Trip Down the Bango Lane
In the middle of the 1960s, British scientist Alec Bangham and colleagues at Babraham Cambridge established the science of liposomology. In 1964, they released the first study describing the structure of liposomes.
Originally known as bangosomes, liposomes are phospholipid-based drug vesicles that self-assemble into a bilayer (uni-lamellar) or a concentric series of several bilayers (multi-lamellar) to enclose an aqueous compartment in the middle. Liposomes can be as small as 30 nm or as large as microns, having a phospholipid bilayer that is 4-5 nm thick.
Liposomes are fundamentally a subclass of amphiphilic nanoparticles with a hydrophobic tail and a hydrophilic head that make up a phospholipid membrane. Liposomes are very lipid-rich spherical or multilayered spherical structures that can be classified according to a wide range of factors, such as structural characteristics, structural parameters, size, manufacturing techniques, preparation, and drug loading.
Exploiting Entrapment Properties
The idea that liposomes can entrap pharmaceuticals and be employed as medication delivery devices was first put out by pioneers like Gregoriadis and Perrie.
The anti-cancer medication cytosine arabinoside was first used to show in vivo activity of liposome-entrapped medicines in animal models by showing measurable increases in the survival periods of mice with L1210 leukemia. As a result, liposomes have gained traction as a “model system” for investigating the impact of a wide range of liposome properties on therapeutic benefits.
Since then, a lot of research has been done on the use of liposomes as delivery systems for small-molecule medications, proteins, nucleic acids, and imaging agents. To increase treatment efficacy and patient compliance, various delivery routes, including parenteral, pulmonary, oral, transdermal, ocular, and nasal routes, have been devised. Liposomes have also been extensively used in the food and cosmetics industries.
Liposomes: The New Biomolecular UPS
Liposomes, as novel drug delivery systems, can be employed as carriers for a variety of medicinal molecules, including chemotherapeutic agents, antibacterial and antiviral medications, antiparasitic treatments, genetic material, vaccines, therapeutic proteins, and anti-inflammatory therapies because they are bimolecular vesicles.
When used as drug delivery systems, liposomes display exceptional qualities such as preventing the encapsulated materials from physiological deterioration, prolonging the drug’s half-life, regulating the release of drug molecules, and having great biocompatibility and safety. Additionally, by using passive or active targeting, liposomes can transport their payload to the sick location with greater precision, reducing systemic adverse effects while increasing the maximum tolerated dose and enhancing therapeutic outcomes.
Enhancing Pharmacokinetic Profiles
When administered without a drug delivery system (DDS), many medications call for regular doses. Liposomes, on the other hand, can be designed to have a lengthy circulating time in the body, maintaining the drug’s consistent level for a longer period of time. The fluidity of the membrane, the size of the liposomes (smaller liposomes circulate longer), and the charge on the liposomes are all factors that affect the duration of circulation (neutral liposomes have a long circulation time).
Some medications are shielded by liposomes from enzyme action as well as immune system and chemical destruction. Because of the sustained drug levels provided by liposomes, especially when so-called “stealth” liposomes are utilized, toxicity is reduced and needed dose is reduced.
Fearing the Enzyme No More
Because the lipids utilized in the liposomal formulation are sufficiently resistant to enzymatic degradation, the encapsulated medicine can be protected by the liposomes while they are in circulation. By membrane diffusion or lysosomal degradation of the lipid membrane, the medication is liberated from the liposome as it enters the cell.
Additionally, liposomes can help a number of things move more easily through the digestive system and safeguard the medications they have contained.
Liposomes can be employed as vaccine delivery systems due to their advantages of biodegradability and non-toxicity. Liposomes are a promising choice for oral vaccination delivery due to the protective effects of loaded compounds.
It’s Better When It’s Oral
Bile, pH levels, and pancreatic enzymes in the gastrointestinal environment are said to be the key variables determining the stability of oral medications.
Medications can be protected from the gastrointestinal environment and have their oral bioavailability increased by creating microemulsions utilizing liposomes as suspensions or solubilizers for very insoluble or lipophilic drugs. Liposome-antigen formulations may also improve antigen delivery to cells that present antigens when taken orally.
Inhale, Bronchi No Ail
Proteins and peptides, two common types of medications, are highly unstable and breakdown in an unfavorable gastrointestinal environment. For such delicate medications, pulmonary administration is the best and most appropriate route of administration.
Liposomal formulations have benefits over non-encapsulated drug aerosols as pulmonary medication delivery systems. The topical and systemic therapeutic effects of medications can be prolonged by pulmonary delivery of drug-loaded liposomes. Similar to this, liposomal DDS makes intracellular drug administration easier, particularly in tumor cells, alveolar macrophages, and epithelial cells. Additionally, this DDS lessens drug toxicity and prevents topical stimulation of lung tissue.
The most important benefit of liposome formulations for pulmonary administration application is the targeting of particular cell populations using surface-bound ligands or antibodies.
Antibiotic Shield On!
Antibiotics’ ability to treat patients effectively is hampered by a number of circumstances. Antibiotics are degraded by enzymes, which is a critical feature.
Poor clinical results are caused by the high vulnerability of cephalosporin and penicillin to hydrolysis by β-lactamases.
Liposome encapsulation of antibiotics is a crucial strategy to prevent this breakdown. Similar to this, the liposomal administration of antibiotics boosts cellular absorption, lowers the effective dose indicated, and delays the onset of dose-dependent toxicity.
Integument Loading? No Problem.
Due to the fact that liposomes require very minimal quantities when used as topical formulations, they can lessen the negative effects of topical medications. Additionally, they make the skin more permeable to the loaded medication.
In skincare and cosmetic applications, liposomes are found to be crucial as well. The lipid characteristics of the vesicles as drug carriers are responsible for the improved skin absorption of medications.
Oncology, Ever Better
Liposomes are also employed to transport chemotherapeutic agents, which minimizes cytotoxic effects in the skin and heart.
In studies involving animals, the liposomal DDS group had a greater survival rate than the group receiving free anticancer drug molecules.
Drug-loaded liposomes have been shown in similar investigations to boost the chemotherapeutic drug concentration in tumor tissue. Drugs administered by liposomes have better anticancer effects on solid tumors than free drug molecules.
By selectively delivering particular ligands to antigens expressed on cancerous cells, liposomal targeting of anticancer medicines can be further enhanced. The strategy not only enhances the therapeutic outcomes but also lessens the negative effects of chemotherapy.
Subscribe
to get our
LATEST NEWS
Related Posts

