Renal, cardiovascular, and endocrine problems can all benefit from medications that affect the kidney. Sodium and water homeostasis are mostly affected by these illnesses. The proximal convoluted tubule (PCT), thick ascending limb (TAL), distal convoluted tubule (DCT), and cortical collecting tubule (CCT) of the nephron each have a unique mechanism for reabsorbing sodium and other ions. These nephron locations and processes serve as the foundation for the subgroups of diuretics that excrete salt. A few additional medications primarily affect water excretion. Knowing how the nephron segment in which they act functions allows us to predict how the diuretic drugs will behave.
Mechanisms of Renal Transport and Diuretic Pharmacology
At the glomerulus, the kidney acts as a filter to both plasma water and solutes at a blistering pace of 180 liters per day, and it is necessary to recover a sizeable portion of most of these chemicals before excretion in the urine. The four main tubular segments have different methods for reabsorption of salt and water, hence the diuretics operating in these segments have distinct mechanisms of pharmacologic activity. Most diuretics work by acting on the membrane’s luminal side. Spironolactone and eplerenone, which enter the collecting tubule cell from the basolateral side and attach to the cytoplasmic aldosterone receptor, are an exception to this rule.
Adenosine and prostaglandin receptors are widely distributed in the kidney. These receptors’ agonists and antagonists have the potential to directly affect renal function as well as the way the body reacts to diuretics. Glomerular filtration depends on prostaglandins to remain effective. The effectiveness of most diuretics declines when prostaglandin synthesis is decreased, as is the case with nonsteroidal anti-inflammatory medicines (NSAIDS). After the 20th week of pregnancy, the fetal kidney is primarily in charge of producing amniotic fluid; hence, whether or not a diuretic is being administered, pregnant women should not take NSAIDs after this point.
Proximal Convoluted Tubule
Amino acids, glucose, and many ions are isosmotically reabsorbed in the proximal convoluted tubule (PCT). The PCT is the primary location for reabsorption of sodium, chloride, and bicarbonate. In fact, a total of 60–70% of the sodium reabsorption occurs in the proximal tubule. However, t here are no medicines on the market right now that affect the proximal convoluted tubule’s ability to reabsorb sodium chloride (NaCl). The luminal membrane has a weak ability to reabsorb bicarbonate, but when bicarbonate is converted to carbon dioxide via carbonic acid, the carbon dioxide can be rapidly reabsorbed. The tubular cell could then synthesize bicarbonate from carbon dioxide and transport it into the interstitium. Meanwhile, sodium is recycled back from the lumen in exchange for hydrogen ions (NHE3 transporter), and the sodium-potassium pump (Na+/K+ ATPase) transports it into the interstitial space.
The target of carbonic anhydrase inhibitory xenobiotics is carbonic anhydrase, the enzyme necessary for the bicarbonate reabsorption process on the brush boundary and in the cytoplasm. The proximal tubule also actively secretes and absorbs weak acids and bases. The straight S2 section distal to the convoluted part is where the majority of weak acid transport takes place. Some of the medications used to treat gout target uric acid transport, which is particularly significant. The S1 and S2 segments transport weak bases. The sodium-glucose cotransporter (SGLT2) is in charge of reabsorbing glucose in the proximal tubule. SGLT2 inhibitors antagonizes the transporter and lowers blood sugar levels in diabetic patients
Carbonic Anhydrase Inhibitors
Acetazolamide serves as the model substance for carbonic anhydrase inhibitors. Sulfonamide derivatives make up these class of diuretics. Mechanistically, carbonic anhydrase is inhibited in the cytoplasm and brush border. Also present in various tissues, carbonic anhydrase is crucial for the production of aqueous humor and cerebrospinal fluid. All bodily tissues that contain acetazolamide have their carbonic anhydrase enzymes altogether inhibited.
Bicarbonate diuresis, or the significant excretion of sodium bicarbonate, is the primary renal consequence of carbonic anhydrase inhibition; as a result, the body’s supply of bicarbonate is reduced and metabolic acidosis develops. A large amount of potassium is lost as potassium is secreted and some excess sodium is reabsorbed as more sodium is supplied to the cortical collecting tubule. Because of bicarbonate depletion, sodium bicarbonate output slows, even when a diuretic is still being administered, and the diuresis ends after two to three days. Reduced bicarbonate secretion from the ciliary epithelium of the eye and the choroid plexus into the cerebrospinal fluid are also observed. It is possible to reduce intraocular pressure in the eye in a helpful way by exploiting this very mechanism. Hyperventilation caused by acidity of the cerebrospinal fluid in the central nervous system (CNS) helps prevent high-altitude sickness. There is no self-limitation to the effects on the cerebrospinal fluid and eyes.
