The Lip: An Intersection of Function and Aesthetic
The human lip, a remarkable blend of form and function, stands as both a critical element of communication and a hallmark of personal identity. Structurally, it bridges the external facial skin and the moist oral cavity, facilitating speech articulation, sensory interactions, and expressions that are universally understood. However, this delicate feature is not impervious to abnormalities. Congenital malformations such as orofacial clefts (OFC), traumatic injuries, and age-related changes can disrupt the lips’ functionality and aesthetics. Such conditions frequently lead to psychological stress and, in severe cases, social stigma for affected individuals and their families.
OFCs, encompassing cleft lip with or without cleft palate (CLP), represent the most common congenital anomalies involving the lips. Surgical intervention at an early age—often within the first six months of life—remains the cornerstone of treatment. However, the long-term aesthetic and functional outcomes of such interventions are far from guaranteed, imposing a lifelong burden that extends beyond the physical. To alleviate this multifaceted impact, researchers are turning to advanced cellular models, which promise to unravel the biological intricacies of the lip and its associated conditions.
The Cellular Frontier: Limitations and Innovations
The human lip, despite its centrality in daily life, is a challenging subject for cellular research. Primary cells derived from lip tissue are often seen as the gold standard for studying biological functions due to their retention of native tissue characteristics. Yet, their use is fraught with limitations, primarily their limited capacity for proliferation ex vivo and susceptibility to cellular senescence. This natural growth arrest, whether replicative—linked to telomere shortening—or stress-induced, restricts their utility for extensive experimentation.
To overcome these barriers, researchers have sought methods to immortalize these cells while preserving their inherent properties. By genetically modifying keratinocytes—the predominant cell type in the lip—scientists can create long-lived, stable cell lines that retain the biological traits of their parental tissue. A significant step forward has been the development of keratinocyte lines derived from cleft lip and healthy lip tissue, offering a proof-of-concept for models that could revolutionize the study of lip abnormalities.
Creating Immortalized Keratinocytes: A New Standard in Research
Immortalization involves bypassing cellular senescence, allowing cells to proliferate indefinitely without losing their fundamental characteristics. For lip-derived keratinocytes, this was achieved through the introduction of telomerase reverse transcriptase (hTERT)—an enzyme that elongates telomeres—combined with suppression of the tumor suppressor protein p16INK4A, a key regulator of cellular aging. The resulting immortalized keratinocytes, designated 19K-Ep/T and PA-Ep/T, were derived from healthy lip tissue and cleft lip margins, respectively.
These immortalized lines demonstrated a remarkable capacity for extended proliferation, exceeding 100 population doublings compared to the 30 typical of primary cells. They retained key keratinocyte traits, such as characteristic morphology, specific protein expression patterns, and differentiation potential. Importantly, chromosomal stability tests confirmed the absence of genetic aberrations, assuaging concerns about malignant transformations often associated with immortalization processes. These findings establish a robust foundation for their use in translational and clinical research.
Genetic and Molecular Mechanisms of Lip Development
The development of the upper lip is a complex process orchestrated by the interaction of multiple genetic factors and signaling pathways. Key genes such as IRF6, MSX1, and TFAP2A play pivotal roles in this process. Mutations in IRF6 are associated with Van der Woude syndrome, characterized by cleft lip and palate, underscoring its critical function in lip formation. Similarly, MSX1 is involved in craniofacial development, and mutations in this gene have been linked to orofacial clefts. TFAP2A mutations can lead to branchio-oculo-facial syndrome, which often includes midline cleft lip, highlighting its importance in lip morphogenesis.
Signaling pathways such as Bone Morphogenetic Protein (BMP), Fibroblast Growth Factor (FGF), Sonic Hedgehog (Shh), and Wnt are integral to lip development. These pathways regulate cellular activities like proliferation, differentiation, and apoptosis during embryogenesis. For instance, BMP signaling influences the expression of SHH in the palatal epithelium, which in turn regulates BMP2 in the mesenchyme, essential for mesenchymal proliferation. Disruptions in these pathways can result in malformations such as cleft lip and palate.
