Despite aggressive approaches to treatment and decades of research, prognosis remains poor for patients with glioblastomas, with the overall survival period reported to be less than 15 months after diagnosis. Nanoparticle drug delivery is one of the many methods researchers hope will address the challenge of delivering chemotherapeutic agents across the blood-brain barrier (BBB).
Introduction
Gliomas refers to tumour formation originating from glial cells of the central nervous system (CNS). Glial cells are non-neuronal cells present in the CNS and peripheral nervous system (PNS) which act to support and protect neurons.
Glioblastoma (GBM) is a grade IV glioma subtype and accounts for almost half of all primary malignant brain tumours. According to National Brain Tumor Society, the five-year survival rate for glioblastoma patients is only 6.8%, and the average length of survival for glioblastoma patients is estimated to be only 12 to 18 months.
The key takeaway is that the survival rates and mortality statistics for these aggressive brain tumours, which accounts for a huge proportion of brain tumour cases, have remained virtually unchanged for decades. This represents a significant unmet clinical need for effective treatment options and focus on drug development.
Current treatment
As of the last five years, the regimen for patients with GBMs is not curative, meaning it does not kill every tumour cell. This has seen huge efforts across cancer research and the pharmaceutical industry to work hard to discover new treatment strategies.
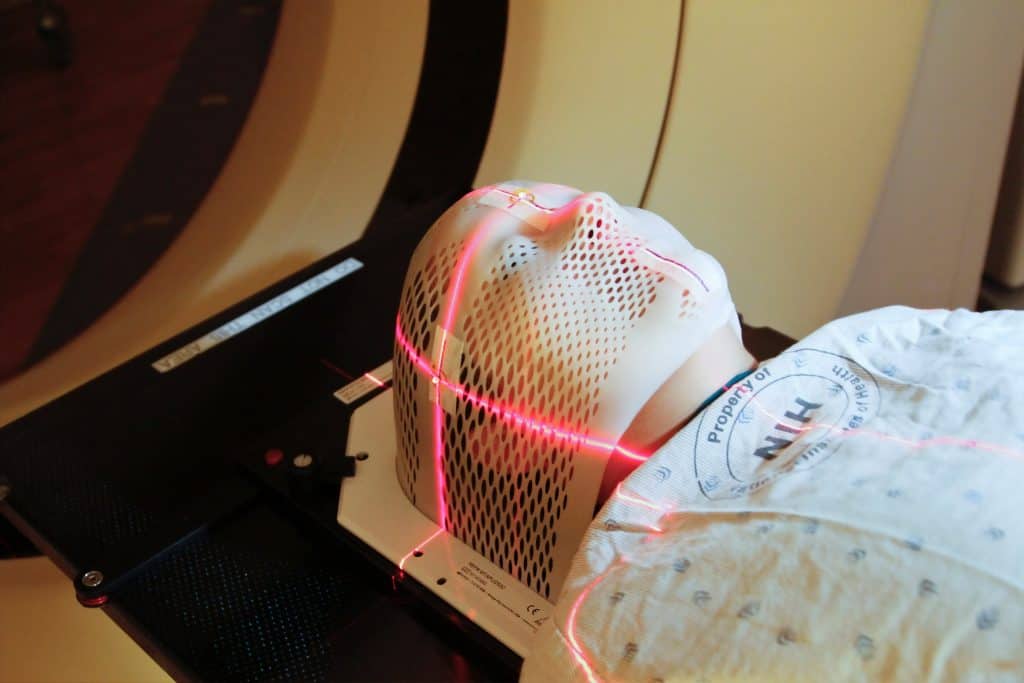
The current treatment option for patients diagnosed with GBM is surgery to remove the tumour (resection), followed by daily radiation and oral chemo for six and a half weeks, then a six-month regimen of oral chemotherapy given five days a month. Resection not only helps to relieve pressure in the brain but also prolongs overall survival rate, as demonstrated in studies as early as 2012.
In terms of chemotherapy, three chemotherapeutic agents are available to patients with glioblastoma – Temozolomide (TMZ), bevacizumab, and carmustine. Chemotherapy has only recently been introduced into the regimen for glioblastoma treatment, having previously been surgery followed by radiation.
