Achieving immune reconstitution necessitates a comprehensive understanding of the intricate network comprising immune cells, cytokines, and signaling pathways. This multifaceted process entails the replenishment of immune cell populations and the restoration of immune homeostasis, encompassing a complex interplay of cellular and molecular events. An in-depth exploration of the processes involved in immune reconstitution unveils the remarkable regenerative capacities and regulatory mechanisms that underlie the restoration of immune function.
Replenishing Immune Cell Populations
Replenishing immune cell populations is a fundamental aspect of immune reconstitution. This process often involves the restoration of lymphocyte subsets, including T cells, B cells, and natural killer (NK) cells, which play vital roles in mounting effective immune responses. Hematopoietic stem cell transplantation (HSCT) represents a prominent approach for immune cell replenishment in cases of severe immunodeficiencies or bone marrow failure. HSCT involves the infusion of donor-derived hematopoietic stem cells, which possess the remarkable ability to differentiate into various immune cell lineages. As these stem cells engraft in the recipient’s bone marrow, they reconstitute the immune system by generating functional immune cells.
Restoring Immune Homeostasis
The restoration of immune homeostasis is equally crucial for immune reconstitution. This process involves fine-tuning immune responses, ensuring a balanced and coordinated reaction to pathogens while preventing excessive inflammation or autoimmunity. Several factors contribute to immune homeostasis, including the harmonious interplay of immune cell subsets, the regulation of cytokine networks, and the maintenance of immune tolerance.
Collaboration of Immune Cell Subsets in Immune Homeostasis
Immune cell subsets collaborate to orchestrate immune responses with precision and efficiency. T cells, for instance, exhibit diverse functions mediated by distinct subsets, such as effector T cells, regulatory T cells (Tregs), and memory T cells. Effector T cells execute targeted immune responses against pathogens, while Tregs suppress excessive immune activation and promote immune tolerance. Memory T cells, on the other hand, provide long-lasting protection by facilitating rapid and robust responses upon re-exposure to previously encountered pathogens. The restoration of appropriate ratios and functions of these immune cell subsets is essential for immune homeostasis.
Role of Cytokines in Immune Regulation
Cytokines, small signaling proteins, play pivotal roles in immune regulation and the restoration of immune homeostasis. They orchestrate immune cell communication, activation, and differentiation, shaping the immune response according to specific needs. For instance, interleukins such as IL-2, IL-7, and IL-15 are critical for T cell development, survival, and proliferation. These cytokines facilitate the expansion of T cell populations and contribute to immune reconstitution following lymphopenia or HSCT. Moreover, cytokines such as IL-10 and TGF-β exert immunoregulatory functions by dampening immune responses and promoting immune tolerance. Restoring the delicate balance of cytokines is essential for immune homeostasis and effective immune reconstitution.
Immune Tolerance and Regulatory T Cells
Immune tolerance, a central pillar of immune homeostasis, prevents the immune system from mounting harmful responses against self-antigens. Regulatory T cells (Tregs) are key orchestrators of immune tolerance, suppressing excessive immune activation and maintaining immune equilibrium. Tregs achieve this through various mechanisms, including the secretion of immunosuppressive cytokines (e.g., IL-10 and TGF-β), direct cell-to-cell contact, and modulation of antigen-presenting cells. The restoration and proper function of Tregs are crucial for immune reconstitution, as they help prevent autoimmune reactions and promote immune tolerance.
Addressing Dysregulated Cytokine Networks and Inflammation
Furthermore, the restoration of immune homeostasis involves addressing dysregulated cytokine networks and inflammatory processes. Chronic inflammation can disrupt immune responses, compromise tissue integrity, and impede immune reconstitution. Modulating inflammatory responses through targeted interventions, such as anti-inflammatory cytokines or anti-inflammatory agents, can help restore immune homeostasis and create a favorable environment for immune reconstitution.
Achieving successful immune reconstitution relies on a comprehensive understanding of the interplay between immune cell populations, cytokines, and regulatory mechanisms. Through the replenishment of immune cell populations and the restoration of immune homeostasis, the immune system can regain its functionality and mount effective immune responses against pathogens. The evolving field of immune reconstitution research continues to unravel the intricate cellular and molecular processes involved, paving the way for innovative therapeutic approaches and improved outcomes in various immunodeficiencies and immune-related disorders.
