The development of anti-cancer vaccines is supported by many studies which prove the efficacy of immunotherapy against cancer. Cancer vaccines are also the beginning of preventative treatment for many cancer types, offering hope for susceptible patient populations. The latest advancements show the potential of cancer vaccines as a therapeutic alternative with fewer side effects and greater clinical response.
The introduction of cancer vaccines
Cancer vaccines represent a significant development in onco-immunotherapy. In 2001, the first cancer vaccine was created against the human papilloma virus. This important breakthrough paved the way for the development of the first preventive cervical cancer vaccine – Gardasil.
As with conventional immunotherapy, the goal of cancer vaccines is to amplify the tumour-specific T-cell response. Cancer vaccines are categorised into three platforms: cellular, viral vector, or molecular (e.g. DNA). Dendritic cells are a type of antigen-presenting cell whose role resides in consuming and processing – these cells are used to develop cellular vaccines.
The natural mechanism of viruses allows oncolytic viral vector vaccines to replicate within and destroy tumours. Their ability to directly deliver tumour antigens induces tumour-directed immune responses. Peptide-based DNA cancer vaccines induce tumour-specific responses through the encoding of tumour-associated antigens (TAA) and immunomodulatory molecules. Peptide-based cancer vaccines are popular because of their low toxicity and low manufacturing cost. In addition, they possess direct functional T-cell epitopes (the region of the antigen recognised by the immune system). DNA vaccines are easy to manufacture and present excellent safety profiles.
Effective tumour immunity from cancer vaccines is dependent on a series of specific events:
1. Delivery of the antigen to the antigen-presenting cells
2. Maturation of dendritic cells which create additional environmental signals
3. Migration of dendritic cells, which are appropriately polarised and laden with antigens, to the draining nodes (all material and cells transported out of a certain region have to pass through a certain lymph node packed with B lymphocytes, T lymphocytes and dendritic cells)
4. Antigen presentation to circulating T cells
5. Selection and growth of antigen-reactive T cells (present in nodes)
6. Systematic widespread of T cells directly to tumour deposits
7. Activated tumour-reactive T cells induce apoptosis (programmed cell death)
There are currently four cancer vaccines approved by the FDA for preventive measures including Cervarix (cervical cancer). Unfortunately, there are only two cancer vaccines approved for therapeutic treatment: Bacillus Calmette-Guérin for bladder cancer and Sipuleucel-T (Provenge) for prostate cancer. This emphasises the need to further develop cancer vaccines in order to progress through clinical research to reach FDA approval.
In terms of side effects, cancer vaccines are now being compared with conventional therapies. A 2020 review found that “Cancer vaccines and oncolytic viruses exert profoundly lower side effects in cancer patients than other systemic therapies”. It was found that vaccination with cancer immunotherapy was well tolerated without serious adverse effects. TA peptide-based vaccines, for example, showed to spare healthy tissue, resulting in low toxic effects. In the review, chemotherapy was described to have a negative impact upon the immune system, creating unwanted toxic activity in health tissue. In reference to another study, virus-vector vaccines were also described as better for safety and efficacy in comparison to systemic virus administration.
Challenges and recent developments
Unfortunately, T cell-based immunotherapy for cancer continues to face a number of challenges. Firstly, objective responses to treatment are not consistent across patient populations. Ageing or immune exhaustion after previous treatment, for example, compromise the efficacy of cancer vaccines. The tumour location site is also a factor in the response to immunotherapy interventions like cancer vaccines. Sites such as the bone are typically more challenging to target due to the high concentration of inflammatory cells such as cytokines. In comparison, tumours in the lungs or skin are considered promising anti-cancer targets due to the high occurrence of immune cells. In addition, the tumour microenvironment often presents powerful immunosuppressive mechanisms throughout disease progression which combats immune attacks.
Different types of cancer vaccines also have their own specific disadvantages. After injection of peptide-based vaccines, free peptides rapidly enter circulation in the body, resulting in a lower dose reaching the antigen-presenting cells. The efficacy of DNA vaccines are limited by low transfection rates into tumour cells; mRNA vaccines can deliver higher numbers of antigens but are relatively unstable and inefficient delivery systems.
A 2021 study investigated the efficacy of a neoantigen cancer vaccine (NCV) influenced by microbiota composition of the gut. Microbiotas are communities of microorganisms including bacteria, fungi and viruses. They found that “decreased microbiota diversity induced by prolonged antibiotic (ATB) treatment is associated with higher intratumor specific immune responses and consequently to a better antitumor effect induced by NCV”.
The 2021 study was supported by a 2018 investigation which suggested that gut microbiota composition may compromise the efficacy of immunotherapy. The same study inferred that the highly-personalised gut microbiota in humans may account for the variability in clinical response to immunotherapy treatment. This presents a significant step forward in understanding why some patients’ respond better with immunotherapy like cancer vaccines.
