Read on for PharmaFEATURES’ end-of-month roundup highlights in drug approvals for January 2022. The article covers the most innovative products to be approved for tackling unmet needs throughout the industry.
Vabysmo
31 January 2022
Roche announced the approval of faricimab-svoa, marketed as Vabysmo, for the treatment of neovascular age-related macular degeneration (nAMD) and diabetic macular edema (DME). This makes the treatment the first bispecific antibody to be approved for any eye conditions. The treatment functions through the inhibition of two pathways that contribute to the disease: the neutralization of angiopoietin-2 and vascular endothelial growth factor-A. These pathways destabilize ocular vasculature and also lead to the development of new, leaky blood vessels – increasing inflammation. Untreated nAMD and DME can lead to severe vision loss – the two conditions affect over 40 million people worldwide. The therapy only needs to be administered once every month, or two months depending on patient needs, and large improvements can be seen in the first year after treatment. The approval follows positive results from four large phase III trials, with even an editorial on the Lancet covering the one-year results from the studies. The approval of Vabysmo marks an important step forward in ophthalmology and the treatment of some of the leading causes of vision loss in advanced age. Its long-lasting action and effect on two separate mechanisms of disease at once marks Roche’s commitment to Ophthalmology, as noted by their Chief Medical Officer, Levi Garraway:
“Vabysmo provides a new approach to treating vision-threatening retinal conditions through a mechanism of action that targets two pathways simultaneously. This is our second FDA approval in ophthalmology in recent months, underscoring our commitment to people living with retinal conditions.”
Kimmtrak
26 January 2022
The approval of tebentafusp-tebn, marketed as Kimmtrak, was announced by Immunocore in late January, providing further hope for patients living with uveal melanoma. The treatment targets cancers that occur in the iris, the ciliary body or the choroid of the eye – which are parts of the uvea. While uveal melanomas have high (>70%) 5-year survival rates when detected before distant metastases, approximately 50% of patients will show metastases within 15 years. The survival rate for the latter group tends to be 4-5 months. Aside from radiation therapy, enucleation – the removal of the affected eye – is the other most common treatment modality. Novel therapeutics for the area can therefore provide large improvements in quality of life. Kimmtrak is the first T-cell receptor bispecific immunotherapy to be FDA-approved, and also the first treatment for metastatic uveal melanoma which cannot be resected. Median overall survival for the group that received the treatment in trials was 22 months – a massive life-extending improvement compared to the lack of options prior to the approval. The toxicity profile of the product is similar to other immunotherapies. Immunocore also aims to launch a program to improve access to the treatment. John Kirkwood from the UPMC Hillman Cancer Center noted the significance of the novel treatment:
“Uveal melanoma is a devastating disease that has historically resulted in death within a year of metastasis for our patients. The approval of KIMMTRAK (tebentafusp-tebn) represents a major paradigm shift in the treatment of metastatic uveal melanoma, and for the first time offers hope to those with this aggressive form of cancer.”
Cibinqo
14 January 2022
Pfizer announced the launch of Abrocitinib, marketed as Cibinqo, a Janus kinase 1 inhibitor for the treatment of moderate and severe atopic dermatitis. Atopic dermatitis is one of the most common forms of eczema, a form of inflammatory skin disease, with millions affected worldwide. Cibinqo aims to target the demographics which have failed to respond to other treatment options. Like other Janus Kinase inhibitors, the treatment works by reducing inflammation – which is what causes the symptoms. The approval follows the conclusion of five clinical trials investigating the product, involving over 1,600 patients. Common adverse events included nasopharyngitis (8-12%), nausea and (6-15%) and headache (6-8%), marking Cibinqo as a relatively safe option for treatment-resistant atopic dermatitis. As a Janus Kinase inhibitor, Cibinqo is also subject to other contraindications – the drug class is known to raise the risk of blood pressure, cardiovascular adverse events and blood cancers. However, the approval is indicative of the new avenues with which Janus Kinase inhibitors allow us to intervene in immune-related disorders, and further developments in the field are expected.
QUVIVIQ
10 January 2022
Daridorexant, marketed as QUVIVIQ, was approved by the Food and Drug Administration in January for the treatment of insomnia. QUVIVIQ was developed by Idorsia, which demonstrated significant improvements in sleep onset, maintenance and total sleep duration over placebo treatments in Phase III trials. The approval marks Idorsia’s first successful drug launch. Daridorexant – unlike current treatments which tend to sedate the brain – is a dual orexin receptor antagonist. This prevents orexins, which are neuropeptides that maintain wakefulness, from binding to orexin receptors. QUVIVIQ will also be classified as a controlled substance due to its potential for addiction and abuse. Adverse events noted in the trial of the treatment were generally mild and included headaches in 6-7% of patients and somnolence in 5-6%. These effects may last beyond the duration of sleep caused by Daridorexant, which may make some activities such as driving early in the morning unsafe. Chief Scientific Officer of Idorsia, Martine Clozel, noted the pioneering nature of the treatment and its well-rounded safety profile in a forward-looking statement:
“After more than 20 years of research and a progressive understanding of the role of orexin in sleep-wake balance and of the potential of orexin receptor antagonism, we designed daridorexant to help address several issues people with insomnia face. Daridorexant properties include a potent inhibition of both orexin receptors, a rapid absorption for sleep onset, and a pharmacokinetic profile such that around 80% of daridorexant has been eliminated after a night of sleep to help minimize residual effects.”
Recorlev
30 December 2021
Levoketoconazole, marketed as Recorlev, received an approval from the Food and Drug Administration at the end of December for the treatment of Cushing’s Syndrome in adults. The therapy was developed by Xeris Pharmaceuticals, a company that specializes in developing therapies for endocrine disorders. The approval is Xeris’ first foray into cortisol-related disorders; Cushing’s Syndrome is a rare disease characterized by an excess of cortisol in the body. The disease often results from a history of chronic steroid use and results in the accumulation of excess fat on the abdominal area and the shoulders. However, endogenous Cushing’s Syndrome is often caused by tumours in the adrenal or pituitary glands; treatments to relieve symptoms when the tumour cannot be completely eliminated have been lacking, and Recorlev is expected to change that. Professor of Medicine and Neurological Surgery and Director of the Pituitary Center at Oregon Health Sciences University, Maria Fleseriu, highlighted the importance of the approval for the disease moving forward:
“Levoketoconazole (Recorlev) is an important and welcome new therapeutic option for clinicians to help manage patients with endogenous Cushing’s syndrome, a severe, potentially life-threatening rare disease, if not appropriately treated, with multisystem signs and symptoms.”
Nick Zoukas, Former Editor, PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts

