Systemic sclerosis (SSc), a severe rheumatic autoimmune disease, emerges with a high prevalence among women, affecting a striking number compared to men. The disease is marked by three primary characteristics—chronic inflammation, vascular abnormalities, and fibrosis—that collectively challenge the patient’s quality of life. These features progressively damage various internal organs, including the lungs, heart, gastrointestinal tract, and kidneys, leading to a debilitating decline in function and survival.
The exact triggers of systemic sclerosis remain a mystery, but there is growing evidence pointing to the immune system as a central player in its development. Patients with SSc display unique autoantibodies and cytokine profiles, suggesting immune cell activation as a key driver of the disease. Specifically, an imbalance in T helper cell cytokines—marked by elevated Th2 and suppressed Th1 activity—underscores the immune system’s role. Immune cells accumulate around blood vessels in the early stages, initiating damage to capillaries, which triggers pro-fibrotic pathways and an influx of inflammatory molecules. This cascading reaction underscores how immune responses not only contribute to inflammation but also escalate tissue fibrosis, the defining feature of SSc.
Immune System Pathways: The Engine of Inflammation and Fibrosis
The Role of Innate Immunity in Systemic Sclerosis
The innate immune system, the body’s first line of defense, is unusually active in SSc, with several immune cells abnormally present within affected tissues. In particular, macrophages, mast cells, and eosinophils appear to contribute to excessive fibrosis, the core of SSc pathology. Macrophages, known for clearing pathogens and aiding tissue repair, become altered in SSc, where they adopt a pro-fibrotic phenotype that releases cytokines such as IL-4, IL-6, and TGF-β. This cytokine cocktail spurs myofibroblasts—cells instrumental in creating and remodeling extracellular matrix (ECM)—to produce excessive fibrous tissue. These myofibroblasts further release growth factors and additional cytokines that amplify inflammation, creating a cycle of escalating fibrosis. In experimental models, reducing macrophage populations has been shown to mitigate fibrotic progression, highlighting their pivotal role in SSc.
Eosinophils, another cell type linked to innate immunity, are elevated in the blood of SSc patients, particularly in cases with interstitial lung disease and increased skin thickness. These cells respond to IL-4 and IL-13, suggesting their involvement in SSc inflammation and tissue remodeling. The precise mechanism by which eosinophils drive SSc-related fibrosis remains unclear, but evidence points to their ability to interact with other immune cells and contribute to the vascular and tissue abnormalities seen in SSc.
Adaptive Immunity and Fibrosis: T and B Cells as Key Actors
The adaptive immune system also plays a substantial role in SSc, particularly through T and B cells. Among T helper cells, the Th2 and Th17 subtypes have garnered significant attention. Th2 cells release IL-4 and IL-13, both of which are known to increase collagen production and ECM deposition. Th17 cells, meanwhile, secrete IL-17, a cytokine that amplifies fibroblast proliferation and promotes further inflammatory signals, feeding into the fibrotic cycle. In contrast, Th1 cells, which produce anti-fibrotic IFN-γ, are suppressed in SSc, tilting the balance in favor of fibrosis.
Additionally, regulatory T cells (Tregs) usually help prevent autoimmune responses, but in SSc, their numbers and effectiveness are often reduced, diminishing the body’s capacity to counteract fibrosis. Advances in technology, like single-cell RNA sequencing, have unveiled specific T cell types unique to SSc, pointing to personalized therapeutic targets.
B cells also exhibit dysregulated activity in SSc, producing autoantibodies such as anti-DNA topoisomerase I, anti-centromere, and anti-RNA polymerase. These autoantibodies are not only markers of the disease but are believed to actively drive fibrosis by transforming fibroblasts into a more pro-fibrotic state. Effector B cells in SSc release IL-6, a pro-fibrotic cytokine, while regulatory B cells, which have anti-inflammatory properties, are diminished, further intensifying the immune imbalance.
