Owing to their invasive propensity and immunity to radiation therapy, gliomas, a kind of brain tumor, provide a considerable problem in the field of oncology. A potential advancement in the treatment of malignant tumors, however, has been highlighted by recent study that was published in the journal Clinical Cancer study. Zinc Finger MYND-Type Containing 8 (ZMYND8) is a gene that is epigenetically controlled in mutant Isocitrate Dehydrogenase 1 (IDH1) gliomas and is essential for fostering radioresistance, according to researchers at the University of Michigan Rogel Cancer Center. This finding opens up new possibilities for creating focused therapeutics that will improve the efficacy of radiation therapy for people with mutant IDH1 gliomas.
Gliomas: Genetics, Pathophysiology, and Classification
Gliomas are a diverse group of tumors that arise from glial cells, which are supportive cells of the central nervous system. These tumors can occur in various regions of the brain and spinal cord and are classified based on their histological features, genetic alterations, and clinical behavior. Understanding the genetics, pathophysiology, and classification of gliomas is crucial for accurate diagnosis, prognostication, and treatment planning.
Genomic alterations play a significant role in the development and progression of gliomas. Several genetic mutations have been identified in gliomas, and some of the most common and well-studied alterations involve genes such as Isocitrate Dehydrogenase 1 and 2 (IDH1/2), TP53, EGFR, PTEN, and TERT promoter. These mutations can affect key cellular processes, including DNA repair, cell cycle regulation, and signaling pathways, leading to uncontrolled cell growth and tumor formation.
The pathophysiology of gliomas is complex and involves a combination of genetic, epigenetic, and microenvironmental factors. Gliomas can arise from either astrocytes (astrocytomas) or oligodendrocytes (oligodendrogliomas), with some tumors showing mixed features (mixed gliomas). The abnormal genetic alterations observed in gliomas result in dysregulated cellular pathways, increased cell proliferation, evasion of cell death, and angiogenesis. Additionally, gliomas often exhibit infiltrative growth, infiltrating nearby brain tissue, making complete surgical resection challenging and contributing to tumor recurrence.
Gliomal classification has undergone significant revisions in recent years, reflecting advances in our understanding of their molecular and genetic characteristics. The World Health Organization (WHO) classification system is widely used and categorizes gliomas into four major groups: diffuse gliomas (including diffuse astrocytoma, oligodendroglioma, and oligoastrocytoma), ependymomas, other gliomas (such as pilocytic astrocytoma and pleomorphic xanthoastrocytoma), and glioblastomas. Each category is further classified based on histological features and molecular markers.
In the updated WHO classification, molecular markers have gained increasing importance in glioma classification. For instance, the IDH mutation status, 1p/19q codeletion, and the presence of other genetic alterations are now used as essential diagnostic and prognostic markers. This molecular information provides additional insights into the underlying biology of the tumors and can help guide treatment decisions. Furthermore, the integration of molecular and genetic features has led to the identification of specific glioma subtypes with distinct clinical behaviors and treatment responses. For example, IDH-mutant gliomas with 1p/19q codeletion have a better prognosis and are more responsive to certain chemotherapy regimens, whereas IDH-wildtype gliomas often exhibit a more aggressive clinical course.
The Persistence of Mutant IDH1 Glioma
Generally speaking, patients with IDH1-mutated gliomas have higher survival times than those without the mutation. Although the prognosis was initially positive, these cancers frequently recur in a more aggressive form and show resistance to radiation treatment. The elimination of radioresistance is a key objective in the treatment of gliomas, and the discovery of ZMYND8 as a possible therapeutic target offers promise for better therapeutic approaches.
Uncovering ZMYND8’s Role in Glioma
ZMYND8 is overexpressed in mutant IDH1 glioma cells, according to extensive experiments using human cell cultures and a cutting-edge animal model. Notably, they discovered that suppressing ZMYND8 expression made glioma cells more susceptible to radiation therapy, indicating that ZMYND8 plays a crucial role in modulating radioresistance.
Radiation therapy works by causing DNA damage in cancer cells, and ZMYND8 is a well-known regulator of DNA damage response. The scientists found that increased ZMYND8 protein expression in mutant IDH1 gliomas resulted in resistance to radiation therapy. Radiation therapy, however, caused considerable DNA damage and elevated cell mortality in glioma cells when ZMYND8 was silenced.
Validation in a Mouse Model
The researchers created a mouse model of a mutant IDH1 glioma in order to further demonstrate the importance of ZMYND8 in glioma radioresistance. ZMYND8 was knocked out in this model, improving survival by making the tumors more responsive to radiation therapy. These results support the possibility of targeting ZMYND8 as a workable strategy to improve radiation therapy efficacy in patients with mutant IDH1 glioma.
Combination Therapy Potential
Building upon their observations, the researchers explored the possibility of combining ZMYND8 knockdown with other cancer drugs, such as PARP (poly ADP [adenosine diphosphate]-ribose polymerase) inhibitors and HDAC (Histone deacetylases) inhibitors. Encouragingly, they found that these combinations synergized, making the glioma cells more responsive to radiation. This discovery suggests the potential for a combination therapy approach in the treatment of mutant IDH1 glioma.
