It has long been recognized that acetylcholine controls hemoperfusion (blood flow) and is an important neurotransmitter in the neurological system. Nevertheless, the origin of the acetylcholine found in human blood is still unknown. According to a study by Karolinska Institutet, it was recently discovered that specific T cells in human blood can create acetylcholine. This finding has profound implications for inflammatory and cardiovascular illnesses.
Cholinergic Chemistry
Acetylcholine is a small organic molecule that belongs to the class of neurotransmitters, which are chemical messengers that transmit signals between neurons, as well as between neurons and other cells. Acetylcholine is composed of two basic building blocks, an acetyl group and a choline molecule. The acetyl group is derived from acetyl-CoA, which is synthesized in the mitochondria of cells through a series of metabolic reactions. Choline, on the other hand, is obtained from the diet and is a precursor for acetylcholine synthesis. Once acetylcholine is synthesized, it is stored in vesicles in the axon terminals of neurons and is released into the synapse upon depolarization of the presynaptic neuron.
In order to carry out its job, acetylcholine has to bind to specific targets on the postsynaptic cell. This binding results in a change in the cell’s membrane potential, which can be either excitatory or inhibitory depending on the kind of receptor activated. Numerous physiological functions, such as muscular contraction, heart rate control, stimulation of glandular secretion, and attention and memory modulation, involves acetylcholine.
The Role of Acetylcholine in Inflammation
Inflammation is a key process in the immune response to injury or infection, but excessive inflammation can lead to tissue damage and contribute to the development of chronic diseases such as atherosclerosis, rheumatoid arthritis, and diabetes.
Acetylcholine has a crucial role in the control of inflammation in addition to its function as a neurotransmitter. It has been demonstrated that acetylcholine can prevent immune cells such monocytes, macrophages, and T cells from secreting pro-inflammatory cytokines. Acetylcholine is hypothesized to have an anti-inflammatory influence through binding to nicotinic acetylcholine receptors on immune cells, which inhibits signaling pathways that cause inflammation. Acetylcholine can also activate a subpopulation of T cells known as choline acetyltransferase (ChAT)+ T cells, which can make their own acetylcholine and control blood vessel endothelial function, helping to further control inflammation.
The new study by Karolinska Institutet demonstrates that immune cells known as ChAT+ T cells can secrete acetylcholine, which can regulate inflammation in the blood vessels.
The Importance of ChAT+ T Cells in Human Blood
ChAT+ T cells have been previously identified in mice and have been shown to affect endothelial cells in the blood vessels. The recent discovery that ChAT+ T cells also exist in human blood and can produce acetylcholine opens up new possibilities for understanding the regulation of blood flow and inflammation in humans. The researchers at Karolinska Institutet analyzed blood from healthy donors and found that ChAT+ T cells were present in human blood.
Clinical Implications of the Study
Additionally, the research examined the blood of 33 critically sick patients with circulatory failure and discovered that larger levels of ChAT+ T cells were linked to a lower probability of passing away. This implies that ChAT+ T cells may play a protective function in inflammatory and cardiovascular disorders. The existence of ChAT+ T cells in various patient populations and organs, as well as how these cells influence inflammatory and metabolic processes, will be further investigated, the researchers expect.
Diagnostic and Therapeutic Potentials
The recent study by Karolinska Institutet sheds new light on the regulation of blood flow and inflammation by acetylcholine. The discovery of ChAT+ T cells in human blood that can produce acetylcholine has important implications for the development of new diagnostic and therapeutic approaches for cardiovascular and inflammatory diseases. Patients with higher relative blood levels of ChAT+ T cells had a lower risk of death, suggesting that measuring these cells in patients with cardiovascular and inflammatory diseases could serve as a diagnostic tool for predicting disease severity and prognosis.
The study also demonstrates that acetylcholine in the blood can control blood vessel inflammation, suggesting that medications that target the cholinergic system may one day be created for the treatment of inflammatory illnesses. In addition, the researchers’ intention to map the distribution of ChAT+ T cells across various patient populations and organs may point to new therapeutic targets.
