The Unmet Need in Colorectal Cancer Treatment
Colorectal cancer (CRC) remains a formidable global health challenge. As the third most prevalent malignancy and the second leading cause of cancer-related deaths, its societal and clinical burden is immense. Current therapeutic options, ranging from surgery and chemotherapy to targeted molecular therapies, have shown limited success in metastatic settings due to chemoresistance and tumor recurrence. Despite advances, survival rates plateau, underscoring the urgent need for innovative therapeutic approaches.
Enter TG1, a novel derivative of the natural compound THSG (2,3,5,4′-Tetrahydroxystilbene-2-O-β-D-Glucoside). Derived from Polygonum multiflorum, a cornerstone of traditional Chinese medicine, TG1 represents a promising frontier in CRC therapy. Unlike its parent compound, TG1 undergoes structural modification, enhancing its potency while retaining minimal toxicity. This article explores the multifaceted mechanisms through which TG1 targets CRC, including the induction of ferroptosis, apoptosis, and autophagy, providing new hope for overcoming therapeutic stagnation in CRC management.
Ferroptosis: The Linchpin of TG1’s Cytotoxic Effects
Ferroptosis, a novel form of programmed cell death distinct from apoptosis and necrosis, is emerging as a therapeutic focus in oncology. Characterized by iron-dependent lipid peroxidation and reactive oxygen species (ROS) accumulation, ferroptosis selectively targets cancer cells resistant to traditional therapies. TG1 stands out by leveraging this mechanism with unparalleled precision.
RNA sequencing revealed that TG1 treatment significantly alters ferroptosis-related gene expression in CRC cells. Genes such as GPX4, a ferroptosis suppressor, and HSPB1, a resistance-associated protein, are markedly downregulated. Concurrently, TG1 upregulates ferroptosis drivers like ACSL4, a lipid metabolism regulator critical for peroxidation pathways. These shifts disrupt cellular homeostasis, leading to the accumulation of lipid peroxides and culminating in ferroptotic cell death.
The ferroptosis inhibitor Bardoxolone confirmed TG1’s reliance on this pathway. Inhibition of ferroptosis rescued CRC cells from TG1-induced cytotoxicity, highlighting the pathway’s centrality to the compound’s anticancer effects. This precision targeting positions TG1 as a novel therapeutic agent in CRC, especially in cases resistant to conventional treatments.
Apoptosis: Amplifying Cellular Self-Destruction
TG1’s anticancer arsenal extends beyond ferroptosis to include apoptosis, a well-established mechanism of programmed cell death. Apoptosis plays a dual role in cancer, eliminating malignant cells while circumventing the inflammatory aftermath of necrosis. TG1’s ability to modulate apoptotic pathways underscores its versatility.
Flow cytometry and Western blot analyses demonstrate that TG1 significantly enhances apoptotic markers in CRC cells. Pro-apoptotic proteins such as Bax, cleaved caspase-3, and c-PARP are upregulated, while anti-apoptotic proteins like Bcl-2 and phosphorylated Akt are suppressed. These molecular shifts dismantle the cell’s survival machinery, driving it toward self-destruction.
What sets TG1 apart is its synergistic modulation of apoptosis and ferroptosis. Cancer cells often adapt to evade single-cell death pathways; by concurrently targeting multiple mechanisms, TG1 amplifies its cytotoxic potential, reducing the likelihood of resistance. This dual approach marks a paradigm shift in CRC therapy.
Autophagy: Navigating the Balance Between Survival and Death
Autophagy, the cellular process of self-digestion and recycling, plays a paradoxical role in cancer. While often protective under stress, excessive autophagy can induce autophagic cell death. TG1 exploits this duality to tip the balance against CRC cells.
Using autophagy detection assays, researchers observed increased autophagic vacuole formation in TG1-treated cells. Western blotting confirmed the upregulation of autophagy-related proteins, including Beclin-1 and LC3B-II, alongside the degradation of p62, a hallmark of autophagic flux. These findings suggest that TG1 induces autophagy as a complementary mechanism to ferroptosis and apoptosis.
Interestingly, autophagy may act as a bridge linking ferroptosis and apoptosis. Studies have shown that autophagy facilitates ferritin degradation, increasing free iron availability and amplifying ferroptotic signaling. TG1’s ability to orchestrate this interplay highlights its sophisticated therapeutic potential.
Targeting MYC: Disrupting the Oncogenic Nexus
The MYC proto-oncogene is a critical driver of CRC progression, implicated in cell proliferation, metabolic reprogramming, and chemoresistance. Aberrant MYC activation is a hallmark of aggressive CRC phenotypes, making it a prime therapeutic target. TG1 emerges as a potent MYC modulator, offering a strategic advantage in combating CRC.
Gene expression analyses reveal that TG1 downregulates MYC and its downstream targets, disrupting metabolic pathways essential for CRC survival. Pathway enrichment analyses identified significant reductions in MYC-regulated processes, including cholesterol homeostasis and glycolysis. By dismantling these pathways, TG1 starves cancer cells of essential resources, compounding its cytotoxic effects.
This anti-MYC activity positions TG1 as a promising candidate for addressing chemoresistance, a major obstacle in CRC therapy. By undermining the molecular infrastructure of MYC-driven tumors, TG1 offers a targeted approach to improving therapeutic outcomes.
In Vivo Efficacy: Translating Promise to Practice
The therapeutic potential of TG1 is not confined to in vitro studies. In vivo experiments using a xenograft mouse model demonstrate TG1’s robust anticancer effects. Administered intravenously, TG1 significantly suppresses tumor growth, outperforming irinotecan, a standard CRC chemotherapeutic agent. This efficacy, coupled with its low toxicity, underscores TG1’s translational potential.
Tumor volume reduction in TG1-treated mice correlates with molecular findings, affirming its mechanisms of action. The compound’s ability to induce ferroptosis, apoptosis, and autophagy in a live model validates its clinical relevance. These results mark a significant step toward TG1’s eventual application in human CRC therapy.
A New Frontier in Colorectal Cancer Treatment
TG1 represents a groundbreaking advancement in CRC therapy. By targeting ferroptosis, apoptosis, and autophagy while modulating MYC, TG1 disrupts the intricate survival networks of CRC cells. Its dual in vitro and in vivo efficacy positions it as a compelling candidate for further clinical development.
In a landscape dominated by resistance and recurrence, TG1 offers a multi-mechanistic approach to overcoming the limitations of current therapies. As research progresses, TG1 could redefine CRC treatment paradigms, bringing renewed hope to patients worldwide.
Study DOI: https://doi.org/10.3390/biomedicines11071798
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Subscribe
to get our
LATEST NEWS
Related Posts