Future Directions
While further research is necessary to fully harness the therapeutic potential of ZMYND8, the findings from this study lay the groundwork for developing innovative treatment strategies. Looking ahead, Dr. Maria G. Castro, the senior author of the study, envisions collaborating with colleagues at the U-M Biointerfaces Institute to design RNA-based inhibitors that can specifically target ZMYND8. To overcome the challenge of delivering these inhibitors across the blood-brain barrier, which protects the brain from harmful substances, the researchers plan to utilize nanoparticles, a technique they have already explored in previous studies. This multidisciplinary approach holds promise for the development of novel therapies that can effectively downregulate ZMYND8 expression and render mutant IDH1 glioma cells radiosensitive.
The identification of ZMYND8 as an epigenetically regulated gene in mutant IDH1 glioma marks a significant step forward in understanding the mechanisms underlying radioresistance in these tumors. By targeting ZMYND8 and combining it with other drugs, researchers may be able to enhance the efficacy of radiation therapy and improve outcomes for patients. This groundbreaking research not only provides valuable insights into the biology of mutant IDH1 glioma but also opens up exciting possibilities for the development of personalized treatment strategies in the future.
Through ongoing research and clinical trials, we move closer to a future where patients with mutant IDH1 glioma can benefit from more effective treatment options and improved survival rates.
Study DOI: 10.1158/1078-0432.CCR-22-1896
Subscribe
to get our
LATEST NEWS
Related Posts

Immunology & Oncology
The Silent Guardian: How GAS1 Shapes the Landscape of Metastatic Melanoma
GAS1’s discovery represents a beacon of hope in the fight against metastatic disease.
Immunology & Oncology
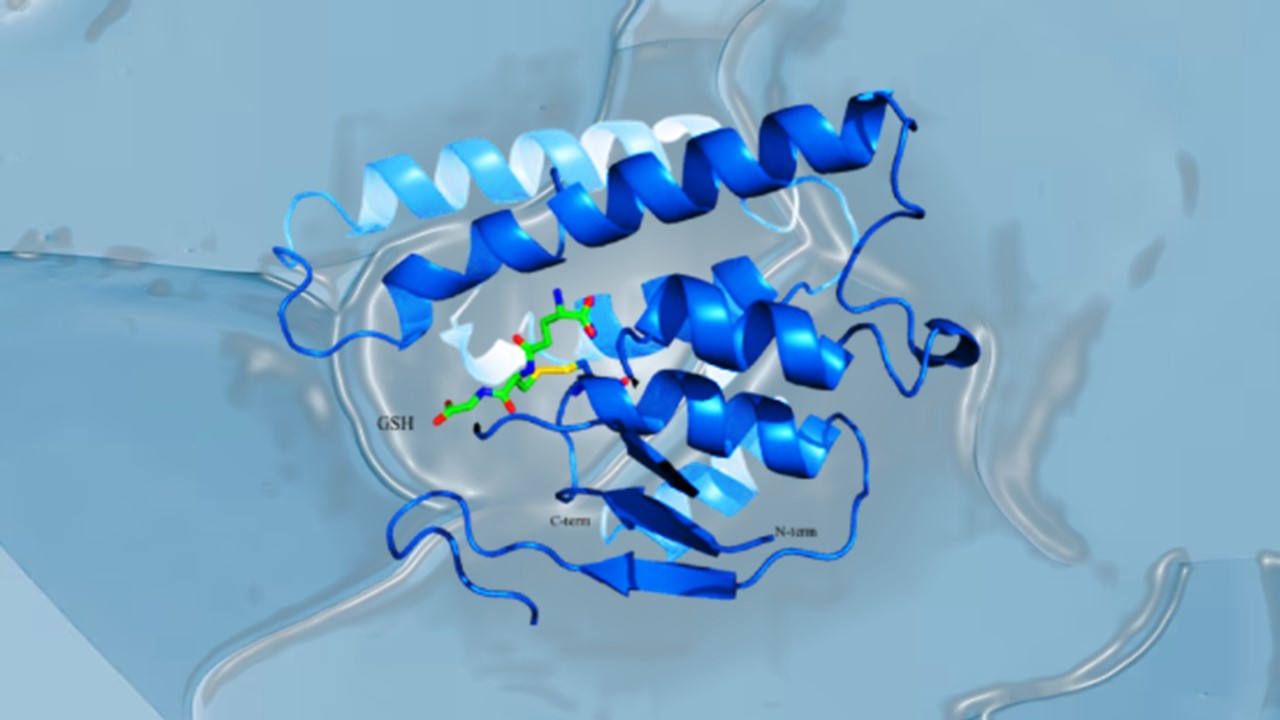
Resistance Mechanisms Unveiled: The Role of Glutathione S-Transferase in Cancer Therapy Failures
Understanding this dual role of GSTs as both protectors and accomplices to malignancies is central to tackling drug resistance.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.
Designing Better Sugar Stoppers: Engineering Selective α-Glucosidase Inhibitors via Fragment-Based Dynamic Chemistry
One of the most pressing challenges in anti-diabetic therapy is reducing the unpleasant and often debilitating gastrointestinal side effects that accompany α-amylase inhibition.