Thick Ascending Limb of the Loop of Henle
The thick ascending limb (TAL) of the loop of Henle forces sodium, potassium, and chloride from the lumen into the kidney’s interstitium. It is also a significant site for the reabsorption of calcium and magnesium. A Na+/K+/2Cl– carrier (NKCC2), the target of loop diuretics, is responsible for reabsorbing sodium, potassium, and chloride. This cotransporter is in charge of reabsorbing 20–30% of the sodium filtered at the glomerulus and contributes to the concentration gradient for the kidney’s countercurrent concentrating process. A potassium-selective channel is used to pump potassium into the lumen because potassium is fed into the cell via the luminal and basal sides. A net positive charge is established in the lumen as a result of the absence of an anion from the potassium flowing through these channels. The calcium and magnesium are more easily reabsorbed thanks to this positive potential.
Loop Diuretics
The standard example of a loop diuretic agent is furosemide. Sulfonamide derivatives include furosemide, bumetanide, and torsemide. Although ethacrynic acid is not a sulfonamide and instead is a derivative of phenoxyacetic acid, it functions in a similar fashion. The cotransport of sodium, potassium, and chloride is inhibited by loop diuretics (NKCC2). The loop diuretics have a brief action time with observed diuresis usually happening over a 4-hour period following administration.
If glomerular filtration is adequate, a maximum dose of a loop diuretic results in a huge salt chloride diuresis. With this, blood volume may be greatly decreased as a consequence. Advantageously, e dema fluid is quickly expelled if tissue perfusion is adequate. The loop of Henle is where there is high urine dilution, which reduces the nephron’s capacity to dilute. The decrease of the lumen-positive potential caused by NKCC2 transporter inhibition also lowers the reabsorption of divalent cations. Calcium excretion is consequently markedly elevated. If blood volume is maintained, ethacrynic acid is a fairly effective uricosuric medication. Significant potassium loss and proton excretion may occur when high levels of sodium are presented to the collecting tubule. Another expected side effect following suit is hypokalemic alkalosis. The method by which loop diuretics lower pulmonary vascular pressures is unknown.
Distal Convoluted Tubule
Via the Na+/Cl– carrier (NCC), the distal convoluted tubule (DCT) actively removes sodium and chloride from the nephron lumen. Thiazide diuretics aim to inhibit this cotransporter. Five to eight percent of the body’s filtered sodium is reabsorbed through the DCT. In this renal section, calcium is also reabsorbed under the influence of parathyroid hormone (PTH).
Thiazide Diuretics
All of the other members of this group, including the standard thiazide diuretic hydrochlorothiazide, are sulfonamide derivatives. A few analogs that lack the characteristic thiazide ring in their structure are still regarded as thiazide-like because they produce outcomes that are equivalent to those of thiazides. Thiazides primarily prevent sodium chloride transport in the distal convoluted tubule’s first section. Thiazides are orally active and have an action period of 6–12 hours, which is significantly longer than other loop diuretics. The only thiazide diuretic that can be administered parenterally is chlorothiazide.
Thiazides generate a modest but long-lasting sodium and chloride diuresis when taken as directed. There could be a hypokalemic metabolic alkalosis as an expected side effect. Intracellular sodium is decreased when sodium transport from the lumen into the tubular cell is reduced, which encourages sodium-calcium exchange at the basolateral membrane. As a result, the impact of loop diuretics is reversed, with an increase in calcium reabsorption from the urine and a reduction in urine calcium content. Thiazides may impair water excretion and lead to dilutional hyponatremia because they work in a nephron segment that dilutes the body’s fluids. Thiazides also lower blood pressure, and their blood pressure-lowering effects are most pronounced at doses below those of diuretics. Compared to hydrochlorothiazide, chlorthalidone has a longer half-life and may be especially useful in treating hypertension. Thiazides are less effective when renal prostaglandin production is inhibited. A thiazide and a loop diuretic together have a synergistic effect that results in pronounced diuresis.
Cortical Collecting Tubule
Aldosterone, a steroid hormone released by the adrenal cortex, controls sodium reabsorption at the last tubular site of the nephron, which is the final section of the organ. Under typical conditions, this section reabsorbs 2-5% of the total sodium filtered; this percentage rises if aldosterone is elevated. The loss of potassium or hydrogen ions happens simultaneously with the reabsorption of sodium through epithelial sodium ion channels (ENaC), which are not transporters. Hence, the collecting tubule serves as both the last location for potassium excretion and the principal source of urine acidity. The potassium-sparing diuretics act at the aldosterone receptor and the ENaC sodium channels. Antidiuretic hormone regulates the medullary collecting tubule’s capacity to absorb water (ADH).