Medicinal Chemistry & Pharmacology
Aerogel Pharmaceutics Reimagined: How Chitosan-Based Aerogels and Hybrid Computational Models Are Reshaping Nasal Drug Delivery Systems
Simulating with precision and formulating with insight, the future of pharmacology becomes not just predictive but programmable, one cell at a time.

Medicinal Chemistry & Pharmacology
Coprocessed for Compression: Reengineering Metformin Hydrochloride with Hydroxypropyl Cellulose via Coprecipitation for Direct Compression Enhancement
In manufacturing, minimizing granulation lines, drying tunnels, and multiple milling stages reduces equipment costs, process footprint, and energy consumption.

Medicinal Chemistry & Pharmacology
Decoding Molecular Libraries: Error-Resilient Sequencing Analysis and Multidimensional Pattern Recognition
tagFinder exemplifies the convergence of computational innovation and chemical biology, offering a robust framework to navigate the complexities of DNA-encoded science
Read More Articles
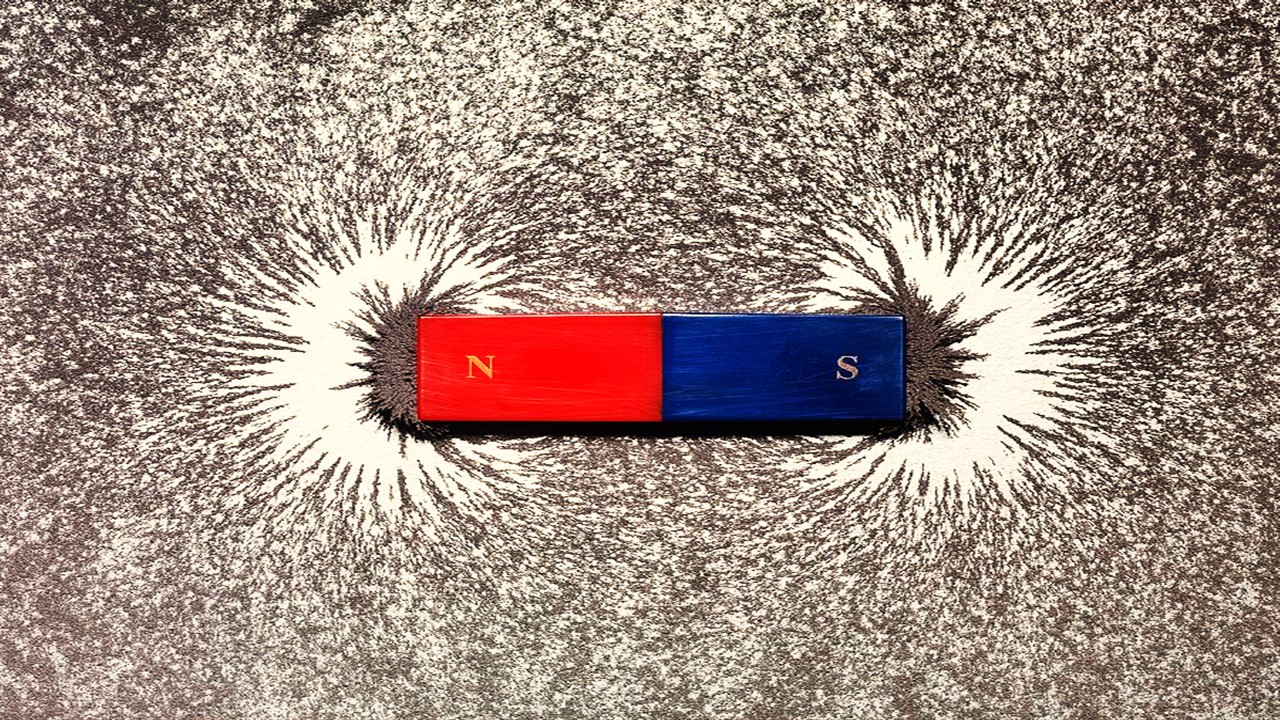
Magnetic Nanoengineering: Overcoming Biological Variability and Enhancing Therapeutic Precision
The future of nanomedicine lies in harmonizing precision, accessibility, and ecological responsibility, ushering in an era where therapies are tailored to individual biological landscapes.
Trials, Triumphs, and Trials Ahead: Navigating the Landscape of Randomized Controlled Trials in Artificial Intelligence-Driven Healthcare
The adoption of artificial intelligence in clinical practice has prompted a surge in randomized controlled trials, highlighting a balance of enthusiasm and prudence.
Illuminating the Dark Genome: Uncharted Frontiers in Therapeutic Discovery
The dark genome is not a biological void but a frontier awaiting illumination.