Infliximab, a monoclonal antibody targeting tumor necrosis factor-alpha (TNF-α), has transformed the treatment of autoimmune diseases since its introduction in 1998. This drug, a chimeric mouse-human antibody, neutralizes TNF-α, a key pro-inflammatory cytokine responsible for driving inflammatory conditions such as rheumatoid arthritis (RA) and inflammatory bowel diseases (IBD), including Crohn’s disease and ulcerative colitis. The importance of TNF-α as a therapeutic target has cemented infliximab as a cornerstone in the management of these debilitating diseases, leading to remarkable advances in patient outcomes.
Beyond its role in suppressing TNF-α, infliximab also modulates other inflammatory mediators, such as vascular endothelial growth factors and chemokines, particularly within synovial tissues. This reduction in chemokine expression limits the migration of lymphocytes to inflamed areas like the joints in RA patients, thereby alleviating symptoms and disease progression. As more is learned about infliximab’s mechanisms of action, its role in modern therapeutics is continually being refined, offering deeper insights into the genetic underpinnings of patient responses.
Polymorphisms and Genetic Predictors of Response
Infliximab’s success has sparked an interest in understanding genetic markers that influence patient response. Numerous studies have focused on genetic polymorphisms in RA patients to determine why some individuals experience a more profound clinical response than others. A prime example is the study of polymorphisms in FCGR2A and FCGR3A, two genes involved in immune complex clearance, which may impact how efficiently infliximab is eliminated from the body.
The FCGR2A-RR genotype has emerged as a potential predictor of positive response, with patients exhibiting this low-affinity variant demonstrating a more favorable ACR20 response compared to those with the HH or RH genotypes. Similarly, the FCGR3A low-affinity variant (FF) shows a significantly better ACR50 response after just six weeks of infliximab treatment, providing further evidence that genetic makeup can influence therapeutic outcomes.
These findings suggest that infliximab’s effectiveness in RA may be closely tied to these specific genetic traits, allowing for more personalized approaches to treatment in the future. By identifying patients who are more likely to respond based on their genetic profile, clinicians may eventually tailor therapies to optimize outcomes, a concept at the heart of precision medicine.
Current Diagnosis: From Symptom Presentation to Molecular Targeting
The diagnosis of RA and IBD has evolved significantly from traditional clinical evaluations to more refined molecular and imaging techniques. In RA, diagnostic criteria now emphasize early detection, incorporating biomarkers such as anti-cyclic citrullinated peptide (anti-CCP) antibodies and rheumatoid factor (RF). These biomarkers are not only predictive of disease severity but also help guide therapeutic decision-making, particularly in choosing biologic therapies like infliximab.
Imaging techniques, including ultrasound and magnetic resonance imaging (MRI), have become critical tools in diagnosing and monitoring disease activity. These methods enable physicians to assess the extent of joint damage and inflammation, which can be difficult to gauge through clinical examination alone. For IBD, colonoscopy remains the gold standard for diagnosing Crohn’s disease and ulcerative colitis, though advancements in imaging modalities like capsule endoscopy and magnetic resonance enterography (MRE) are providing less invasive options for assessing intestinal inflammation.
The integration of molecular diagnostics, such as genetic profiling and biomarkers, is increasingly shaping the approach to diagnosing autoimmune diseases. These advances allow for earlier intervention, reducing the long-term complications of these chronic conditions.
Current Best Practices in Management: A Shift Towards Biologics
The management of RA and IBD has shifted considerably with the advent of biologic therapies like infliximab. Traditionally, treatment centered on disease-modifying antirheumatic drugs (DMARDs) such as methotrexate and corticosteroids. While these therapies remain foundational, biologics offer more targeted approaches, directly interfering with the cytokine cascades that drive inflammation.
Infliximab’s role in the induction and maintenance of remission in both RA and IBD is now well established. In RA, combination therapy with methotrexate enhances the efficacy of infliximab, reducing antibody formation against the drug and improving patient outcomes. For IBD, infliximab is particularly effective in patients with fistulizing Crohn’s disease and moderate to severe ulcerative colitis, providing long-term remission and mucosal healing in many cases.
However, treatment is not without challenges. Primary and secondary non-response, where patients either fail to respond initially or lose responsiveness over time, remains a significant issue. Factors such as the development of anti-drug antibodies (ADAs), suboptimal dosing, and underlying genetic polymorphisms contribute to this phenomenon. To mitigate this, therapeutic drug monitoring and individualized dosing strategies are becoming more common, helping clinicians adjust therapy based on infliximab serum levels and ADA presence.
Genetic Insights: Exploring the Role of TNF Polymorphisms
The relationship between TNF gene polymorphisms and infliximab response has been the subject of extensive research, given TNF’s central role in inflammation. Variations in the TNF-α promoter, such as the −308G/A polymorphism, have been linked to differences in patient outcomes, although findings remain inconclusive.
For example, RA patients with the G/G genotype often experience greater improvements in disease activity scores after infliximab treatment compared to those with the A/A or A/G genotypes. This is thought to be due to differences in TNF-α bioactivity levels, as patients with the G/G variant tend to have lower circulating TNF-α levels, leading to better disease control.
In contrast, other polymorphisms, such as the TNF-238 and +489 genotypes, have been associated with severe RA and poorer outcomes. Understanding these genetic variations not only deepens our knowledge of TNF’s role in disease pathogenesis but also paves the way for more effective, personalized treatment regimens.