Potassium-Sparing Diuretics
Aldosterone is pharmacologically inhibited by the steroid derivatives spironolactone and eplerenone in the collecting tubules. These medications inhibit the expression of the genes that code for the ENaC and Na+/K+ ATPase by interacting with and inhibiting the intracellular aldosterone receptor. Triamterene and amiloride work by obstructing ENaC sodium channels. Spironolactone and eplerenone have sluggish onsets and offsets (1-3 days) of action. To note, these medications do not inhibit INa channels in excitable membranes. The duration of action for amiloride and triamterene is 12 to 24 hours. All medications in this family are potassium-sparing diuretics because they increase sodium clearance while decreasing potassium and hydrogen ion excretion. Hyperkalemic metabolic acidosis could result from administration of these diuretic class.
Osmotic Diuretics
The classic osmotic diuretic, mannitol, is administered intravenously. Glycerin, isosorbide (not isosorbide dinitrate), and urea are some additional medications that are frequently grouped with mannitol (but are rarely used). They persist in the lumen by virtue of their osmotic action because they are freely filtered at the glomerulus but poorly reabsorbed from the tubule. The proximal convoluted tubule is where most of this activity takes place. The collecting tubule and the descending limb of the loop of Henle both experience less water absorption. Urine production increases in volume. Unless they are actively reabsorbed, the majority of filtered solutes are expelled in greater levels. Sodium excretion is typically increased because sodium transporters are unable to handle the volume of urine flowing through the tubule at a fast enough rate. By osmotically drawing water from the tissue into the blood, mannitol can also lower brain volume and intracranial pressure. In the eye, a comparable process takes place.
SGLT2 Antagonists
The sodium-glucose cotransporter-2 (SGLT2) is crucial for the reabsorption of glucose by the kidneys. SGLT2 inhibitors (flozins or gliflozins) that have been approved for the treatment of diabetes include dapagliflozin, canagliflozin, empagliflozin, and ipragliflozin in Japan. They cause a 30–50% increase in excretion and a reduction in active reabsorption of filtered glucose in the proximal tubule. Except in diabetics with heart failure, they are not approved for use as diuretics even if they increase urine volume. Current research reveals that even in people without diabetes, they can reduce heart failure-related hospitalizations and deaths. The most effective gliflozins for SGLT2 inhibition, however, are empagliflozin and tofogliflozin. Empagliflozin, in particular, has been demonstrated to lower the risk of cardiovascular death. Evidently, urinary tract infections can arise from excessive glucose levels in the urine.
Vasopressin Agonists and Antagonists
Human vasopressin, also known as the antidiuretic hormone (ADH), and desmopressin are examples of typical ADH agonists. Being peptides, they must be administered parenterally. ADH antagonists include conivaptan and tolvaptan. Formerly, demeclocycline was employed as an antagonist. Although lithium has ADH antagonistic properties as well, it is never utilized for this purpose.
Human vasopressin stimulates V2 receptors, which in turn activate adenylyl cyclase via Gs. This helps water be reabsorb from the collecting tubule. As cyclic adenosine monophosphate (cAMP) levels rise, more aquaporin 2 (AQP2) water channels are inserted into the luminal membrane of this tubule pan. At V1a, conivaptan inhibits ADH. V2 receptors, are keenly inhibited as well. Tolvaptan has a lower affinity for V1 and is a more selective V2 blocker. Demeclocycline and lithium ostensibly prevent the insertion of water channels into the membrane while inhibiting the function of ADH at a point distal to the production of cAMP.
Antidiuretic Hormone Agonists
Arginine vasopressin (ADH) and desmopressin (ADH) raise urine concentration while decreasing urine volume. ADH and desmopressin are therefore helpful for treating pituitary diabetic insipidus, a condition involving ADH insufficiency. In the nephrogenic type of the disease (ADH resistance), they are useless, although salt restriction, water restriction, thiazides, and loop diuretics can be employed. These treatments lower blood volume, which stimulate proximal tubular reabsorption extremely strongly. Hence, in nephrogenic diabetes insipidus, increased water reabsorption in the proximal tubule partially compensates for the collecting tubule’s inadequate concentrating ability.
Vasopressin Antagonists
ADH blockers work to counteract the effects of vasopressin and other peptides found in nature that bind to the same V2 receptor as ADH. Such ADH-like peptides can significantly increase water retention and lead to serious hyponatremia. They are produced by some cancers, such as small cell lung carcinoma. Demeclocycline and conivaptan or tolvaptan are medications that can be used to treat this syndrome of inappropriate ADH secretion (SIADH), which results in hyponatremia. Although more toxic and never used for this indication, lithium also works. Several individuals with heart failure worsened by hyponatremia additionally benefit with conivaptan and tolvaptan usage outside of the recommended dosage range.
