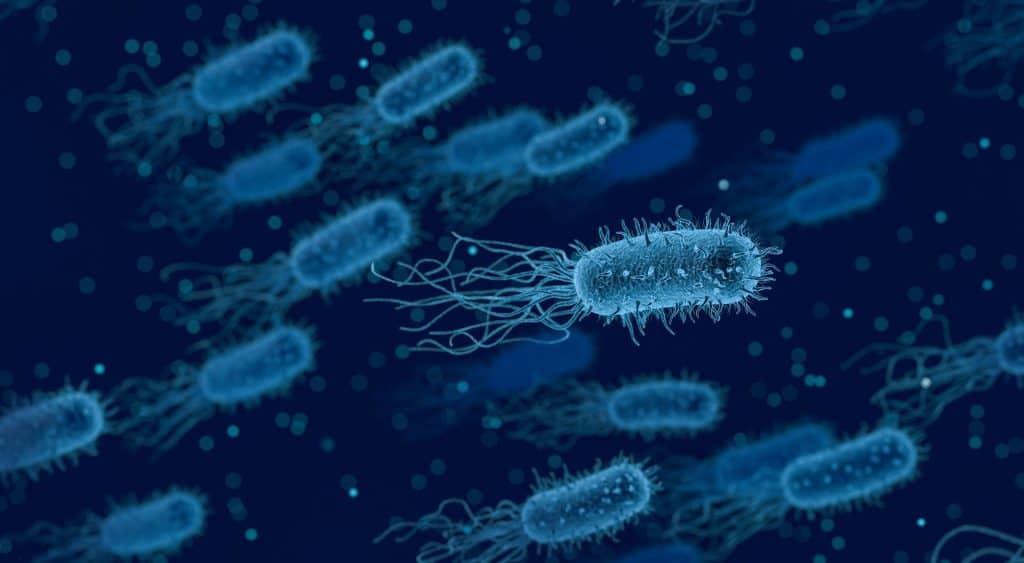
Over the last few years, increasing evidence has mounted for the implication of the gut microbiome in human health and disease. Cancer, multiple sclerosis and some mood disorders have been linked to dysfunctional changes in human gut health. Research efforts continue to investigate the link between this system and disease, and potentially harness the results to develop effective therapeutics.
Introduction
The human gut microbiome is a collection of microorganisms that reside in the gastrointestinal tract. Bacteria and fungi are a few of the many microorganisms which contribute to a system that plays a critical role in human health. In addition to regulating our metabolism, the gut microbiome is also a key player in the development and maintenance of the host immune system.
Changes within this sensitive environment have been studied for a number of years, with increasing evidence supporting the association between gut health and the development of disease states.
The gut forms a barrier composed of a mucus and epithelial layer that serves as an interface between the host internal environment and the outside environment. A disrupted gut barrier increases the permeability to potentially harmful microbes and other by-products which cause an aberrant inflammatory response. The gut microbiota can be disrupted by a number of extrinsic factors including diet, lifestyle and infection in addition to intrinsic factors like genetic profile.
While this could be as mild as inflammation or an allergy response, it can cause an unwarranted immune response which can lead to the development of autoimmune disorders. Studies as recent as 2018 have linked gut microbiota to inflammatory diseases like multiple sclerosis and rheumatoid arthritis.
Disorders such as these correlate with a loss of microbial diversity and the depletion of specific bacteria. Identifying this association is one of the reasons research continues to explore this biological system and better understanding of the functional interactions between the human host and the microbiome. With continued research efforts, it is very likely this could lead to new diagnostic, prognostic and therapeutic capabilities.
Oncology: The toxic side effects of chemotherapy
As described, the gut microbiome plays a huge role in metabolic function within the human body. In addition to processing food and breaking down internal by-products, bacterial enzymes impact the metabolism of diverse pharmaceutical compounds, including chemotherapeutics.