Engr. Dex Marco Tiu Guibelondo, BS Pharm, RPh, BS CpE
Subscribe
to get our
LATEST NEWS
Related Posts

Immunology & Oncology
The Silent Guardian: How GAS1 Shapes the Landscape of Metastatic Melanoma
GAS1’s discovery represents a beacon of hope in the fight against metastatic disease.
Immunology & Oncology
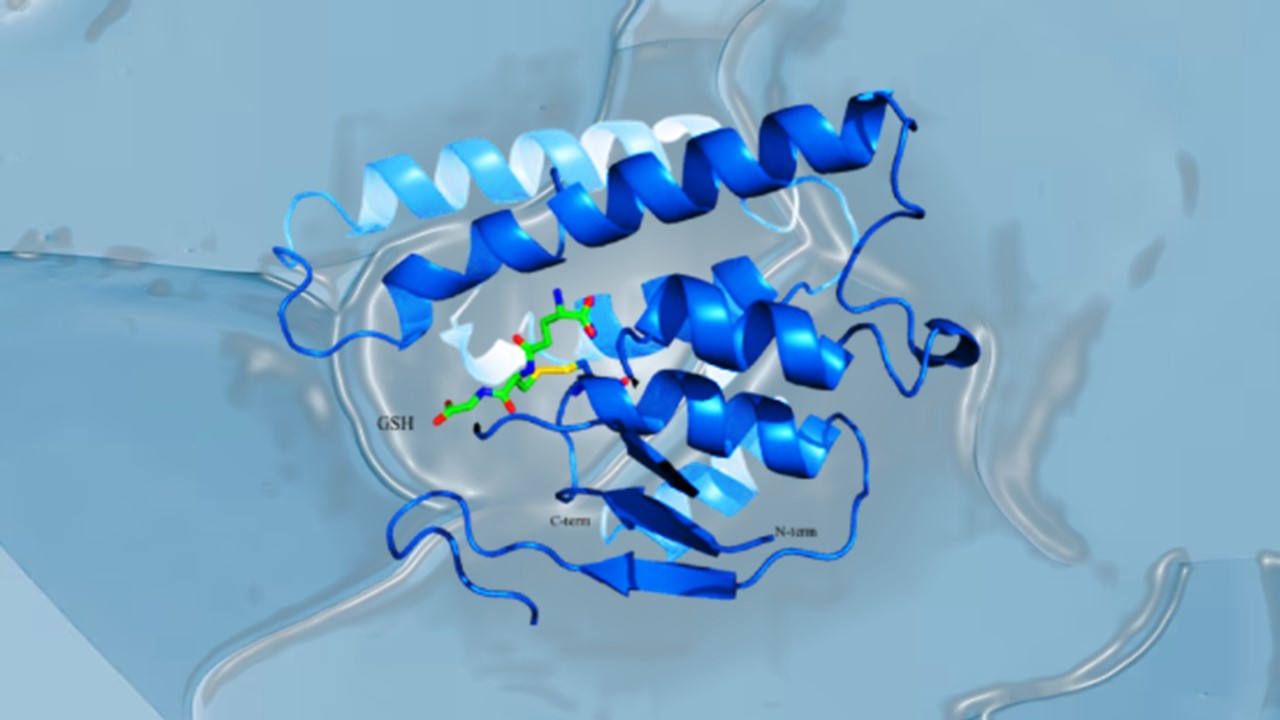
Resistance Mechanisms Unveiled: The Role of Glutathione S-Transferase in Cancer Therapy Failures
Understanding this dual role of GSTs as both protectors and accomplices to malignancies is central to tackling drug resistance.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.
Designing Better Sugar Stoppers: Engineering Selective α-Glucosidase Inhibitors via Fragment-Based Dynamic Chemistry
One of the most pressing challenges in anti-diabetic therapy is reducing the unpleasant and often debilitating gastrointestinal side effects that accompany α-amylase inhibition.