Diabetes is a metabolic disorder characterized by insufficient insulin production or action, primarily manifesting as Type 1 Diabetes (T1D) and Type 2 Diabetes (T2D). These conditions collectively impact over 500 million individuals worldwide, with projections estimating an increase to 1.3 billion by 2050. Under normal physiological conditions, pancreatic beta-cells respond dynamically to fluctuations in blood glucose levels by modulating insulin secretion. In instances of hypoglycemia, insulin secretion is inhibited, and glucagon, released from pancreatic alpha-cells, acts to restore glycemic balance. However, in diabetic patients, this glucose homeostasis is disrupted, necessitating regular insulin administration, which can lead to hypoglycemic episodes—a common and potentially dangerous complication. While traditional treatments have relied on glucagon for acute hypoglycemia management, emerging scientific concepts emphasize the importance of proactive strategies for hypoglycemia prevention.
Glucagon Delivery Systems
The landscape of glucagon delivery has evolved significantly, with various formulations and delivery systems emerging to enhance patient safety and efficacy. Traditional glucagon kits, which utilized lyophilized powders requiring reconstitution, have seen advances in formulation that include solubilizing the peptide at alkaline pH and employing new stabilizing additives. FDA-approved systems now encompass a nasal spray and a prefilled syringe of glucagon in dimethyl sulfoxide, showcasing innovative approaches to glucagon administration.
Recent studies have indicated that repeated glucagon doses do not lead to hepatic glycogen depletion, which raises the potential for smart delivery systems capable of sensing low glucose levels and releasing glucagon as a preventative measure. While glucose-responsive materials for insulin delivery have been extensively studied, glucagon delivery systems that respond to low glucose levels are still under development.
