The Extracellular Matrix: Tumor Architecture and a Barrier for Migration
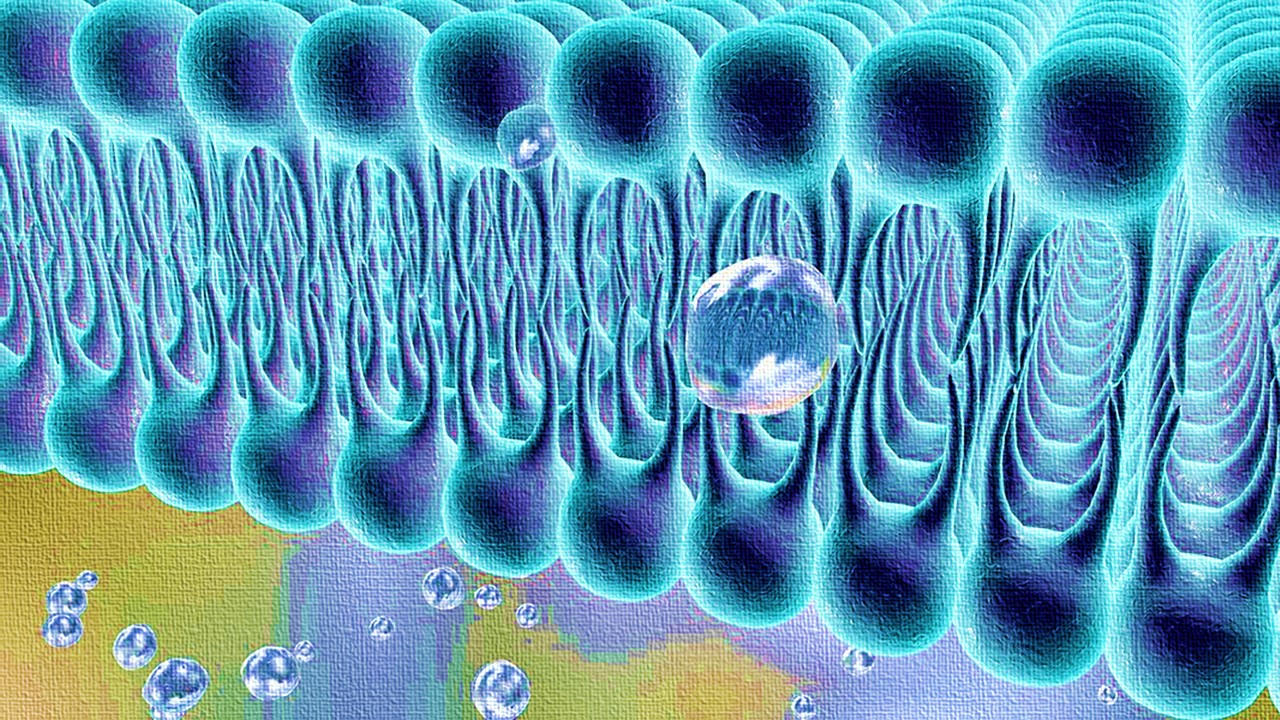
The extracellular matrix (ECM) is a dense, intricate mesh of proteins and glycosaminoglycans, providing physical support and biochemical signals to tissues. In cancer biology, its role extends far beyond structural scaffolding. Tumor cells encounter the ECM as a double-edged sword: a pathway for survival and proliferation or a physical constraint to invasion. ECM remodeling, previously understood as protein degradation at the tumor-stroma interface, now reveals a new dynamic: internalization of ECM components by invasive cancer cells. This study uncovers the crucial players orchestrating ECM endocytosis and links this process to the invasive migration of carcinoma cells.
ECM internalization occurs through macropinocytosis—a process of engulfing extracellular fluid and materials into large vesicles—and this activity is markedly elevated in aggressive cancer phenotypes. Through a pioneering high-content screening assay, scientists identified key regulators, specifically components of the mitogen-activated protein kinase (MAPK) pathway, α2β1 integrin, and protein phosphatase 2A (PPP2R1A). These components coordinate ECM uptake, lysosomal degradation, and subsequent cancer cell migration across diverse in vitro and in vivo platforms. Their findings point to a central axis—α2β1 integrin-p38 MAPK signaling—that drives ECM internalization and promotes invasive behavior, offering new insight into tumor progression and chemoresistance.
High-Content Screening Reveals MAPK Kinases as ECM Uptake Regulators
To understand how ECM internalization is regulated, researchers developed a high-content live-cell imaging assay. This method overcame limitations of traditional 2D culture models, which often overlook ECM dynamics. ECM components were fluorescently tagged with a pH-sensitive dye, enabling real-time visualization of trafficking through acidic endosomal compartments. Cancer cells were cultured on ECM substrates like Matrigel, collagen I, and cell-derived matrices (CDM) to simulate the tumor microenvironment.
By screening a library of 948 kinases and phosphatases, the study identified key positive regulators of ECM uptake, including MAP3K1, MAPK11 (p38β), and PPP2R1A. Knockdown of these genes impaired the internalization of ECM-bound α2β1 integrin. Interestingly, further inhibition of the p38 MAPK pathway disrupted macropinocytosis entirely, suggesting a dependency on MAPK signaling for ECM endocytosis.
The study’s secondary validation of hits revealed consistent involvement of MAP3K1 (a MAPK kinase kinase) and MAPK11 in ECM uptake. MAP3K1 appeared to act upstream of p38 signaling, while PPP2R1A, a scaffolding subunit of protein phosphatase 2A, modulated ECM uptake via its phosphatase activity. Together, these findings underscored a signaling network where α2β1 integrin triggers p38 activation to promote ECM internalization, fueling invasive cancer cell behavior.
Integrin-Dependent ECM Endocytosis: The α2β1-p38 Axis
Integrins—heterodimeric receptors composed of α and β subunits—mediate cell-ECM adhesion and activate intracellular signaling cascades. Among them, α2β1 integrin serves as the primary receptor for collagen I, a major ECM component in tumors. The study demonstrated that α2β1 integrin is indispensable for ECM endocytosis. Pharmacological inhibition or siRNA-mediated knockdown of α2 integrin impaired collagen I and CDM internalization across breast, ovarian, and pancreatic cancer cell lines.
The researchers observed that ECM-bound α2β1 integrin is internalized via macropinocytosis and trafficked through the lysosomal pathway for degradation. Importantly, α2 integrin co-localized with ECM components in early endosomes, suggesting a tightly regulated endocytic route. Inhibition of p38 MAPK signaling reduced internalized pools of α2 integrin and impaired dextran uptake, a hallmark of macropinocytosis. These results indicated that p38 acts downstream of α2β1 integrin to regulate ECM uptake.
Further experiments revealed that p38 MAPK phosphorylates sodium/proton exchanger 1 (NHE1), a well-established macropinocytosis regulator. Downregulation of NHE1 impaired ECM internalization and disrupted cancer cell migration, highlighting its role as a key effector downstream of α2β1-p38 signaling. Collectively, these findings position the α2β1-p38-NHE1 axis as a driver of ECM macropinocytosis, facilitating invasive tumor migration.
