The Epstein-Barr virus (EBV) is a widely prevalent virus transmitted through bodily fluids, including saliva, and infects over 90% of the global population. While most infections remain asymptomatic or cause mild ailments, EBV can establish latent infections that may reactivate over time, leading to chronic inflammatory conditions and various cancers. In a recent publication in the prestigious journal Nature, researchers from the University of California San Diego shed light on how EBV exploits genomic vulnerabilities to drive cancer development while undermining the body’s ability to suppress it.
EBV Spotlight
A ubiquitous herpesvirus that infects humans, EBV is responsible for causing infectious mononucleosis, also known as glandular fever or the “kissing disease.” This illness typically presents with symptoms like fever, sore throat, swollen lymph nodes, and fatigue. However, many EBV infections are asymptomatic, meaning individuals may not show any noticeable signs of illness.
Following the initial infection, EBV can enter a dormant or inactive state within the body, living in specific cells, most notably B lymphocytes. The virus remains dormant during latency and does not generate active infection or symptoms. However, under some conditions, such as a compromised immune system, the virus might reactivate and begin reproducing once more.
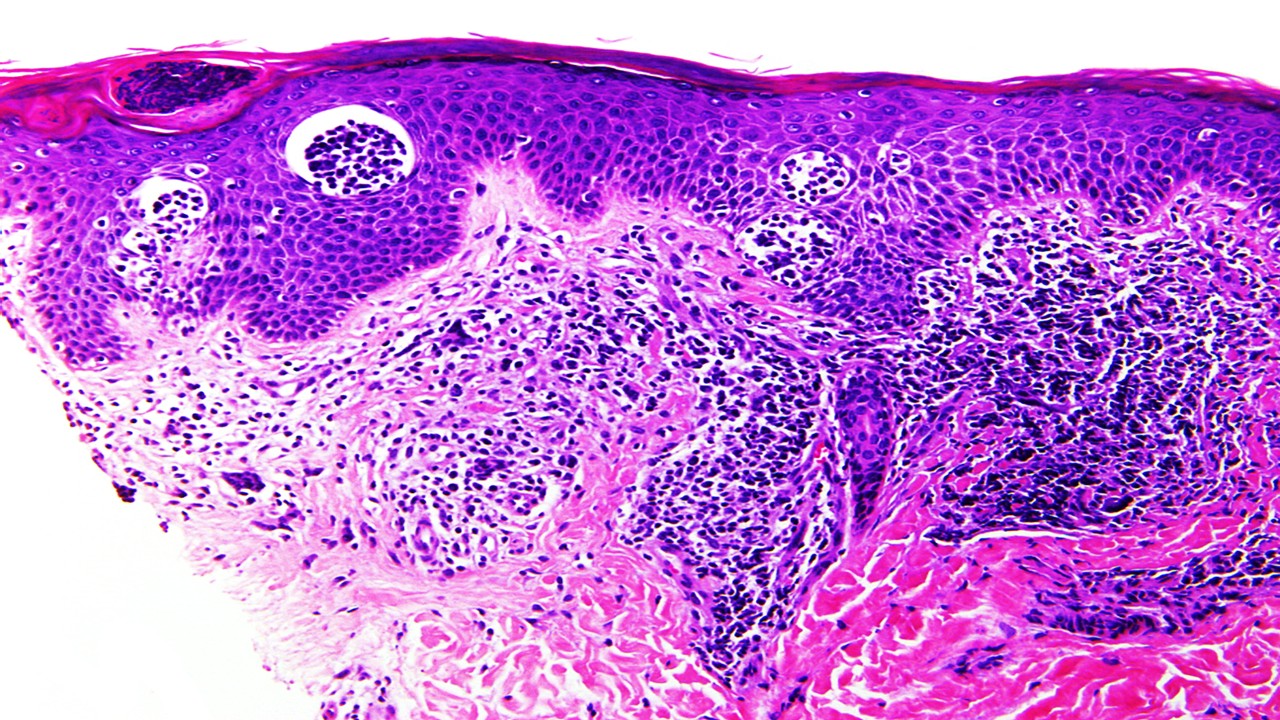
Long-term latent EBV infections have been associated with several chronic inflammatory conditions and various cancers. These include certain types of lymphomas (cancers of the lymphatic system), nasopharyngeal carcinoma (a type of head and neck cancer), and some stomach cancers. The mechanisms by which EBV contributes to cancer development are still being actively researched.