Toxicity
Having a lot of water in your system can result in serious hyponatremia if you have ADH or desmopressin present. Some people may get hypertension from taking large dosages of either peptide. If hyponatremia is cured too quickly, conivaptan and tolvaptan may cause demyelination with negative effects on the nervous system. Conivaptan may produce responses at the site of infusion. Demeclocycline, like other tetracyclines, can lead to abnormalities in the bones and teeth in children under the age of eight. Because of its various toxicities, lithium is never used to treat SIADH since it has the harmful consequence of causing nephrogenic diabetic insipidus.
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Subscribe
to get our
LATEST NEWS
Related Posts

Medicinal Chemistry & Pharmacology
Aerogel Pharmaceutics Reimagined: How Chitosan-Based Aerogels and Hybrid Computational Models Are Reshaping Nasal Drug Delivery Systems
Simulating with precision and formulating with insight, the future of pharmacology becomes not just predictive but programmable, one cell at a time.

Medicinal Chemistry & Pharmacology
Coprocessed for Compression: Reengineering Metformin Hydrochloride with Hydroxypropyl Cellulose via Coprecipitation for Direct Compression Enhancement
In manufacturing, minimizing granulation lines, drying tunnels, and multiple milling stages reduces equipment costs, process footprint, and energy consumption.

Medicinal Chemistry & Pharmacology
Decoding Molecular Libraries: Error-Resilient Sequencing Analysis and Multidimensional Pattern Recognition
tagFinder exemplifies the convergence of computational innovation and chemical biology, offering a robust framework to navigate the complexities of DNA-encoded science
Read More Articles
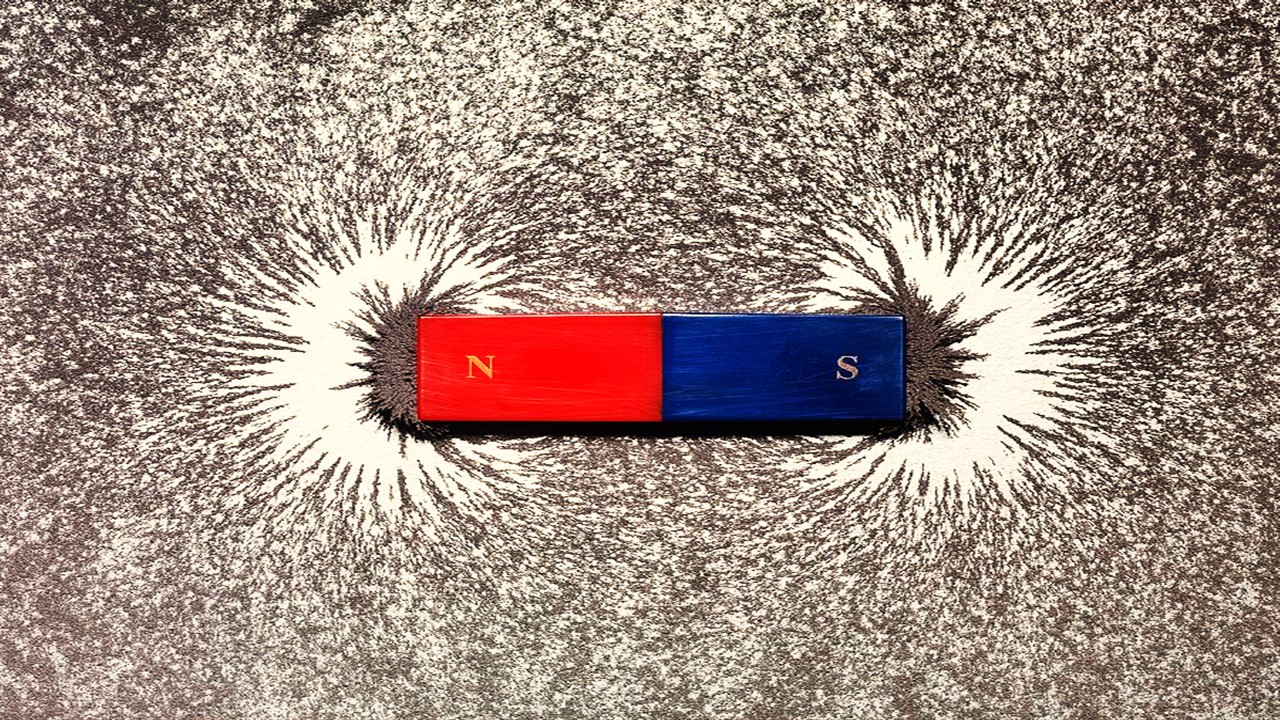
Magnetic Nanoengineering: Overcoming Biological Variability and Enhancing Therapeutic Precision
The future of nanomedicine lies in harmonizing precision, accessibility, and ecological responsibility, ushering in an era where therapies are tailored to individual biological landscapes.