Pharmacological Approaches: Beyond Infliximab
While infliximab remains a pivotal drug in the management of autoimmune diseases, other biologics have joined the therapeutic arsenal. Rituximab, another monoclonal antibody, targets CD20 on B-cells and is used primarily in RA patients who do not respond to TNF inhibitors like infliximab. Rituximab’s ability to deplete B-cells helps reduce the production of autoantibodies, leading to decreased inflammation and symptom improvement.
The combination of infliximab and rituximab with other DMARDs continues to show promise in achieving remission in patients with severe or refractory RA. Meanwhile, newer biologics targeting different pathways, such as interleukin-6 (IL-6) inhibitors and Janus kinase (JAK) inhibitors, are expanding treatment options, offering hope to patients who do not respond to traditional therapies.
The future of autoimmune disease management lies in expanding our understanding of the molecular and genetic drivers of disease. As personalized medicine continues to evolve, the role of pharmacogenomics will likely become more prominent, ensuring that therapies like infliximab are administered to the patients most likely to benefit.
Conclusion: Precision and Innovation in Drug Discovery
The journey from traditional drug discovery to modern biologics like infliximab marks a monumental shift in the treatment of autoimmune diseases. As our understanding of genetics and molecular biology deepens, the possibility of tailored therapies that offer more consistent and effective outcomes comes closer to reality. By identifying genetic predictors of response, refining diagnostic methods, and employing advanced pharmacological strategies, clinicians are increasingly able to provide personalized care to patients with chronic inflammatory diseases.
Infliximab’s success is just the beginning of this precision medicine revolution. As we continue to uncover the genetic and molecular bases of disease, the future of drug discovery promises even greater strides in the treatment of complex conditions like RA and IBD.
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts

Chronic & Debilitating Diseases
Renopathology Tipping Point: Deciphering the Molecular Code of Stage 2 Chronic Kidney Disease
The molecular events of Stage 2 CKD, from inflammation to lipid metabolism, offer insights for diagnosis and treatment.
Chronic & Debilitating Diseases
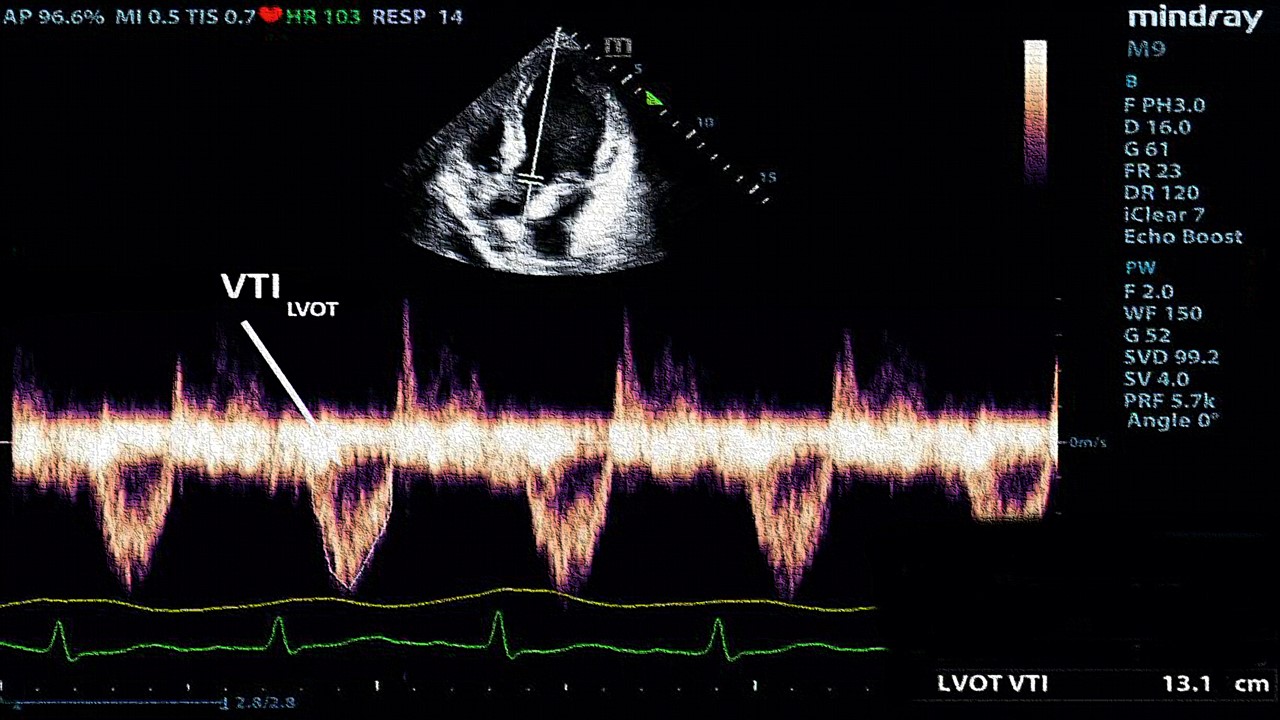
A New Lens on Shock: Hemodynamic Insights Through Critical Care Ultrasound
CCU has transformed the hemodynamic assessment of shock, delivering a reliable, reproducible, and non-invasive tool for ICU clinicians.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.