Further research is needed to fully understand the role of ChAT+ T cells in disease pathogenesis and to explore the potential of cholinergic-targeted therapies.
Study DOI: pnas.org/doi/10.1073/pnas.2212476120
Subscribe
to get our
LATEST NEWS
Related Posts

Immunology & Oncology
The Silent Guardian: How GAS1 Shapes the Landscape of Metastatic Melanoma
GAS1’s discovery represents a beacon of hope in the fight against metastatic disease.
Immunology & Oncology
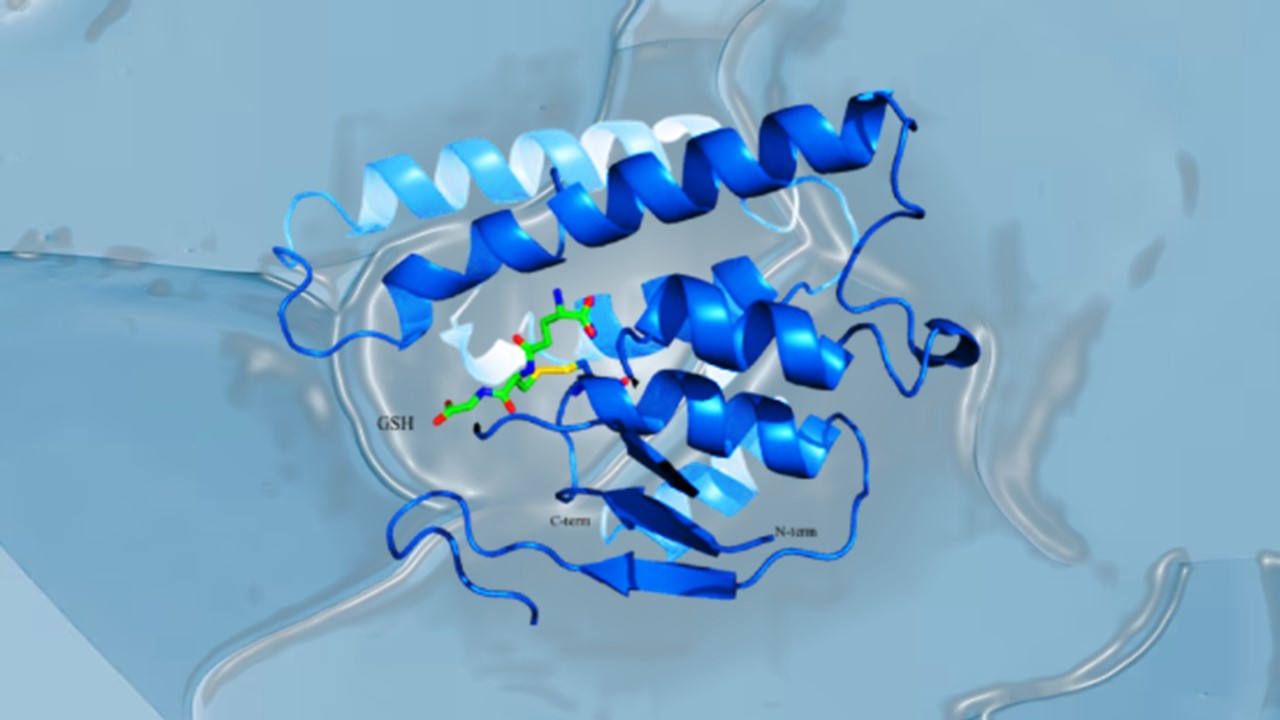
Resistance Mechanisms Unveiled: The Role of Glutathione S-Transferase in Cancer Therapy Failures
Understanding this dual role of GSTs as both protectors and accomplices to malignancies is central to tackling drug resistance.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.
Designing Better Sugar Stoppers: Engineering Selective α-Glucosidase Inhibitors via Fragment-Based Dynamic Chemistry
One of the most pressing challenges in anti-diabetic therapy is reducing the unpleasant and often debilitating gastrointestinal side effects that accompany α-amylase inhibition.