The interplay between genetic factors and signaling pathways is crucial for proper lip development. Transcription factors like IRF6 and TFAP2A regulate the expression of genes involved in these signaling pathways, ensuring coordinated development. For example, IRF6 is a downstream target of p63 and activates the expression of Grainyhead-like 3 (GRHL3), which is essential for periderm development and preventing adhesions during lip formation. Understanding these genetic and molecular mechanisms provides insight into the etiology of congenital anomalies such as cleft lip and palate and can inform potential therapeutic interventions.
Mimicking Native Lip Tissue: The Power of 3D Cultures
The complexity of lip biology demands models that replicate the tissue’s three-dimensional (3D) structure. Immortalized keratinocytes were used to create 3D lip cultures that faithfully recapitulated the stratified, keratinized epithelia of native lip tissue. These cultures exhibited similar histological and immunohistochemical characteristics to their primary cell counterparts and the original lip biopsies, including the expression of key markers like E-cadherin, keratin 10, and transglutaminase 1.
These 3D models are transformative for studying lip abnormalities. They provide a controlled environment to explore the molecular underpinnings of conditions like OFC, enabling researchers to investigate tissue-specific responses to genetic, environmental, or microbial challenges. Additionally, these models offer a platform for testing new therapeutic interventions, ranging from regenerative medicine to antimicrobial treatments.
Applications in Wound Healing and Infection Studies
One of the most promising applications of immortalized keratinocytes lies in studying wound healing processes. Lip tissue is highly susceptible to trauma and surgical wounds, particularly in the context of cleft lip repairs. Using scratch assays, researchers demonstrated that these keratinocytes respond to growth factors like epidermal growth factor (EGF) and transforming growth factor-alpha (TGFα) by accelerating wound closure. This aligns with observations in other epithelial tissues, underscoring the clinical relevance of these models.
Infection studies also stand to benefit from these advancements. Lips are frequently exposed to pathogens, with Candida albicans serving as a pertinent example. Immortalized keratinocytes, cultured in 3D systems, were used to model candidal infections, revealing hyphal invasion into the stratified epithelium. This not only highlights the potential for these models to study host-pathogen interactions but also underscores their value in screening antimicrobial agents and exploring immune responses.
Beyond the Lip: Broadening Horizons in Translational Research
The implications of these immortalized keratinocytes extend beyond the study of lip-specific conditions. They hold potential in broader fields such as dermatology, oral pathology, and craniofacial biology. For instance, these cell lines could be pivotal in investigating mucositis—a common complication of cancer therapies affecting the oral mucosa—and actinic cheilitis, a precursor to lip squamous cell carcinoma.
Additionally, genome-editing technologies like CRISPR/Cas9 could be applied to these immortalized cells to dissect the genetic basis of lip-related diseases. The stability and proliferative capacity of these keratinocytes make them ideal candidates for high-throughput genetic studies, which would be impractical with primary cells.
Toward Personalized Therapies for Lip Abnormalities
The development of immortalized keratinocytes marks a significant leap toward personalized medicine in the context of lip abnormalities. By creating cell lines derived from individual patients, researchers can explore patient-specific responses to treatments, paving the way for tailored therapeutic strategies. This approach could be particularly impactful for cleft lip patients, who often face unpredictable outcomes following surgery.
Furthermore, these models support the broader trend toward reducing reliance on animal testing in biomedical research. As human-derived systems, they offer a more accurate representation of human biology, aligning with ethical and scientific imperatives to refine research practices.
The Future of Lip Research
The establishment of immortalized lip keratinocytes heralds a new era in the study of lip biology and pathology. These cell lines provide a versatile and reliable platform for investigating the molecular mechanisms underlying lip development, abnormalities, and repair. As researchers continue to expand their applications, the potential for breakthroughs in personalized medicine, regenerative therapies, and disease prevention becomes ever more tangible.
By bridging the gap between basic science and clinical application, these advancements promise to transform the landscape of craniofacial research and improve outcomes for individuals affected by lip-related conditions. The lips, long celebrated for their role in communication and aesthetics, now stand at the forefront of scientific innovation.