The concept of glucagon-responsive microneedle patches represents an exciting frontier in this field. These patches can deliver both insulin and glucagon in a controlled manner, presenting a multifaceted approach to diabetes management. Nevertheless, challenges persist, including ensuring that glucagon is only released in response to hypoglycemia without background release.
Glucagon-Polymer Conjugates
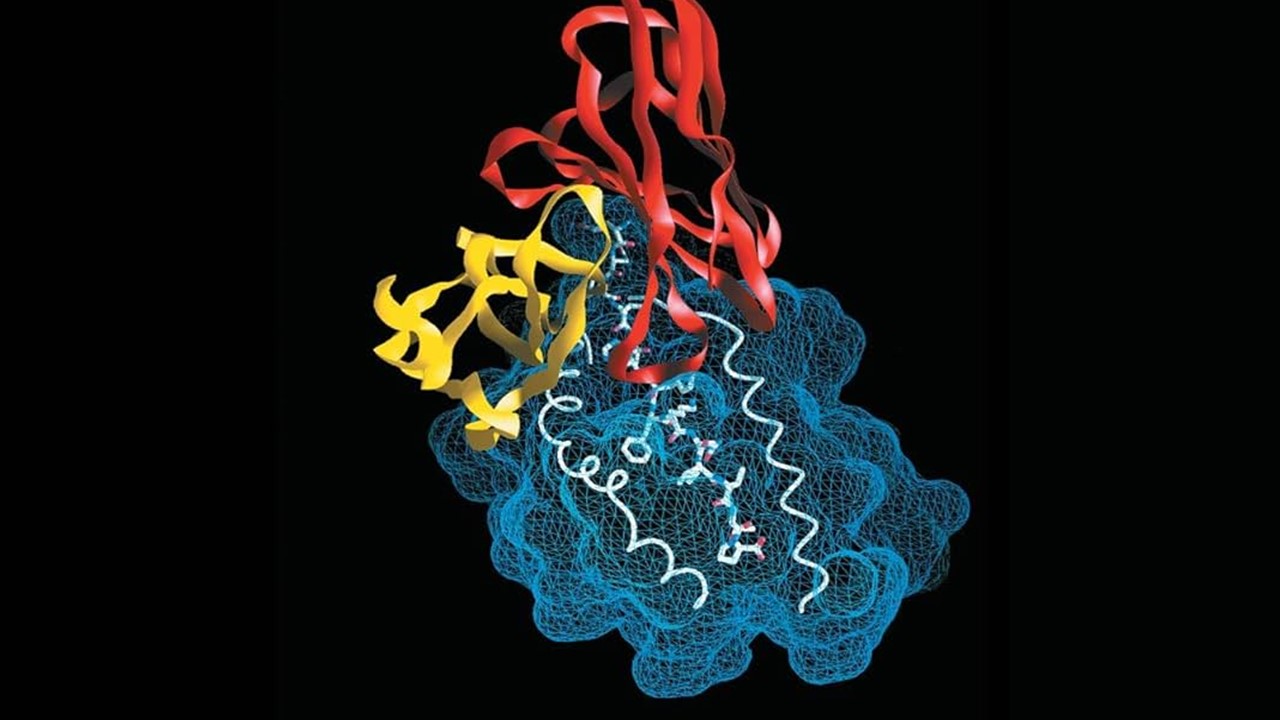
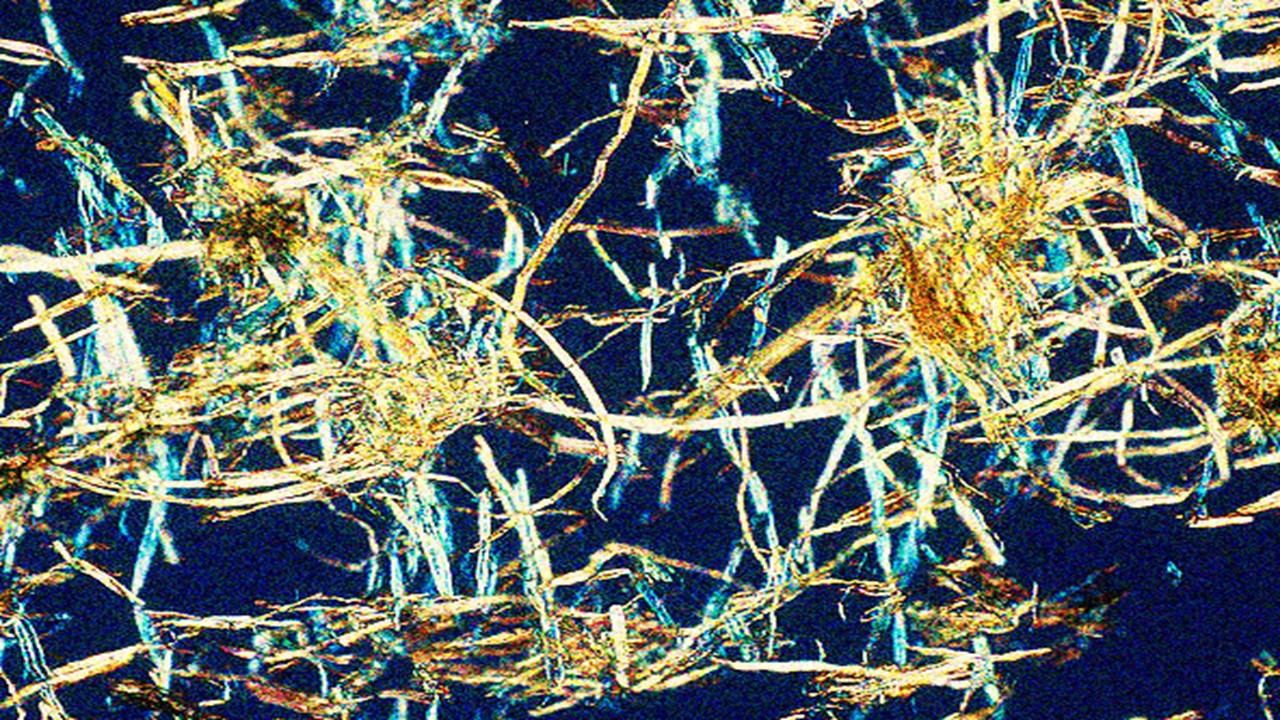
One innovative approach in glucagon delivery involves the use of glucagon-polymer conjugates, designed to release glucagon specifically in low glucose environments. This strategy takes advantage of the unique properties of 2-acrylamidophenylboronic acid (2-APBA), which can form stable complexes that respond to changes in glucose concentration. The incorporation of this boronic acid group allows for modulating the hydrophobicity of the material, leading to a controlled release mechanism.
In addition, the lower critical solution temperature (LCST) of thermoresponsive polymers, such as N-isopropylacrylamide copolymers, can be engineered to respond to physiological glucose levels. The LCST refers to the temperature at which a polymer transitions from a soluble to a dehydrated phase, influenced by the polymer’s hydrophobic characteristics. The ability to adjust the LCST is critical for ensuring that glucagon is released precisely when needed.
Furthermore, covalent grafting of glucagon onto polymer matrices via disulfide linkages ensures stability and bioactivity. This approach not only enhances the conjugate’s efficacy but also preserves the functional integrity of glucagon, enabling it to effectively interact with its receptor, thereby exerting its physiological effects.
