Rare cancers are notoriously difficult to study and present a critical problem in clinical research. Innovations to clinical trial design and patient recruitment are some of the many changes in the field to optimise the outcome of clinical trials for rare cancer types. The current focus is to obtain more reliable and valid data on disease progression and therapeutic treatment for patients of rare cancers.
As of 2019, rare diseases affect approximately 60 million people across the US and Europe. In the UK, one in five patients with cancer will be diagnosed with a rare cancer. Unfortunately, rare diseases often lack safe, therapeutic treatment as a result of barriers in clinical research. In comparison to non-rare diseases, clinical trials studying rare diseases typically struggle to meet patient recruitment targets, which results in trials lacking clinical validity and often early termination. Furthermore, despite innovations in cancer research, therapeutic development for rare cancer types fails to progress. It is critical to create strategies to optimise clinical research for rare diseases including cancer, which are often chronic and life-threatening.
Challenges of therapeutic development for rare disease
There are a multitude of challenges in clinical and scientific research for rare diseases, cancer especially. According to the National Cancer Institute, a cancer type is classified as rare if it occurs in fewer than 15 out of 100,000 people. Stomach (gastric) cancer is an example of rare cancer. Due to a subtle onset, the disease has often progressed upon diagnosis resulting in poor prognosis for patients. While scientific research understanding the pathology of the disease has seen great advancements, the clinical applications have seen little success in changing prognosis. Survival rates for rare cancer types like gastric cancer continues to be low in comparison with common cancer types like breast or prostate cancer. This suggests that poor outcomes in clinical research are limiting progression in precision medicine, further inferring there are challenges that need be addressed in clinical trials.
Fibrolamellar hepatocellular carcinoma is classified as an ultra-rare cancer type. According to a 2021 review, due to the limited number of studies and absence of standard treatment, treatment decisions for this cancer are often made on case reports. This supports the absence of a sufficient number of validated clinical studies for treatment. Surgery for this rare liver cancer predicts survival from 44 to 68%. Unfortunately, without surgery the prognosis plummets with chances of survival ranging between 2 and 17%. Surgery is not always an option for patients with underlying health conditions or of an older age group. Hence, effective therapeutic treatment needs to be a viable alternative.
These two cancer types emphasise the problem with limited rare disease research. With limited clinical evidence for safe, effective treatment, patients cannot access appropriate treatments. In addition, clinicians often make incorrect diagnoses, and have difficulty finding clinical expertise to support their decision.
Clinical and regulatory challenges
With rare diseases, there is typically a small patient population which presents many issues. A limited patient cohort comprises the validity of randomised controlled trials. Furthermore, the small patient population often means potential subjects are geographically diverse which makes the logistics of clinical operations very difficult. According to Dr. Evangeline Wassmer, Paediatric Neurology Consultant at Birmingham Children’s Hospital, “very rare diseases often don’t have treatment, so any treatment you are using or trying out, you can pretty much only do phase I or phase II studies. It is very hard to get to phase III or even randomised studies because the numbers are just too small”. This factor in particular is a challenge for regulatory procedures. Ethics submission, informed consent and approval often differ across national borders and place additional burden on international trials.
The cost of a rare disease clinical trial can also increase disproportionately to the number of enrolled patients which becomes a burden for already-underfunded trials. There are also many practical issues including ensuring reliable communication among sponsors, adequate monitoring and follow-ups which can create a bias for the outcome of the clinical trial.
Strategies and future challenges
With a small patient population, understanding of the disease in terms of clinical progression can be difficult. Modelling disease progression from natural history data has been suggested in a 2019 review as a solution to be used as a part of clinical trial simulations. The review states that “a robust quantitative understanding of disease progression may be used to define cut-off points for clinical trial enrolment”. However, natural history databases require continuous updates to remain relevant, which can be time consuming and costly.