The chemotherapy administered for glioblastoma is based on therapeutic targets found in preclinical studies, for example bevacizumab is an anti-VEGF monoclonal antibody. While it has been clinically observed that bevacizumab has anti-glioma activity with some improvement in progression-free survival (PFS) it has no significant impact on overall survival.
Challenges
One of the main challenges for treatment of GBM is not only the fragility of the brain, but the inability of most chemotherapeutic agents to cross the BBB. This barrier is not so much a static structure, but a wall of endothelial cells which actively select which molecules to pump in and out of the brain.
From an evolutionary standpoint, the BBB plays a huge role in protecting the brain from potential harmful substances. However, in terms of treatment, it can be counter-productive in preventing drugs being delivered to target sites in the brain.
A 2020 systematic literature search reinforced the issue of limited brain delivery of anticancer drugs. It found that “drug accumulation in the brain was low, due to limited penetration into the brain and a rapid efflux from the brain to the blood. For most targeted therapies, including monoclonal antibodies and tyrosine kinase inhibitors, penetration into the brain was barely detectable”.
Even if chemotherapeutic agents were able to successfully overcome the BBB, the bioavailability of a drug in the brain may be significantly limited as the drug is likely to be actively transported back out the BBB into circulation.
Other issues with current treatment is the implication of inoperable tumours. Surgery is the first-line option for glioblastoma, however the site of the tumour may not be operable depending on the brain region. In addition, brain surgery is a high risk operation with a number of potential complications for patients.
The need to develop effective pharmacological treatment could address some of the issues associated with resective surgery and offer hope for those who do not qualify for it due to tumour location in the brain.
Emerging area of research for drug delivery
Nanoparticles
Nanoparticles are natural or artificial particles ranging from 10 to 1000 nm in size, and are a popular area of focus for the drug delivery across the BBB. These particles have two main advantages:
- • First, they are taken up by the BBB via receptor-mediated or adsorptive-mediated pathway
- • Secondly, when administered systemically, nanoparticle encapsulation protects the drugs transported from damage.
Gold nanoparticles (GN) in particular are of key interest for drug delivery to brain tumours. According to a recent publication, preclinical “in vitro blood–brain barrier model, glucose-coated gold nanoparticles are taken up by brain-endothelium, and they target glial cells by passive diffusion”. The low toxicity and high loading capacity of GN-based nanocarriers make them attractive candidates for delivery of various payloads into the brain
A recent review investigated the efficacy of cisplatin conjugated gold nanoparticles (GNP-UP-Cis) as a drug delivery system for chemotherapeutic into the brain.
According to this review, in vivo models investigating GNP-UP-Cis have showed a great reduction in the growth of GBM tumours and magnetic resonance (MR)-guided focused ultrasound led to increased BBB permeability and gold nano-particle delivery in brain tissue. MR-guided focused ultrasound is an emerging platform with which researchers are investigating how ultrasound can impact the permeability of the BBB.
While nanoparticle drug delivery remains at the preclinical stage for chemotherapy targeting the brain, the success of some animal models over the last few years show potential for clinical applications in the future.
Charlotte Di Salvo, Lead Medical Writer
PharmaFeatures
Subscribe
to get our
LATEST NEWS
Related Posts

Immunology & Oncology
The Silent Guardian: How GAS1 Shapes the Landscape of Metastatic Melanoma
GAS1’s discovery represents a beacon of hope in the fight against metastatic disease.

Immunology & Oncology
Resistance Mechanisms Unveiled: The Role of Glutathione S-Transferase in Cancer Therapy Failures
Understanding this dual role of GSTs as both protectors and accomplices to malignancies is central to tackling drug resistance.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.
Designing Better Sugar Stoppers: Engineering Selective α-Glucosidase Inhibitors via Fragment-Based Dynamic Chemistry
One of the most pressing challenges in anti-diabetic therapy is reducing the unpleasant and often debilitating gastrointestinal side effects that accompany α-amylase inhibition.