While EBV is extremely common, the vast majority of infections do not result in severe illness or malignancy. The immune system of the body is normally capable of regulating the virus and avoiding illness progression. However, EBV can be more dangerous in people who have weakened immune systems or are genetically predisposed.
Understanding the biology and behavior of EBV is critical for establishing prevention and management methods for related illnesses. Ongoing research aims to elucidate the virus’s intricate interactions with the human immune system, as well as the processes through which EBV promotes cancer formation.
Unveiling the Manipulation
By inducing cleavage of human chromosome 11, the researchers demonstrated how EBV triggers genomic instability, potentially activating oncogenes associated with leukemia and inactivating crucial tumor suppressor genes. This groundbreaking discovery reveals the selective induction of cleavage at fragile DNA sites, illuminating the mechanisms employed by the virus to promote cancerous transformations.
The Role of EBNA1 Protein
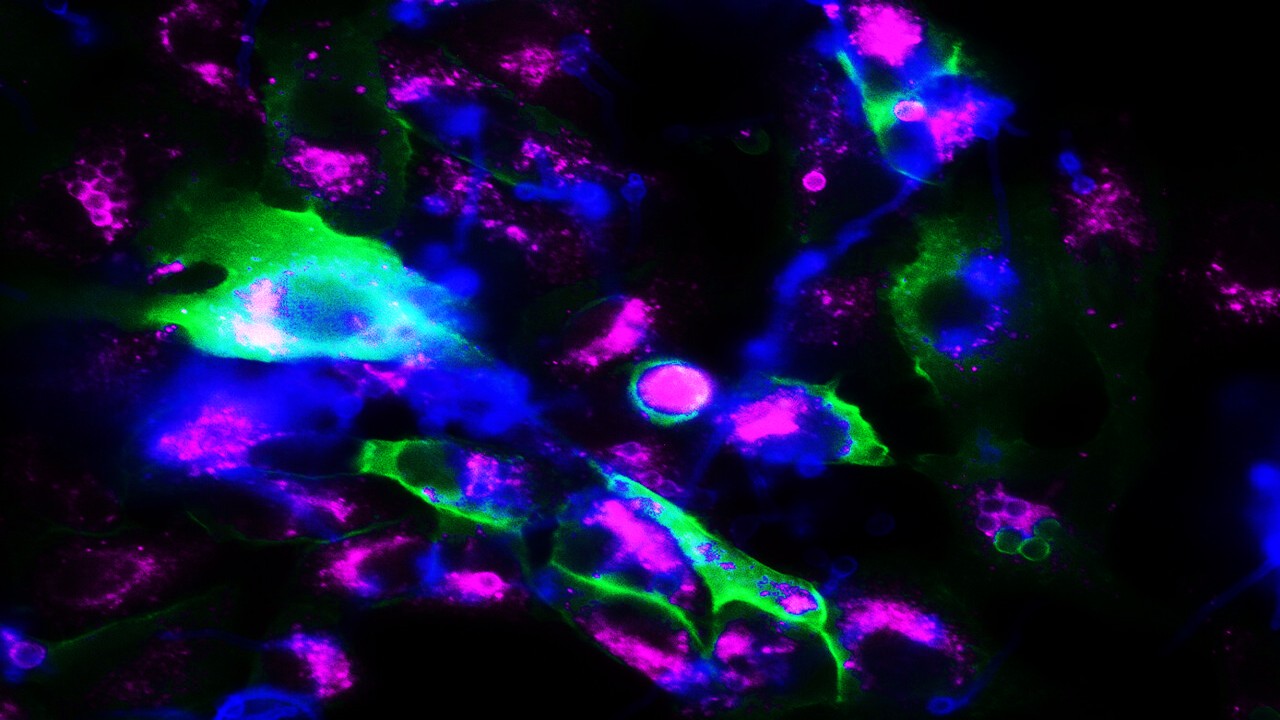
The study focused on EBNA1. Epstein-Barr nuclear antigen 1 (EBNA1) is a multifunctional dimeric viral protein that is related with Epstein-Barr virus (EBV). It is the only EBV protein that is detected in all EBV-related cancers. While previous research identified EBNA1’s binding at specific genomic sequences in the EBV genome, this investigation uncovered its binding to a cluster of EBV-like sequences at a fragile site on human chromosome 11. The abundance of EBNA1 at this site was found to trigger chromosomal breakage, further unraveling the virus’s influence on genomic stability.
