Traditional drug discovery has long relied on a cascade of chemical optimization and biological screening to identify lead compounds that are both efficacious and safe for human use. However, with the advent of nanotechnology, the paradigm has shifted significantly. Nanoparticles (NPs), as drug delivery systems, offer a novel mechanism for enhancing the pharmacokinetic and pharmacodynamic properties of drugs, allowing for more targeted and efficient delivery. Yet, this evolution from conventional drug discovery to modern lead discovery presents both new opportunities and challenges.
Nanoparticle drug delivery systems represent an intersection of material science, molecular biology, and clinical pharmacology. These systems are designed to improve the biodistribution of active pharmaceutical ingredients (APIs), reduce off-target effects, and optimize therapeutic outcomes. While the premise of utilizing nanoscale materials to enhance drug performance is promising, the path from preclinical models to clinical application requires a deep understanding of nanoparticle interactions with biological systems, particularly their absorption, distribution, metabolism, and excretion (ADME) profiles.
Nanoparticles and Preclinical Models: A Complex Interplay
In vivo evaluation of nanoparticle-based therapeutics demands a sophisticated approach, one that takes into account not only the disease model but also the intricacies of the nanoparticle’s physicochemical properties. The surface chemistry and functionalization of NPs, often involving the addition of polyethylene glycol (PEG) or other ligands, significantly affect their ADME properties. A nanoparticle’s ability to evade phagocytic clearance, penetrate target tissues, and maintain therapeutic concentrations in the bloodstream hinges on these modifications.
Animal models play an indispensable role in assessing the safety and efficacy of nanoparticle formulations, yet their predictive value remains imperfect. While small vertebrate models, such as zebrafish, offer high throughput, lower costs, and some clinical relevance due to their conserved immune systems, they are limited by significant physiological differences when compared to humans. Rodents, particularly mice, are the gold standard in nanoparticle preclinical studies, but the physiological and immunological differences between murine models and humans can result in misleading data. Therefore, selecting the appropriate animal model for preclinical nanoparticle assessment must involve a nuanced consideration of the disease state, nanoparticle surface modifications, and desired route of administration (ROA).
Zebrafish: The Initial Vanguard in Nanoparticle Screening
The zebrafish has emerged as a favored model for early-stage nanoparticle toxicity and clearance studies due to its transparent body, which facilitates advanced imaging techniques such as fluorescence and confocal microscopy. These capabilities allow researchers to visualize real-time interactions between nanoparticles and biological systems. Moreover, the zebrafish shares key immune system mechanisms with mammals, including both innate and adaptive immunity, making it a valuable model for studying nanoparticle clearance pathways.
Recent studies have demonstrated that PEGylated nanoparticles exhibit reduced opsonization and macrophage uptake in zebrafish models, a phenomenon previously observed in mammals. The use of transgenic zebrafish expressing green fluorescent proteins in their vasculature and macrophages has enabled the visualization of nanoparticle distribution and clearance dynamics. Interestingly, these studies have shown a strong correlation between the clearance kinetics of nanoparticles in zebrafish and their clearance in mammalian models, particularly in the spleen and liver.
Despite these advantages, the zebrafish model is not without limitations. While it provides valuable insights into nanoparticle clearance and toxicity, it does not fully replicate the complexities of human disease pathophysiology. Thus, while zebrafish offer a valuable first step in nanoparticle screening, further validation in higher-order animal models is required.
Rodent Models: A Closer Approximation to Human Physiology
Rodents, especially mice, remain the cornerstone of preclinical nanoparticle research. Their relatively close anatomical and physiological similarities to humans, combined with the availability of genetically modified strains, make them indispensable for assessing nanoparticle efficacy and safety. However, not all rodent models are created equal, particularly when studying nanoparticle clearance and immune responses.
Athymic nude mice and NOD Skid Gamma (NSG) mice, commonly used in cancer research, are immunocompromised, which allows for the rapid growth of human-derived tumors. While this feature makes them attractive for nanoparticle-based cancer therapy studies, their compromised immune systems pose significant challenges when interpreting clearance data. The absence of mature T cells and reduced levels of opsonizing antibodies, such as IgG and IgA, can lead to aberrant nanoparticle clearance profiles, thus limiting the translatability of results to human clinical settings.
