In the ever-evolving landscape of healthcare, multi-omics approaches are at the forefront of innovation. As these approaches continue to advance, they are not limited to the realm of molecular data alone. Instead, they are expanding their horizons into exciting new frontiers, including the integration of electronic health records (EHRs) and clinical imaging data. These integrations hold the promise of enriching the already potent multi-omics datasets and pushing the boundaries of precision health to new heights.
The Promise of Richer Datasets
The fusion of Electronic Health Records (EHRs), multi-omics data, and clinical imaging creates a comprehensive and synergistic approach to understanding an individual’s health. This integration represents a new frontier in healthcare and research, offering profound insights into disease mechanisms, treatment outcomes, and personalized medicine. Let’s delve into the significance of each component:
EHRs: The Clinical Chronicle
Electronic Health Records are digital repositories of a patient’s medical journey, encompassing a wealth of information, such as diagnoses, treatments, medications, lab results, and clinical outcomes. They provide a chronological narrative of an individual’s interactions with the healthcare system, offering context and depth to their medical history.
When integrated with multi-omics data, EHRs become invaluable. Here’s how:
Contextualizing Molecular Findings: Multi-omics data, which includes genomics, transcriptomics, proteomics, and metabolomics, provides intricate molecular insights. However, to fully comprehend the significance of genetic variants or molecular changes, one needs context. EHRs provide this context by linking molecular data to real-world clinical conditions. For example, a genetic variant associated with an increased risk of heart disease gains clinical relevance when correlated with a patient’s history of cardiovascular issues recorded in the EHR.
Treatment Response and Disease Trajectories: EHRs capture a patient’s response to treatments and the evolution of their medical conditions over time. Integrating this information with multi-omics data allows researchers and healthcare providers to understand how molecular profiles correlate with treatment efficacy and disease progression. It can unveil why certain individuals respond differently to the same therapy or how genetic variations influence the course of a disease.
Early Detection and Prevention: By analyzing EHRs in conjunction with multi-omics data, patterns and markers for early disease detection can be identified. This proactive approach can lead to earlier interventions and better outcomes. For instance, the combination of genomic data and EHRs can help predict an individual’s susceptibility to certain cancers, prompting targeted screening or prevention strategies.
Clinical Imaging: Visualizing the Biological Landscape
Clinical imaging techniques like MRI, CT, and PET provide a visual window into the human body’s anatomical, structural, and functional aspects. These images offer a level of detail that is indispensable for understanding diseases and their mechanisms.
When merged with multi-omics data, clinical imaging takes on a new role:
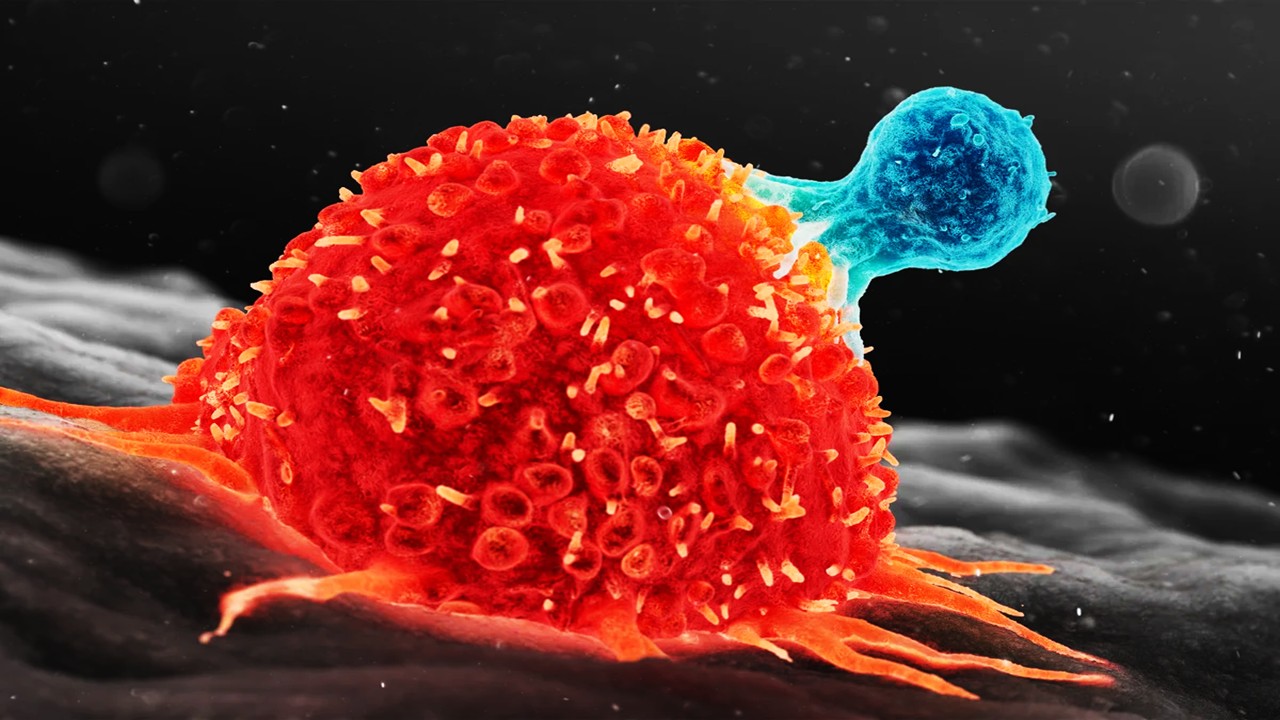
Unraveling Disease Complexity: Diseases are often complex, involving not only molecular alterations but also structural and functional changes. Integrating imaging data with multi-omics allows researchers to unravel this complexity. For instance, in oncology, combining genomics with medical imaging can reveal how genetic mutations influence tumor size, location, and response to treatment.