Acute and Chronic Toxicity Evaluation
The acute toxicity of empty micelles (candidate polymer P2) was assessed in C57Bl/6J male mice through intraperitoneal injections at various time intervals. Complete blood count (CBC) and organ weights were measured, showing no significant differences compared to controls. A chronic toxicity study involved daily injections for 14 days, with similar results indicating no adverse effects on body weight, organ weights, or CBC counts. Histopathological analyses revealed no significant morphological changes in organs, affirming the safety profile of the polymeric material. These findings suggest that the empty micelles can be administered without immediate or long-term toxicity, which is crucial for their potential therapeutic applications.
In addition, immune markers and inflammation responses were evaluated to assess any immune reactions triggered by the micelles. No significant differences were found between treatment groups, indicating that the polymer does not provoke an adverse immune response. This comprehensive toxicity assessment strengthens the case for the use of these micelles in further studies and potential clinical applications, providing a reassuring safety profile for their use in drug delivery systems.
Pharmacokinetics via μPET/μCT Imaging
μPET/μCT imaging was conducted using 18F-labeled micelles and glucagon to investigate pharmacokinetics. The imaging results indicated higher organ uptake of glucagon compared to micelles, with more rapid renal clearance for the micelles. These findings suggest that labeling with different radiometals can influence biodistribution and that the micelles demonstrate a favorable pharmacokinetic profile. Importantly, the imaging results also highlighted the potential for micelle formulations to achieve targeted delivery while minimizing off-target effects, a significant advantage in therapeutic applications.
Furthermore, the imaging studies provide insight into the behavior of the micelles in vivo, offering valuable data on how these systems can be optimized for enhanced drug delivery. The different clearance rates observed for the micelles compared to glucagon may indicate a more controlled release profile, which is essential for maintaining therapeutic levels of glucagon while reducing the risk of hyperglycemia. This detailed understanding of pharmacokinetics is crucial for the development of effective and safe drug delivery systems that can respond dynamically to physiological changes.
In Vivo Efficacy of GCG-Micelles
The efficacy of PEG-b-P(NIPAM-stat-2-APBA)-GCG micelles was evaluated in reversing insulin-induced hypoglycemia in mice. After administration of glucagon-conjugated micelles, blood glucose levels were restored to baseline within 25 minutes. Additionally, simultaneous injection of insulin and micelles effectively maintained normoglycemia, while control groups experienced significant drops in glucose levels. This indicates the potential of GCG-micelles as a responsive treatment to manage glycemia in hypoglycemic conditions. The quick restoration of blood glucose levels underscores the micelles’ effectiveness as an emergency intervention for hypoglycemic episodes.
Moreover, these findings suggest that the glucagon micelles may offer a more controlled and reliable approach to managing blood sugar levels, particularly for patients at risk of hypoglycemia. The ability of GCG-micelles to respond appropriately under varying glucose levels emphasizes their potential utility in clinical settings, where patients require rapid interventions. The overall results encourage further investigation into the micelle formulations, potentially leading to innovative treatment strategies for diabetes management and improved patient outcomes in glycemic control.
Promising Horizons: The Future of Glucagon Micelles
The exploration of glucagon-responsive micelles and polymer conjugates offers a promising advancement in the field of diabetes management, aiming to provide a proactive strategy for preventing hypoglycemia. By harnessing the principles of polymer chemistry and glucose-responsive materials, these systems can facilitate controlled glucagon release in response to low glucose levels. This innovative approach holds the potential to significantly improve patient outcomes, paving the way for further advancements in diabetes therapy.
Study DOI: https://doi.org/10.1021/acscentsci.4c00937
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts
Medicinal Chemistry & Pharmacology
Aerogel Pharmaceutics Reimagined: How Chitosan-Based Aerogels and Hybrid Computational Models Are Reshaping Nasal Drug Delivery Systems
Simulating with precision and formulating with insight, the future of pharmacology becomes not just predictive but programmable, one cell at a time.
Medicinal Chemistry & Pharmacology
Coprocessed for Compression: Reengineering Metformin Hydrochloride with Hydroxypropyl Cellulose via Coprecipitation for Direct Compression Enhancement
In manufacturing, minimizing granulation lines, drying tunnels, and multiple milling stages reduces equipment costs, process footprint, and energy consumption.

Medicinal Chemistry & Pharmacology
Decoding Molecular Libraries: Error-Resilient Sequencing Analysis and Multidimensional Pattern Recognition
tagFinder exemplifies the convergence of computational innovation and chemical biology, offering a robust framework to navigate the complexities of DNA-encoded science