More recently, studies have highlighted the importance of using immune-competent rodent models for nanoparticle evaluation. Murine strains with intact immune systems, such as BALB/c or C57BL/6 mice, provide a more reliable model for studying nanoparticle interactions with the immune system. These models offer insights into how different immune system biases, such as Th1 or Th2 responses, affect nanoparticle clearance. For instance, Th2-biased strains have been shown to clear nanoparticles more rapidly than Th1-biased strains, an observation that may have significant implications for nanoparticle-based immunotherapies.
Route of Administration: Shaping Nanoparticle Efficacy
The route of administration (ROA) is a critical determinant of nanoparticle efficacy and must be carefully considered in preclinical studies. Intravenous (IV) injection and oral administration are the most commonly employed routes in nanoparticle drug delivery. However, nanoparticles face numerous challenges in the bloodstream, including rapid clearance by the mononuclear phagocyte system (MPS) and opsonization by serum proteins.
Surface modifications, such as PEGylation, can extend circulation times by shielding nanoparticles from immune recognition, but these modifications must be tailored to the specific ROA and target tissue. For example, PEGylation has been shown to reduce macrophage uptake in both zebrafish and rodent models, but its effectiveness may vary depending on the disease state and immune environment. Additionally, other ROAs, such as pulmonary or intra-articular delivery, present unique challenges that require specialized animal models. Pulmonary delivery, for instance, is complicated by the presence of lung-associated macrophages (LAMs) that rapidly clear inhaled nanoparticles, while intra-articular delivery is hindered by the small size of rodent joints.
Pulmonary and Intra-Articular Routes: Special Considerations
Nanoparticle delivery through inhalation is becoming increasingly relevant, particularly for diseases affecting the respiratory system or for systemic delivery via the pulmonary route. The inhalation of nanoparticles introduces them to the upper and lower airways, where they are subjected to mucociliary clearance and macrophage uptake. Studies in rodent models, particularly rats, have demonstrated that nanoparticles administered via inhalation are cleared by mechanisms that closely resemble human pulmonary clearance, providing a promising avenue for further research. However, the complexities of the pulmonary immune response and the long-term retention of nanoparticles in lung tissues require more in-depth study before clinical translation can be realized.
Intra-articular (IA) delivery of nanoparticles represents another exciting frontier in drug delivery, particularly for the treatment of joint diseases such as osteoarthritis. Rodent models, particularly rats, have been instrumental in assessing the efficacy of IA nanoparticle delivery systems, such as PLGA microspheres, which have shown promise in delivering sustained drug release directly to affected joints. However, the anatomical and biomechanical differences between rodent and human joints present a significant challenge in translating these findings to the clinic. Larger animal models, with joint structures more similar to those of humans, are necessary to fully understand the potential of IA nanoparticle delivery.
The Road Ahead: Challenges and Opportunities
Nanoparticle-based drug delivery systems have the potential to revolutionize the treatment of a wide range of diseases, from cancer to chronic inflammatory conditions. However, the path to clinical translation is fraught with challenges. The complexity of nanoparticle interactions with the immune system, coupled with the limitations of preclinical animal models, underscores the need for a more nuanced approach to nanoparticle development.
Despite the promise of nanoparticles, their rapid clearance by the mononuclear phagocyte system remains a significant hurdle. While surface modifications such as PEGylation have shown some success in extending circulation times, more sophisticated strategies are needed to fully exploit the potential of nanoparticles as drug delivery vehicles. Furthermore, the choice of preclinical animal model must be carefully tailored to the disease state, nanoparticle characteristics, and desired route of administration.
In the coming years, advances in nanotechnology, immunology, and pharmacology will undoubtedly pave the way for more effective nanoparticle-based therapies. By integrating these disciplines and refining preclinical models, researchers can unlock the full potential of nanomedicine, ushering in a new era of precision medicine.
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts

Medicinal Chemistry & Pharmacology
Aerogel Pharmaceutics Reimagined: How Chitosan-Based Aerogels and Hybrid Computational Models Are Reshaping Nasal Drug Delivery Systems
Simulating with precision and formulating with insight, the future of pharmacology becomes not just predictive but programmable, one cell at a time.