Current Treatment Landscape: Standard Approaches and Limitations
Broad-Spectrum Immunosuppressive Agents
Given SSc’s complex and multisystemic nature, treatments are often limited to broad-spectrum immunosuppressants such as corticosteroids, methotrexate, cyclophosphamide (CYC), and mycophenolate mofetil (MMF). While these drugs offer symptomatic relief, particularly in managing inflammation and fibrosis, their effects on halting disease progression remain limited.
Corticosteroids, a traditional mainstay, have shown potential in alleviating joint and muscle inflammation but carry risks, including scleroderma renal crisis when used at high doses. Methotrexate, though widely used in autoimmune conditions, has shown mixed results in SSc trials.
Cyclophosphamide has demonstrated modest improvements in lung function but is associated with severe side effects, often limiting its use. MMF has emerged as a favorable option, particularly for patients with lung involvement, but like other broad-spectrum agents, its ability to fully reverse fibrosis is limited.
Targeted Immune-Based Therapies: B Cell and T Cell-Directed Approaches
Recent advancements in immune-targeted therapies have introduced new hope for SSc treatment. Rituximab, a monoclonal antibody that targets CD20+ B cells, has shown promise in reducing skin fibrosis and preserving lung function in SSc, though it is less effective against plasma cells. Other B cell-targeting therapies like inebilizumab and belimumab have exhibited encouraging outcomes in early studies, suggesting they may offer more precise B cell depletion with potentially enhanced efficacy.
For T cells, abatacept has shown potential by deactivating CD28, a molecule essential for T cell activation. While early studies suggest abatacept can reduce fibrosis, especially in patients with higher inflammatory markers, larger trials are needed to validate these findings. Additionally, cytokine-targeting therapies such as tocilizumab, which blocks IL-6, have demonstrated promise in preserving lung function but have shown limited efficacy in reducing skin fibrosis.
Emerging Therapeutics and Future Directions
Tyrosine Kinase Inhibitors and Other Molecular Pathways
The discovery of tyrosine kinase inhibitors (TKIs) as potential treatments marks an exciting frontier in SSc therapy. Drugs like nintedanib, originally used for idiopathic pulmonary fibrosis, have shown effectiveness in slowing lung fibrosis in SSc patients. By targeting multiple pathways involved in fibroblast activation and immune cell signaling, TKIs represent a novel approach to addressing SSc’s multifaceted pathology.
Tofacitinib, a Janus kinase inhibitor, has also gained attention due to its anti-inflammatory properties, which downregulate IL-6 signaling. Early trials have indicated a potential for tofacitinib to reduce skin fibrosis, positioning it as a promising candidate for SSc treatment.
Autologous Stem Cell Transplantation: A Hopeful Yet Risky Option
Autologous hematopoietic stem cell transplantation (ASCT) is perhaps the most dramatic intervention available, offering the potential for long-term remission in severe SSc cases. By resetting the immune system, ASCT can reverse skin fibrosis and improve organ function, though it comes with significant risks, including infection and a high mortality rate. For patients with early and aggressive disease, ASCT remains a powerful but carefully considered option.
Moving Toward Personalized Treatment in Systemic Sclerosis
Systemic sclerosis remains one of the most challenging autoimmune diseases, with its unique combination of immune dysregulation, vascular dysfunction, and fibrosis. While broad-spectrum immunosuppressive therapies offer some benefit, the need for more targeted approaches is clear. Advances in understanding the roles of B and T cells, cytokines, and signaling pathways have opened doors to novel therapeutics that may allow more precise and personalized interventions.
In the near future, a deeper molecular understanding of SSc will likely usher in tailored treatment strategies, potentially combining multiple targeted therapies to address the specific immune abnormalities driving each patient’s disease. By dissecting the complex immune landscape of SSc and translating these insights into practical, personalized therapies, researchers hope to transform the outlook for patients with this challenging condition, providing not only symptom relief but also a chance for long-term disease control.
Study DOI: https://doi.org/10.3390/biomedicines10020316
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES
Register your interest [here] at Proventa International’s Clinical Operations and Clinical Trials Supply Chain Strategy Meeting this 14th of November 2024 at Le Meridien Boston Cambridge, Massachusetts, USA to engage with thought leaders and like-minded peers on the latest developments in the clinical space and regulatory affairs.