The microbiota in the gut alter the pharmacokinetics of drugs via a number of mechanisms – this can result in changes to the drug’s bioactivity and bioavailability which can significantly impact therapeutic efficacy and mostly cause toxic side effects.
One of the most documented complications of systemic chemotherapy is gastrointestinal toxicity which can cause nausea, vomiting, diarrhoea and constipation.
It has been suggested that “selective and precise targeting of the gut microbiota may alleviate these toxicities”. This could be a huge breakthrough for chaemotherapeutics, as these side effects often result in patients undergoing dose reduction or drug holidays to manage them better. This can negatively impact prognosis and can result in rapid cancer progression and mortality.
The toxic side effects that arise during chemotherapy could be linked with microbial changes that arise during and following chemotherapy.. A study back in 2014 found that during a five-day high-dose chemotherapy regimen, the team observed a significant reduction in the microbial richness and diversity of the GI tract. The high-dose chemotherapy causes a marked decrease in overall microbial diversity and shifts the microbial community structure.
The richness and diversity of the GI tract is a critical part of a healthy gut microbiome which significantly impacts how it metabolises substances. However, in certain health conditions, gut microbiota diversity can be improved and managed effectively by diet.
Therefore, it has been suggested that “dietary changes may lessen injury to normal tissues and alleviate GI toxicity associated with chemotherapy”. Although preclinical findings suggest a beneficial role in the use of nutritional supplements with chemotherapy, more research is required to develop effective adjuvants during anticancer therapy.
Neurology: Neurodegenerative diseases and mood disorders
In addition to inflammatory disorders, increasing evidence is showing that dynamic changes in gut microbiota (collection of microorganisms) can alter brain physiology and behaviour. For a long time, changes to cognition and mood alterations have been thought to be exclusively regulated by the central nervous system which itself is susceptible to a host of extrinsic factors like hormonal fluctuations.
However, it now appears that alterations in the gut microenvironment regulate not only the synthesis of metabolites but neurotransmitters like serotonin, gamma-aminobutyric acid and acetylcholine. Disruption to serotonin levels especially is linked to a host of mood disorders like anxiety and depression.
The association between the gut microbiota and mood disorders is supported by a number of animal models. A recent publication highlighted how germ-free and antibiotic rodent models have shown that microbiota exposure can induce depression, anxiety decreases in social communication and memory deterioration. In a 2016 study, patients diagnosed with mental conditions, including depression, demonstrated gut microbiome dysbiosis – this refers to a condition in which the gut microbiota become imbalanced.
The study of gut microbiota affecting mood disorders remains a relatively new research topic in the grand scale of the field. A key point raised in 2018 article emphasised more studies are needed to ascertain the benefits of using probiotic interventions in promoting stable brain processing
Recently, gut health has drawn increasing attention with regards to its implication in neurodegenerative disorders like multiple sclerosis. Alterations in the microbiome have been found in MS patients and common inflammatory demyelinating disease models.
In the animal disease models, the immunological changes are characterised by an increased inflammatory response. However, it has been demonstrated that important bacteria like Bifidobacterium and Lactobacillus can reduce the severity of symptoms. Other studies also validated that probiotic treatment can achieve a similar effect. This is a huge step forward in both understanding the mechanism of MS from a gut health perspective and for future therapeutic developments, especially as the response to MS treatment varies greatly between patients.
Charlotte Di Salvo, Former Editor & Chief Medical Writer
PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts

Molecular Biology & Biotechnology
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.

Drug Discovery Biology
Unlocking GPCR Mysteries: How Surface Plasmon Resonance Fragment Screening Revolutionizes Drug Discovery for Membrane Proteins
Surface plasmon resonance has emerged as a cornerstone of fragment-based drug discovery, particularly for GPCRs.
Read More Articles
Designing Better Sugar Stoppers: Engineering Selective α-Glucosidase Inhibitors via Fragment-Based Dynamic Chemistry
One of the most pressing challenges in anti-diabetic therapy is reducing the unpleasant and often debilitating gastrointestinal side effects that accompany α-amylase inhibition.