ECM Uptake Fuels Cancer Cell Migration and Invasion
Cell migration and invasion are hallmarks of cancer metastasis. Using live-cell imaging, researchers tracked cancer cells migrating on ECM substrates and observed that internalization of ECM occurred predominantly at the perinuclear region near the leading edge. Pharmacological inhibition or genetic knockdown of MAP3K1, MAPK11, PPP2R1A, or α2 integrin significantly reduced cell migration velocity and directional persistence.
This phenomenon was confirmed in multiple cancer models. In scratch-wound healing assays, inhibition of α2β1 integrin or p38 MAPK impaired collective cell migration in pancreatic ductal adenocarcinoma (PDAC) cells. Likewise, 3D culture systems revealed that ECM uptake regulators are essential for invasive behavior. MAP3K1 knockdown disrupted the morphology of multicellular protrusions, reducing the ability of cancer cells to invade 3D collagen matrices.
Further experiments linked ECM degradation in lysosomes to migration. Blocking lysosomal activity with inhibitors like bafilomycin A1 or E64d impaired cancer cell migration, indicating that lysosomal processing of internalized ECM is crucial for invasive movement. These findings suggest that ECM internalization supports migration not merely by remodeling the ECM barrier but also by providing metabolic or structural advantages to invasive cancer cells.
Clinical Implications: Chemoresistance and Poor Prognosis
Beyond its role in cancer cell invasion, ECM internalization was shown to correlate with chemoresistance and poor patient outcomes. Analysis of transcriptomic datasets revealed elevated expression of α2β1 integrin, MAP3K1, and MAPK11 in chemotherapy-resistant breast cancer tumors. Additionally, high levels of these genes correlated with reduced survival in pancreatic cancer patients, underscoring their clinical relevance.
In pancreatic tumors, where ECM deposition is excessive and fibrotic, α2β1 integrin expression was markedly elevated compared to healthy tissues. This overexpression correlated with poor prognosis, suggesting a functional role for ECM uptake in pancreatic cancer progression. Importantly, targeting the α2β1-p38 axis could provide a dual therapeutic benefit: impairing tumor invasion while sensitizing cancer cells to chemotherapy.
Ongoing clinical trials targeting p38 MAPK and integrin signaling support this notion. Combined therapies involving p38 inhibition and chemotherapeutic agents have shown promise in ovarian and breast cancers, while α2 integrin inhibitors are being tested in solid tumors. This study highlights the therapeutic potential of disrupting ECM macropinocytosis to limit tumor dissemination and improve treatment outcomes.
A New Paradigm in Tumor-ECM Interactions
This research uncovers an unappreciated facet of tumor biology: the internalization and degradation of ECM components via macropinocytosis, regulated by α2β1 integrin and p38 MAPK signaling. By enabling cancer cells to navigate dense ECM barriers and sustain invasive migration, ECM internalization emerges as a critical driver of tumor progression.
The α2β1-p38-NHE1 axis offers a promising target for therapeutic intervention, particularly in cancers with aggressive phenotypes and chemoresistant traits. As cancer therapies evolve, understanding the interplay between ECM dynamics and cellular signaling pathways will be essential to develop strategies that block metastasis—the ultimate cause of cancer-related mortality.
Study DOI: https://doi.org/10.1371/journal.pbio.3002930
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES

Subscribe
to get our
LATEST NEWS
Related Posts

Immunology & Oncology
The Silent Guardian: How GAS1 Shapes the Landscape of Metastatic Melanoma
GAS1’s discovery represents a beacon of hope in the fight against metastatic disease.

Immunology & Oncology
Resistance Mechanisms Unveiled: The Role of Glutathione S-Transferase in Cancer Therapy Failures
Understanding this dual role of GSTs as both protectors and accomplices to malignancies is central to tackling drug resistance.