugs operate by raising dopamine levels in the brain, which helps some patients with their motor symptoms. They could, however, have unintended consequences like dyskinesia or a worsening of chorea.
Valproic acid may be useful in lowering the frequency and intensity of the movements in those with myoclonic hyperkinesia. The anticonvulsant medicine valproic acid is considered to function by raising the brain’s concentration of the neurotransmitter gamma-aminobutyric acid (GABA), which can assist to inhibit aberrant movements.
In addition, behavioral problems including sadness and psychosis can be treated with psychiatric drugs. Patients with Huntington’s disease may benefit from using mirtazapine and selective serotonin reuptake inhibitors (SSRIs) like fluoxetine to treat their depression. Quetiapine and aripiprazole are examples of atypical antipsychotics that may be useful in treating behavioral issues and psychotic symptoms, but they come with a higher risk of side effects than standard antipsychotics.
Rehabilitation therapies including physical therapy and speech and language therapy can be helpful in controlling the symptoms of Huntington’s disease in addition to pharmaceutical interventions. The quality of life as a whole, as well as speech and language abilities, can all be improved with the use of these services.
Ultimately, the management of Huntington’s disease is focused on improving symptoms and providing supportive care to patients and their families. It is important for patients to have access to a comprehensive care team that can provide a range of interventions to help manage their symptoms and improve their quality of life.
Prognosis & Current Research Directions
Huntington’s disease is a progressive and ultimately fatal disorder, and the prognosis for affected individuals is generally poor. The average lifespan after symptom onset is approximately 10-30 years, with death typically resulting from complications such as pneumonia or other infections.
The rate at which an illness progresses can, however, differ significantly between people. While some people’s symptoms may proceed relatively slowly, others may experience a more rapid course of the condition. The age at which symptoms first appear can also differ; whereas some people have symptoms as early as childhood or adolescence, others might wait until much later in life.
Despite the difficulties the disease presents, research is still being done to find novel cures and interventions that can slow or stop the disease’s course. The HTT gene and the ways in which mutant Huntingtin protein obstructs its normal operation are the subject of one area of study. Additionally, methods to speed up the clearance of mutant Huntingtin protein from the brain are being investigated.
Modulation of Huntingtin aggregation, which is thought to contribute to the onset of the disease, is a different area of study. Drugs that target Huntingtin aggregation may be able to slow or stop the evolution of the illness.
In addition to these strategies, scientists are also looking into how stem-cell therapy and regenerative medicine might be used to restore missing or injured neurons. Preclinical research has indicated that this strategy has potential, and there are now running clinical trials investigating the security and effectiveness of stem-cell treatment for Huntington’s disease.
Last but not least, a number of prospective treatments for Huntington’s disease are currently being studied in clinical trials, including medicines that focus on particular pathological features of the condition. These trials are designed to find novel medications that can reduce or stop the progression of disease and enhance the quality of life for those who are afflicted.
While the prognosis for individuals with Huntington’s disease remains poor, ongoing research provides hope for new treatments and interventions that could potentially slow or halt disease progression and improve outcomes for affected individuals and their families.
The CHDI Foundation
The CHDI Foundation was founded in 2003 with the mission of advancing the understanding and treatment of Huntington’s disease. The foundation is a non-profit organization that funds research programs focused on three main areas: disease biology, drug discovery, and clinical development. The ultimate goal of the foundation is to bring new treatments to patients as quickly as possible, and to improve the quality of life for individuals with Huntington’s disease and their families.
One of the main focuses of the CHDI Foundation is disease biology research, which aims to deepen our understanding of the underlying mechanisms of Huntington’s disease. This research involves the identification and characterization of new therapeutic targets, as well as the development of biomarkers to aid in clinical trial design and patient stratification. Some of the specific areas of research within disease biology include the role of mitochondrial dysfunction and oxidative stress in the disease process, as well as the cellular pathways involved in protein aggregation and clearance.
Another important area of focus for the CHDI Foundation is drug discovery. This involves the development of new compounds or therapies that can target the underlying mechanisms of Huntington’s disease. The foundation funds a variety of drug discovery programs, including high-throughput screening initiatives to identify new lead compounds, and the development of small molecules and biologics that target specific disease pathways. The foundation also works closely with pharmaceutical and biotech companies to facilitate the translation of promising drug candidates into clinical trials.