Personalizing Treatment: Imaging can guide personalized treatment strategies. By visualizing tumor characteristics or organ function, clinicians can tailor therapies to individual patients. For instance, in neurodegenerative diseases, imaging can help identify regions of the brain affected by pathology, aiding in treatment selection and monitoring.
Research Advancements: The synergy of multi-omics and imaging data accelerates research. It enables scientists to investigate how molecular changes manifest in the body and how they correlate with clinical outcomes. This knowledge can lead to the development of novel diagnostics and therapies.
In essence, the integration of EHRs, multi-omics data, and clinical imaging forms a holistic approach to healthcare and research. It transcends the boundaries of traditional medicine, enabling a deeper understanding of diseases at the molecular, clinical, and visual levels. This multidimensional perspective is essential for realizing the promise of precision medicine, where treatments are tailored not just to a patient’s genes but to their entire health profile.
The Challenges Ahead: Data Harmonization and Standardization
The integration of EHRs and clinical imaging data into the realm of multi-omics holds immense promise for advancing precision medicine. However, this merging of diverse data streams is far from straightforward and presents formidable challenges. Two of the most prominent obstacles in this endeavor are data harmonization and standardization.
Data Harmonization: Bridging the Data Divide
Imagine a scenario where EHRs from various healthcare systems need to be combined into a unified framework to be integrated with multi-omics data. Each healthcare system has its own idiosyncrasies in terms of data formats, coding systems, and data standards. This inherent heterogeneity poses a significant hurdle.
Data harmonization is the process by which these disparate data sources are made to harmoniously coexist and interact. It aims to create a common ground where data from different sources can seamlessly converge. This involves developing common data models and ontologies that act as bridges between the varying data structures. These standardized frameworks serve as translators, enabling interoperability and consistent data representation.
For instance, patient diagnoses in one healthcare system might use ICD-10 codes, while another employs SNOMED CT. Data harmonization efforts would involve mapping these different coding systems to a common reference terminology to ensure that the same medical condition is represented consistently across datasets. Such efforts can be a complex and resource-intensive task, but they are essential for making sense of the rich, yet heterogeneous, landscape of clinical data.
Standardization: The Quest for Consistency
Standardization is a critical aspect of integrating clinical imaging data into multi-omics studies. Unlike textual or numerical EHR data, clinical images are often stored in various formats, and different healthcare institutions may use different imaging equipment and protocols. This inherent diversity can introduce variability and inconsistency into the data, making it challenging to draw meaningful conclusions.
To address this issue, standardization efforts focus on several key areas:
Imaging Protocols: Defining standardized imaging protocols is crucial. These protocols outline the specific procedures and settings for acquiring images. For example, in magnetic resonance imaging (MRI), standardization might involve specifying the field strength, sequence parameters, and anatomical planes to be imaged. Adhering to these protocols ensures that images are acquired in a consistent and reproducible manner.
Data Formats: Establishing common data formats for storing clinical images is essential for compatibility. DICOM (Digital Imaging and Communications in Medicine) is a widely adopted standard for medical imaging data. Ensuring that images conform to these formats simplifies data integration and analysis.
Quality Control: Implementing quality control procedures is vital to maintaining data consistency and integrity. This involves regular checks for image artifacts, data completeness, and adherence to imaging protocols. Any deviations can be flagged for review and correction.