Medicinal Chemistry & Pharmacology
Coprocessed for Compression: Reengineering Metformin Hydrochloride with Hydroxypropyl Cellulose via Coprecipitation for Direct Compression Enhancement
In manufacturing, minimizing granulation lines, drying tunnels, and multiple milling stages reduces equipment costs, process footprint, and energy consumption.

Medicinal Chemistry & Pharmacology
Decoding Molecular Libraries: Error-Resilient Sequencing Analysis and Multidimensional Pattern Recognition
tagFinder exemplifies the convergence of computational innovation and chemical biology, offering a robust framework to navigate the complexities of DNA-encoded science
Read More Articles
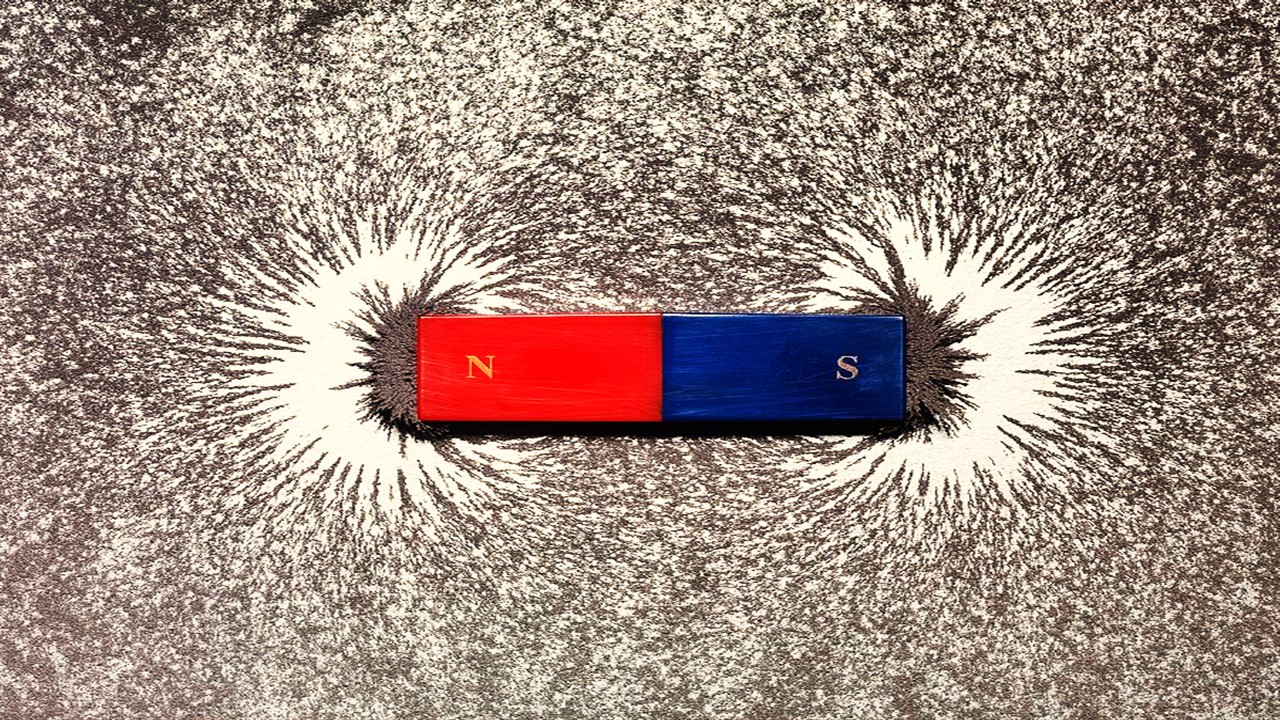
Magnetic Nanoengineering: Overcoming Biological Variability and Enhancing Therapeutic Precision
The future of nanomedicine lies in harmonizing precision, accessibility, and ecological responsibility, ushering in an era where therapies are tailored to individual biological landscapes.
Trials, Triumphs, and Trials Ahead: Navigating the Landscape of Randomized Controlled Trials in Artificial Intelligence-Driven Healthcare
The adoption of artificial intelligence in clinical practice has prompted a surge in randomized controlled trials, highlighting a balance of enthusiasm and prudence.
Illuminating the Dark Genome: Uncharted Frontiers in Therapeutic Discovery
The dark genome is not a biological void but a frontier awaiting illumination.