The CHDI Foundation is also actively involved in the clinical development of novel therapies for Huntington’s disease. This comprises developing patient registries and infrastructure for clinical trials in order to facilitate the recruitment and retention of study participants. It also includes the design and implementation of clinical trials. The foundation additionally promotes the creation of cutting-edge clinical endpoints and outcome metrics, which are essential for assessing the effectiveness of novel medicines in clinical trials.
In addition to its research programs, the CHDI Foundation also works to increase public awareness of Huntington’s disease and to improve the lives of individuals and families affected by the disease. This includes supporting patient advocacy organizations and providing educational resources for patients, families, and healthcare providers.
Conclusion
Huntington’s disease is a devastating neurodegenerative disorder with a well-established genetic component. Although there is currently no cure for the disease, management strategies are available to alleviate symptoms and improve quality of life. Ongoing research efforts offer hope for new treatments and interventions that can slow or halt disease progression, and the work of organizations such as the CHDI Foundation is crucial in accelerating progress towards these goals.
Subscribe
to get our
LATEST NEWS
Related Posts

Chronic & Debilitating Diseases
Renopathology Tipping Point: Deciphering the Molecular Code of Stage 2 Chronic Kidney Disease
The molecular events of Stage 2 CKD, from inflammation to lipid metabolism, offer insights for diagnosis and treatment.
Chronic & Debilitating Diseases
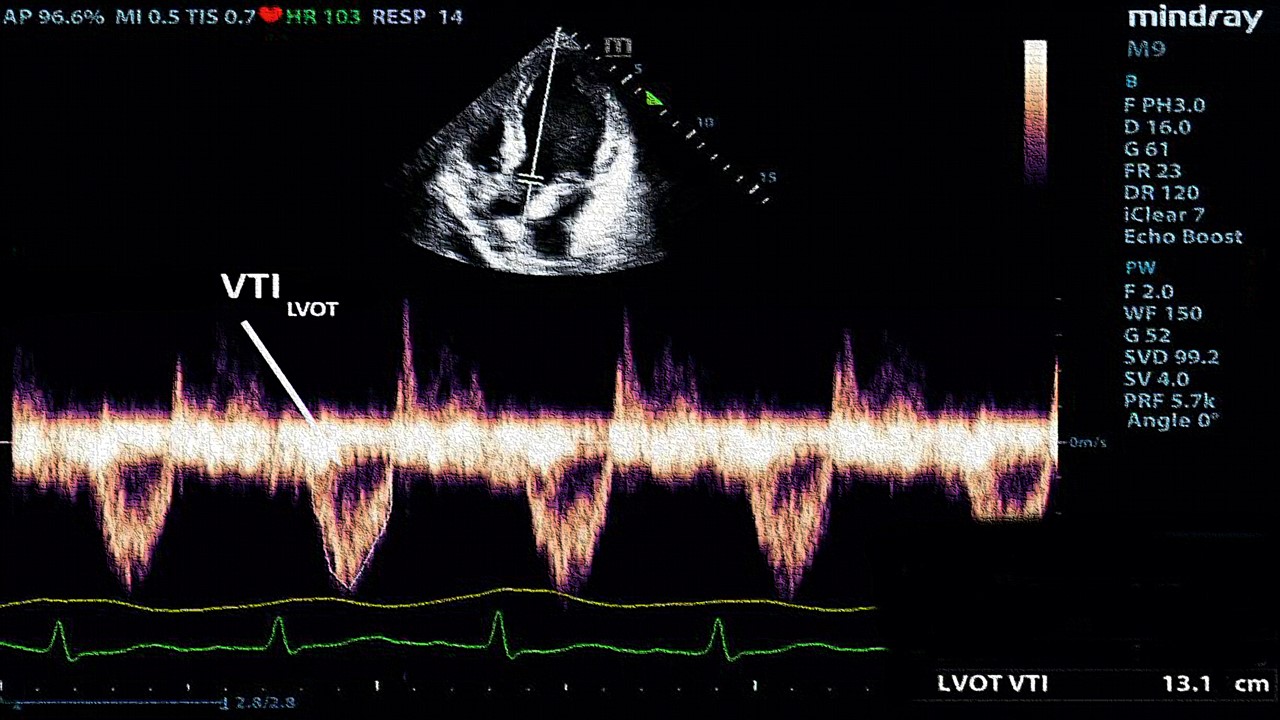
A New Lens on Shock: Hemodynamic Insights Through Critical Care Ultrasound
CCU has transformed the hemodynamic assessment of shock, delivering a reliable, reproducible, and non-invasive tool for ICU clinicians.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.