Medicinal Chemistry & Pharmacology
Aerogel Pharmaceutics Reimagined: How Chitosan-Based Aerogels and Hybrid Computational Models Are Reshaping Nasal Drug Delivery Systems
Simulating with precision and formulating with insight, the future of pharmacology becomes not just predictive but programmable, one cell at a time.

Medicinal Chemistry & Pharmacology
Coprocessed for Compression: Reengineering Metformin Hydrochloride with Hydroxypropyl Cellulose via Coprecipitation for Direct Compression Enhancement
In manufacturing, minimizing granulation lines, drying tunnels, and multiple milling stages reduces equipment costs, process footprint, and energy consumption.

Medicinal Chemistry & Pharmacology
Decoding Molecular Libraries: Error-Resilient Sequencing Analysis and Multidimensional Pattern Recognition
tagFinder exemplifies the convergence of computational innovation and chemical biology, offering a robust framework to navigate the complexities of DNA-encoded science
Read More Articles
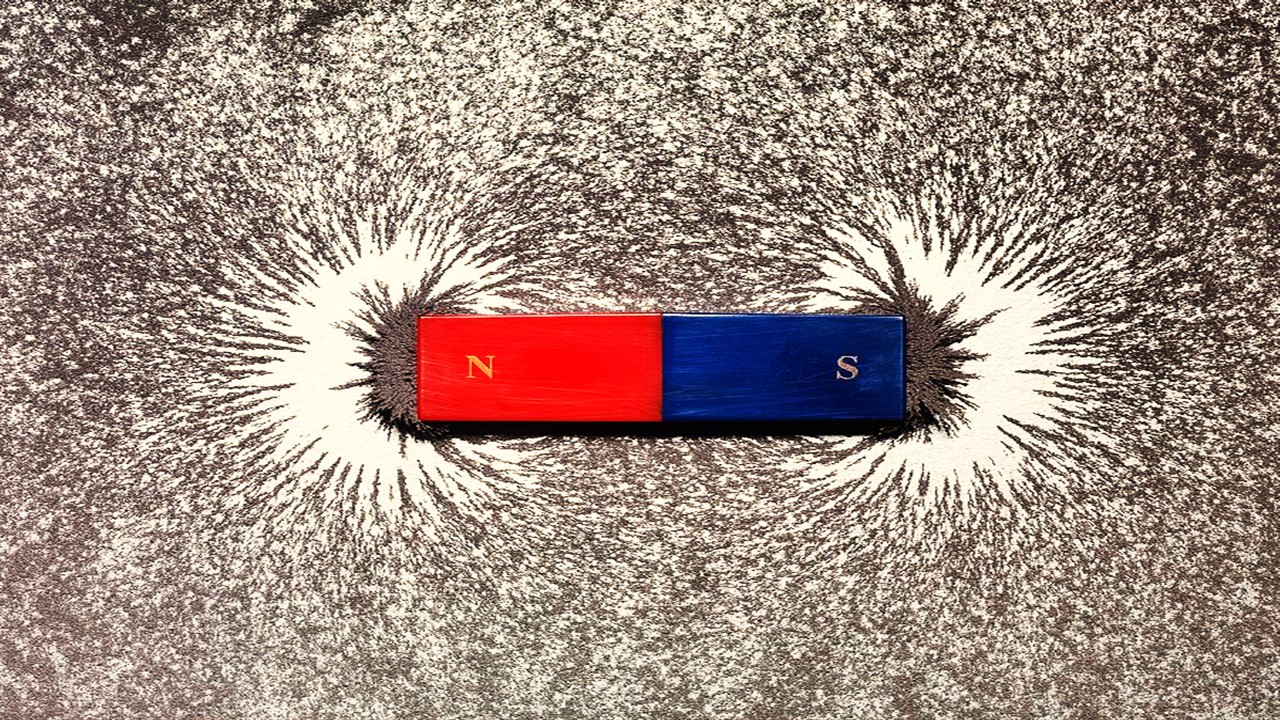
Magnetic Nanoengineering: Overcoming Biological Variability and Enhancing Therapeutic Precision
The future of nanomedicine lies in harmonizing precision, accessibility, and ecological responsibility, ushering in an era where therapies are tailored to individual biological landscapes.
Trials, Triumphs, and Trials Ahead: Navigating the Landscape of Randomized Controlled Trials in Artificial Intelligence-Driven Healthcare
The adoption of artificial intelligence in clinical practice has prompted a surge in randomized controlled trials, highlighting a balance of enthusiasm and prudence.
Illuminating the Dark Genome: Uncharted Frontiers in Therapeutic Discovery
The dark genome is not a biological void but a frontier awaiting illumination.