Study DOI: https://dx.doi.org/10.3389/fcell.2024.1449224
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES

Subscribe
to get our
LATEST NEWS
Related Posts

Pathophysiology & Experimental Medicine
Autism Disentangled: FOXG1 Drives Neural Imbalance in the Developing Brain
If FOXG1 overexpression can be modulated, either genetically or pharmacologically, it may be possible to correct the neurodevelopmental imbalances underlying ASD.
Pathophysiology & Experimental Medicine
Adaptive Interactions: How Stimuli-Responsive Materials Revolutionize Cellular Studies
Stimuli-responsive materials revolutionize cellular dynamics research by replicating ECM adaptability, unlocking insights into cell behavior and regulation.
Pathophysiology & Experimental Medicine
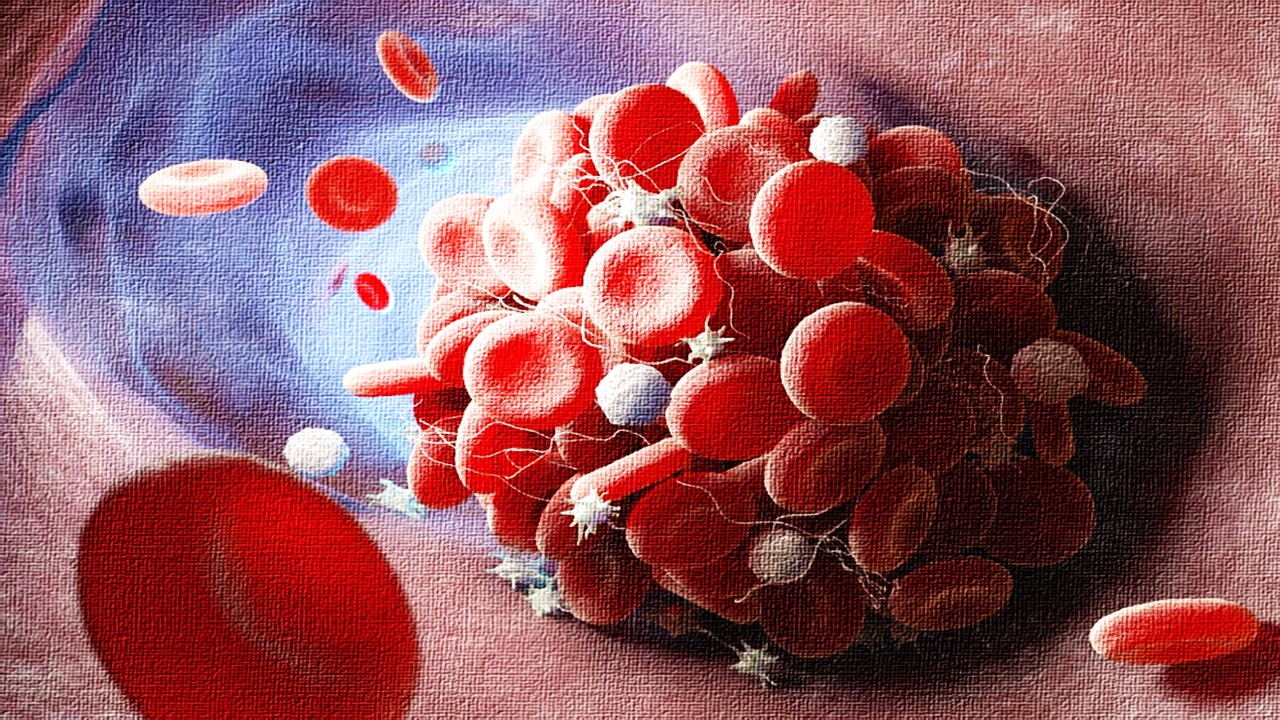
Thrombosis-Free Surfaces: Preventing Blood Clot Formation on Medical Implants Through Selective Protein Interactions
The synthesis and mechanisms of SPI coating are explored, evaluating its potential to overcome the limitations of traditional antifouling surfaces.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.
Designing Better Sugar Stoppers: Engineering Selective α-Glucosidase Inhibitors via Fragment-Based Dynamic Chemistry
One of the most pressing challenges in anti-diabetic therapy is reducing the unpleasant and often debilitating gastrointestinal side effects that accompany α-amylase inhibition.