Interplay with Tumor Suppression
EBNA1 also plays a significant role in inhibiting the function of p53, a crucial gene involved in regulating cell division and cell death. In its normal state, p53 acts as a tumor suppressor, preventing uncontrolled cell growth. However, mutations in p53 have been associated with cancer development. The researchers found that cancer tumors with detectable EBV exhibited higher levels of chromosome 11 abnormalities, particularly in head and neck cancer cases, emphasizing the impact of EBV-induced genomic instability on cancer progression.
Implications for Personalized Risk Assessment
While EBV is generally harmless for most individuals, identifying those at risk of developing latent infection-associated diseases remains an ongoing challenge. The study’s findings suggest that susceptibility to EBNA1-induced fragmentation of chromosome 11 depends on the control of EBNA1 levels in latent infection and the genetic variability of EBV-like sequences on chromosome 11 in each individual. This newfound knowledge opens avenues for screening individuals for risk factors associated with EBV-associated diseases and exploring strategies to block EBNA1 binding to prevent the development of such conditions.
Conclusion
The groundbreaking research conducted by the scientists at the University of California San Diego offers valuable insights into the mechanisms employed by EBV to exploit fragile genomic sites, promoting cancerous transformations and evading tumor suppression mechanisms. By unraveling the interplay between EBV and human chromosomes, this study paves the way for personalized risk assessment and the development of targeted interventions to combat EBV-associated diseases.
Study DOI: 10.1038/s41586-023-05923-x
Subscribe
to get our
LATEST NEWS
Related Posts

Infectious Diseases & Vaccinology
Enduring Blockade: Five-Year Functional Antibody Persistence Against Emerging GII.4 and GII.17 Noroviruses
Natural infection with dominant GII noroviruses elicits long-lived functional antibodies, redefining immune durability in viral gastroenteritis.
Infectious Diseases & Vaccinology
Resistant Mycosis: Reimagining Antifungal Therapy Through Mechanistic Innovation and Molecular Disruption
Emerging antifungal strategies are redefining treatment by targeting fungal physiology through diversified, mechanism-driven approaches that overcome entrenched drug resistance.
Infectious Diseases & Vaccinology
Fungal Refractory States: Deciphering Pathobiology and Therapeutic Weaknesses in the Era of Rising Antifungal Resistance
Rising antifungal resistance reflects a multidimensional biological challenge that demands mechanistically innovative, host-integrated therapeutic strategies.

Infectious Diseases & Vaccinology
Epigenetic Parasite Vulnerabilities: Repurposing Histone Deacetylase Inhibitors for Complex Multispecies Therapeutics
Repurposed HDAC inhibitors target essential parasite epigenetic machinery, offering a powerful but complex frontier for next-generation antiparasitic therapy.
Read More Articles
Spatial Collapse: Pharmacologic Degradation of PDEδ to Disrupt Oncogenic KRAS Membrane Localization
PDEδ degradation disrupts KRAS membrane localization to collapse oncogenic signaling through spatial pharmacology rather than direct enzymatic inhibition.
Neumedics’ Integrated Innovation Model: Dr. Mark Nelson on Translating Drug Discovery into API Synthesis
Dr. Mark Nelson of Neumedics outlines how integrating medicinal chemistry with scalable API synthesis from the earliest design stages defines the next evolution of pharmaceutical development.
Zentalis Pharmaceuticals’ Clinical Strategy Architecture: Dr. Stalder on Data Foresight and Oncology Execution
Dr. Joseph Stalder of Zentalis Pharmaceuticals examines how predictive data integration and disciplined program governance are redefining the future of late-stage oncology development.
Exelixis Clinical Bioanalysis Leadership, Translational DMPK Craft, and the Kirkovsky Playbook
Senior Director Dr. Leo Kirkovsky brings a rare cross-modality perspective—spanning physical organic chemistry, clinical assay leadership, and ADC bioanalysis—to show how ADME mastery becomes the decision engine that turns complex drug systems into scalable oncology development programs.
Policy Ignition: How Institutional Experiments Become Durable Global Evidence for Pharmaceutical Access
Global pharmaceutical access improves when IP, payment, and real-world evidence systems are engineered as interoperable feedback loops rather than isolated reforms.