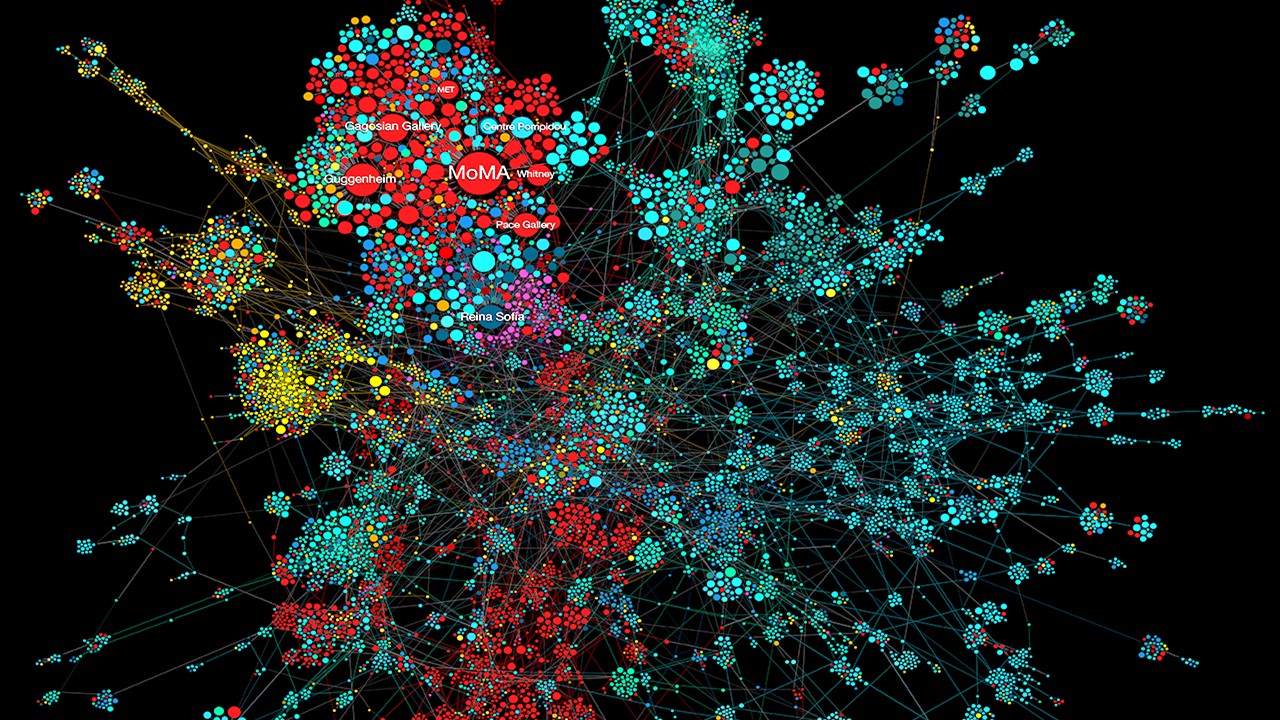
Furthermore, with limited data on rare cancers, attention also needs to be focused on how to make the most of available knowledge. Due to the small number of rare cancer randomised clinical trials, it has been suggested in a European consensus study that other areas of research should also be considered as additional evidence. Examples include preclinical studies, uncontrolled trials, observational studies, and anecdotal cases. The study also proposed that scores be created for the available studies to reduce subjectivity and ensure validity.
Additional comments about the study design, patient enrolment especially, were made explicit in the consensus. “When the enrollment in a study of an adequate number of eligible patients is not feasible, an option is to carry out low-power randomized clinical trials. In this way, the principle of internal controls is met, and the biases from uncontrolled studies are avoided. However, the risk of missing a moderate/small treatment effect is high, and the low power of the trial should be acknowledged in the study protocol.”. Further points were made about the direction for cancer research. It was suggested that biomarkers should be the focus of new drugs, as it may incidentally identify appropriate patient populations that may benefit.
In terms of trial design, the same study encouraged adaptive trials for rare cancer types. Adaptive clinical trials allow parts of the study to be altered while it is ongoing – this is dependent on the data analysis from enrolled patients or other trials. It was emphasised that “rare cancers take special benefit from adaptive trials, because of the difficulty to find patients for clinical studies and the consequently long recruitment timelines. The development of a new drug, all the more in rare cancers, can be easier and faster thanks to adaptive mechanisms, such as, for example, the intensive use of stopping rules”.
Charlotte Di Salvo, Lead Medical Writer
PharmaFeatures
Subscribe
to get our
LATEST NEWS
Related Posts

Clinical Operations
Beyond the Intervention: Deconstructing the Science of Healthcare Improvement
Improvement science is not a discipline in search of purity. It is a field forged in the crucible of complexity.

Clinical Operations
Cracking the Code of Clinical Change: Theories as Tools in Transforming Patient Care
Improving patient care requires more than good intentions; it demands a disciplined, theory-driven approach that connects innovation to implementation and evidence to action.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.
Designing Better Sugar Stoppers: Engineering Selective α-Glucosidase Inhibitors via Fragment-Based Dynamic Chemistry
One of the most pressing challenges in anti-diabetic therapy is reducing the unpleasant and often debilitating gastrointestinal side effects that accompany α-amylase inhibition.