Nanoparticles are a promising adjuvant (substance that enhances efficacy of a certain drug) for cancer vaccines, currently under development. Nanoparticle systems can be surface-modified to selectively target antigen-presenting cells in lymph nodes. In addition, they can act as transporters for antigens. According to a recent study “melanin-based nanoparticles were reported to efficiently localize into draining lymphoid tissues and trigger immune responses against loaded antigens”. Melanin refers to a group of biological molecules responsible for pigmentation of tissue and other structures.
The study stated that due to their photochemical properties, melanin-based nanoparticles can promote anti-cancer mechanisms through photothermal therapy (PTT). PTT works on the basis that molecules like melanin photosynthesise, which means they absorb light and convert it into heat. This type of therapy aims to destroy specific groups of cells without harming the surrounding healthy tissue. The study reinforces melanin as a top candidate as a drug delivery system given its “biocompatibility, biodegradability, high loading efficiency”. Currently, melanin is in development as a transport system for antigenic peptides in vaccines.
Charlotte Di Salvo, Lead Medical Writer
PharmaFeatures
Subscribe
to get our
LATEST NEWS
Related Posts

Immunology & Oncology
The Silent Guardian: How GAS1 Shapes the Landscape of Metastatic Melanoma
GAS1’s discovery represents a beacon of hope in the fight against metastatic disease.
Immunology & Oncology
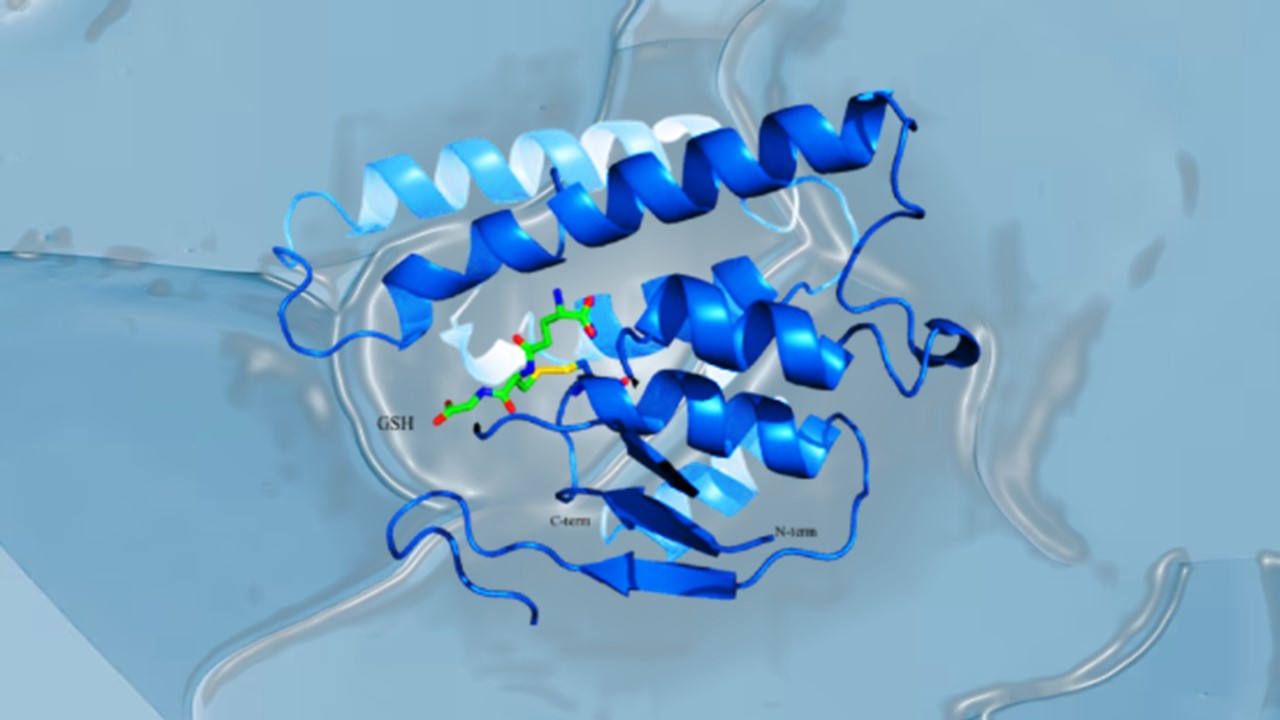
Resistance Mechanisms Unveiled: The Role of Glutathione S-Transferase in Cancer Therapy Failures
Understanding this dual role of GSTs as both protectors and accomplices to malignancies is central to tackling drug resistance.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.
Designing Better Sugar Stoppers: Engineering Selective α-Glucosidase Inhibitors via Fragment-Based Dynamic Chemistry
One of the most pressing challenges in anti-diabetic therapy is reducing the unpleasant and often debilitating gastrointestinal side effects that accompany α-amylase inhibition.