By addressing these standardization aspects, the goal is to create a level playing field where clinical imaging data from different sources can be reliably integrated into multi-omics studies. Standardization not only enhances data compatibility but also facilitates cross-institutional collaborations and ensures the credibility of research findings.
Clinical Implementation: Bridging Research and Practice
Perhaps the most complex challenge is the clinical implementation of multi-omics approaches. While research settings have seen significant advancements in multi-omics technologies and methodologies, translating these findings into routine clinical practice is a multifaceted endeavor. Several key aspects need to be addressed, including:
Clinical Utility: Demonstrating the clinical utility of multi-omics data in improving patient outcomes and healthcare decision-making is paramount. It requires rigorous validation of multi-omics biomarkers, the development of clinical guidelines, and evidence-based practices.
Ethical and Privacy Considerations: Safeguarding patient privacy and ensuring ethical data use are essential when handling sensitive multi-omics and clinical data. Robust data governance frameworks and informed consent processes must be established.
Healthcare Provider Training: Healthcare professionals need to be educated and trained in interpreting multi-omics data and incorporating it into clinical decision-making. This includes understanding the strengths, limitations, and potential biases of these data.
Infrastructure and Integration: Developing the necessary infrastructure, including data storage, analysis pipelines, and reporting tools, is essential for seamless integration into clinical workflows.
Pioneering the Future of Healthcare
As multi-omics continues to advance and expand its horizons by integrating electronic health records and clinical imaging data, it opens up exciting possibilities for precision health. The synergy of molecular, clinical, and imaging data promises to provide a comprehensive view of an individual’s health, enabling personalized and effective healthcare interventions.
However, the journey ahead is not without its complexities. Data harmonization, standardization, and clinical implementation are formidable challenges that require collaborative efforts from researchers, healthcare institutions, policymakers, and technology providers. Overcoming these challenges will pave the way for a future where precision health is not just a concept but a reality—a future where healthcare is truly tailored to the unique characteristics and needs of each individual, ultimately leading to improved patient outcomes and a healthier society.
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Subscribe
to get our
LATEST NEWS
Related Posts

Bioinformatics & Multiomics
Agentic Bioinformatics: How Autonomous AI Agents Compress Biomedical Discovery Cycles
Agentic bioinformatics treats biomedical discovery as a closed-loop system where specialized AI agents continuously translate intent into computation, computation into evidence, and evidence into the next experiment.

Bioinformatics & Multiomics
Proteomic Signatures: Molecular Discrimination of Hyperinflammatory States Through Serum Proteome Architecture
Serum proteomics exposes how sepsis and hemophagocytic syndromes diverge at the level of immune regulation and proteostasis, enabling precise molecular discrimination.

Bioinformatics & Multiomics
Residual Signals: Transcriptomic Surveillance and Multi-Domain Gene-Signature Mapping for Early Breast Cancer MRD Detection
MRD detection in breast cancer focuses on uncovering functional transcriptomic and microenvironmental signals that reveal persistent tumor activity invisible to traditional genomic approaches.
Read More Articles
Spatial Collapse: Pharmacologic Degradation of PDEδ to Disrupt Oncogenic KRAS Membrane Localization
PDEδ degradation disrupts KRAS membrane localization to collapse oncogenic signaling through spatial pharmacology rather than direct enzymatic inhibition.
Neumedics’ Integrated Innovation Model: Dr. Mark Nelson on Translating Drug Discovery into API Synthesis
Dr. Mark Nelson of Neumedics outlines how integrating medicinal chemistry with scalable API synthesis from the earliest design stages defines the next evolution of pharmaceutical development.
Zentalis Pharmaceuticals’ Clinical Strategy Architecture: Dr. Stalder on Data Foresight and Oncology Execution
Dr. Joseph Stalder of Zentalis Pharmaceuticals examines how predictive data integration and disciplined program governance are redefining the future of late-stage oncology development.
Exelixis Clinical Bioanalysis Leadership, Translational DMPK Craft, and the Kirkovsky Playbook
Senior Director Dr. Leo Kirkovsky brings a rare cross-modality perspective—spanning physical organic chemistry, clinical assay leadership, and ADC bioanalysis—to show how ADME mastery becomes the decision engine that turns complex drug systems into scalable oncology development programs.
Policy Ignition: How Institutional Experiments Become Durable Global Evidence for Pharmaceutical Access
Global pharmaceutical access improves when IP, payment, and real-world evidence systems are engineered as interoperable feedback loops rather than isolated reforms.