Medicinal Chemistry & Pharmacology
Aerogel Pharmaceutics Reimagined: How Chitosan-Based Aerogels and Hybrid Computational Models Are Reshaping Nasal Drug Delivery Systems
Simulating with precision and formulating with insight, the future of pharmacology becomes not just predictive but programmable, one cell at a time.

Medicinal Chemistry & Pharmacology
Coprocessed for Compression: Reengineering Metformin Hydrochloride with Hydroxypropyl Cellulose via Coprecipitation for Direct Compression Enhancement
In manufacturing, minimizing granulation lines, drying tunnels, and multiple milling stages reduces equipment costs, process footprint, and energy consumption.

Medicinal Chemistry & Pharmacology
Decoding Molecular Libraries: Error-Resilient Sequencing Analysis and Multidimensional Pattern Recognition
tagFinder exemplifies the convergence of computational innovation and chemical biology, offering a robust framework to navigate the complexities of DNA-encoded science
Read More Articles
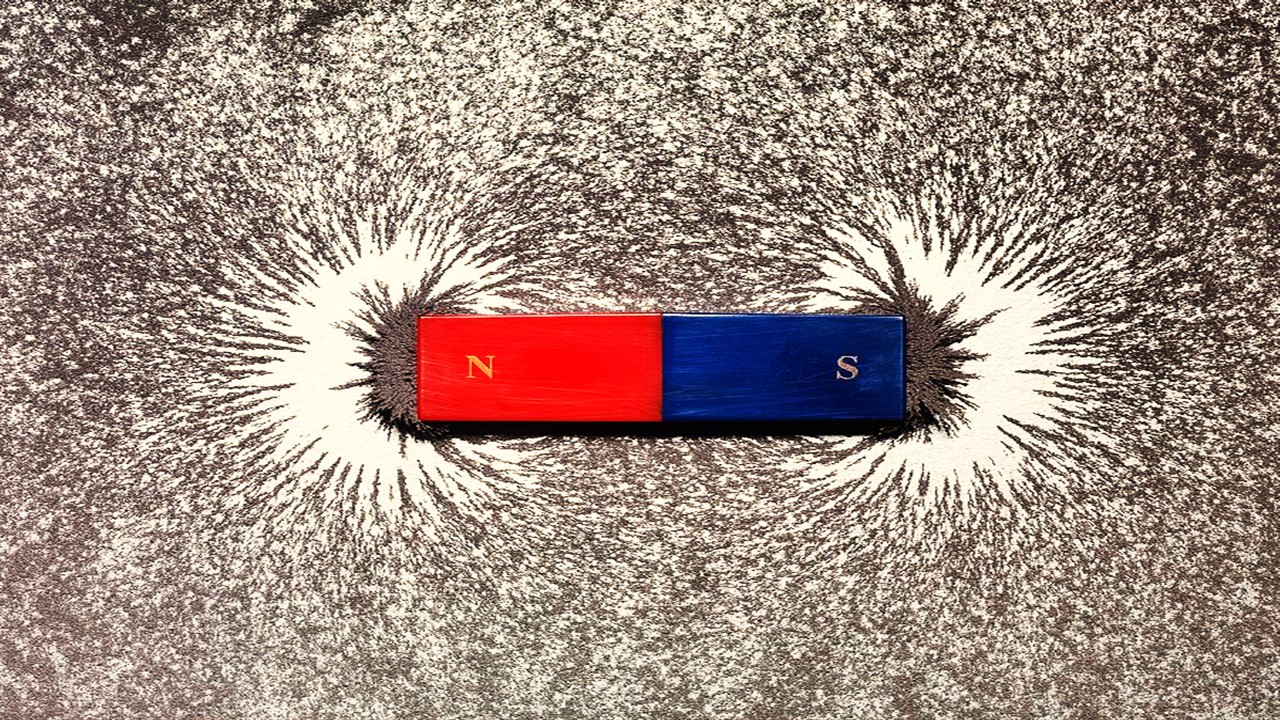
Magnetic Nanoengineering: Overcoming Biological Variability and Enhancing Therapeutic Precision
The future of nanomedicine lies in harmonizing precision, accessibility, and ecological responsibility, ushering in an era where therapies are tailored to individual biological landscapes.