Subscribe
to get our
LATEST NEWS
Related Posts

Immunology & Oncology
The Silent Guardian: How GAS1 Shapes the Landscape of Metastatic Melanoma
GAS1’s discovery represents a beacon of hope in the fight against metastatic disease.
Immunology & Oncology
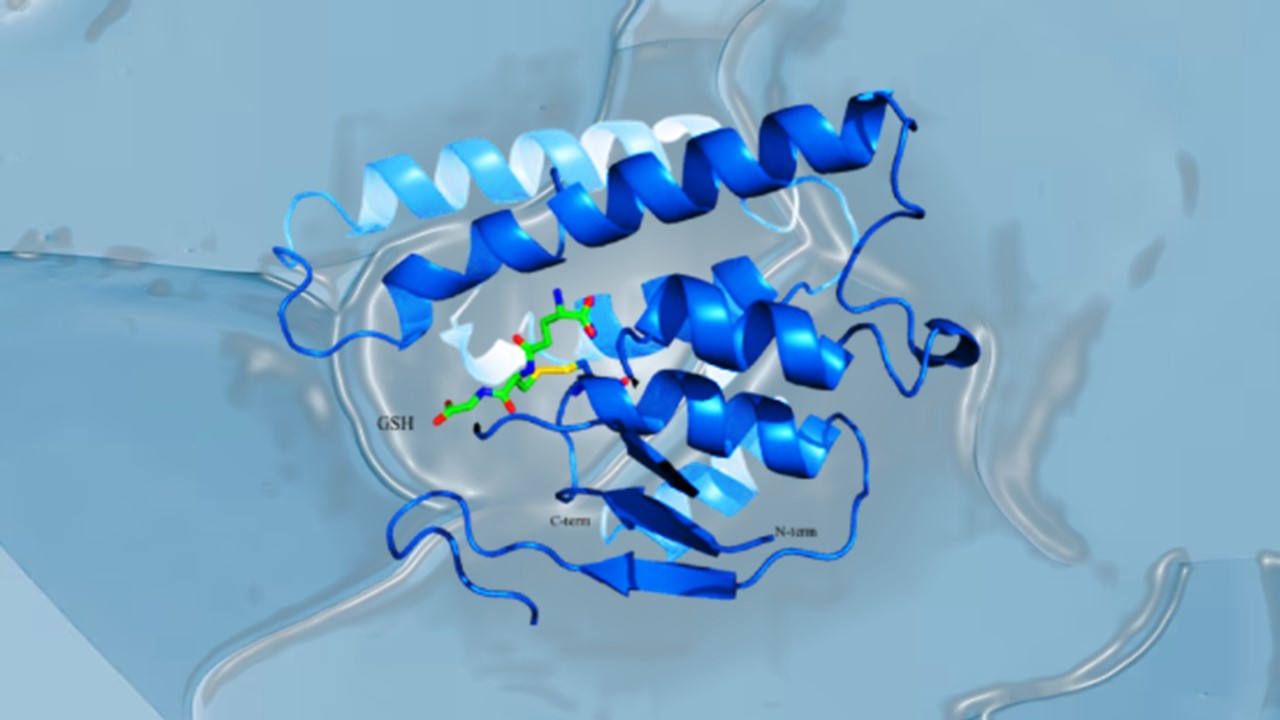
Resistance Mechanisms Unveiled: The Role of Glutathione S-Transferase in Cancer Therapy Failures
Understanding this dual role of GSTs as both protectors and accomplices to malignancies is central to tackling drug resistance.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.
Designing Better Sugar Stoppers: Engineering Selective α-Glucosidase Inhibitors via Fragment-Based Dynamic Chemistry
One of the most pressing challenges in anti-diabetic therapy is reducing the unpleasant and often debilitating gastrointestinal side effects that accompany α-amylase inhibition.