
High relapse rates remain a critical problem for patients with schizophrenia and their symptom management. Daily medication regimens and unwanted side effects are a few of the causes for poor treatment adherence, which remains a challenge in the field. The recent FDA approval for J&J’s latest schizophrenia drug, promises more long-term symptom alleviation with limited clinical intervention.
Schizophrenia accounts for around 30% of all spending on adult mental health in the NHS. Unfortunately, for many disorders like schizophrenia, the success of drug combinations can vary in clinical efficacy across the patient population, and are typically only a short-term solution – hence why therapy is often used in conjunction.
The complexity of brain pathology is another reason why drug development for psychiatric conditions often fails at the clinical stage. Understanding the neural mechanisms for conditions like depression is key for determining target identification and validation.
Schizophrenia for example, is a complex disorder involving the dysregulation of multiple pathways in its pathophysiology. Even today, the pathophysiology of this psychiatric condition is yet to be defined due to the complex interaction between multiple networks and neurotransmitter systems, resulting in a wide range of clinical manifestations.
Due to this issue, it is very hard for pharma companies to progress from the R&D stage to preclinical research – if the pathophysiology cannot be fully understood, then it is difficult to model the disease state in an animal.
The goal of treatment during schizophrenic episodes, such as hallucinations and thought disorder, is to reduce the severity of psychosis and associated symptoms as fast as possible. This creates time for the patient and physicians to formulate short- and long-term treatment plans to prevent relapse or slow disease progression.
Drugs such as olanzapine are often used in acute episodes and can be effective, however side effects like depression, insomnia and weight gain, often deter patients from completing treatment. Up to 50% of patients with schizophrenia do not adhere to treatment in the short-term, and approximately 75% experience recurrent relapse. Relapses also arise due to missed doses which can be a frequent occurrence for patients with schizophrenia.
Poor treatment adherence, complex pathology, and variable treatment efficacy, have challenged drug development for schizophrenia – the latest news however, demonstrates significant progress being made in the right direction.
Latest breakthrough: J&J
On Wednesday, September 1 2021, Johnson and Johnson (J&J) received approval for the long-acting atypical antipsychotic Invega Hafyera (6-month paliperidone palmitate) – the first-and-only twice-yearly injectable for the treatment of schizophrenia in adults.
The FDA approval was achieved based on the results of a 12-month, randomised, double-blind phase 3 global study. According to a J&J press release, the results showed that “92.5% of patients treated with INVEGA HAFYERA and 95% treated with INVEGA TRINZA were relapse-free at 12 months”.
The drug is administered by a healthcare provider in the upper buttocks area every six months, resulting in continuous treatment and symptom control for that period.
The long-acting injectable offers a number of advantages over the oral medication, including relief from remembering a medication regimen, lower discontinuation rates, and sustained treatment over longer periods. It is hoped that this longer-acting treatment will support patients in maintaining their prescriptions and reduce the chance of relapse.
The safety profile was consistent with previous studies of J&J’s other injectable schizophrenia treatment, Invega Sustenna and Invega Trinza. The most common adverse reactions (≥5%) were upper respiratory tract infection (12%), injection site reaction (11%), weight increase (9%), headache (7%), and parkinsonism (5%).
The data from the phase 3 clinical trial supports this, demonstrating “compelling evidence that 6-month paliperidone palmitate offers longer-term symptom control with the fewest doses per year, which may support greater patient adherence”.
It has been raised in the media that doctors may be concerned with administering such large doses to patients, before assessment of their reaction to the drug. Therefore, it has been advised by J&J, that patients will be stabilised using a shorter-acting version before switching over to the twice-yearly shots.
Long-acting injectables
Long-acting injectables allow for the slow release of medicine into the bloodstream, and a number of antipsychotic drugs are administered in this way. Risperidone, Aripiprazole, and Paliperidone are a few examples which are prescribed to schizophrenia patients.
In addition to the risk of forgetting oral medication, patients with schizophrenia can intentionally avoid a medication regimen due to voices in their head persuading them to avoid it, or denial they are mentally ill. Long-acting drugs take away this risk of poor adherence, because doctors can keep track of a patient’s treatment as they are personally administering the shots.
In comparison to J&J’s 6-month paliperidone palmitate, long-acting injectables such as risperidone are administered from every two to 12 weeks. Paliperidone is the major active metabolite of risperidone and has a pharmacological profile almost identical to risperidone which is already approved for the treatment of schizophrenia and bipolar mania.
Of course there are some limitations with long-acting injectables, the obvious being the organisation of travel required for clinic visits and some soreness during/after each shot. However, the benefits of long-acting injectables appear to outweigh the risk when compared with oral medication.
The FDA approval for 6-month paliperidone palmitate is hugely important for patients with schizophrenia, for whom oral treatment regimens were tedious and the symptom control was limited in the long-term. It enables patients to manage their symptoms better in a way which does not disrupt their daily life and see more sustainable results.
Charlotte Di Salvo, Lead Medical Writer
PharmaFeatures
Subscribe
to get our
LATEST NEWS
Related Posts

Drug Discovery Biology
Proteolytic Rewriting: Engineering Controlled Absence of Pathogenic Protein Persistence
Targeted protein degradation transforms drug therapy by engineering the cellular machinery to erase, rather than merely inhibit, pathogenic proteins.

Drug Discovery Biology
Open Nucleotides: Grant-Driven Infrastructure for Equitable mRNA Vaccine Manufacturing
By developing accessible cap analogs and RNA raw materials, Hongene Biotech, guided by David Butler’s expertise in nucleotide chemistry and supported by the Gates Foundation, is reshaping the molecular infrastructure that underpins global mRNA vaccine equity.
Drug Discovery Biology
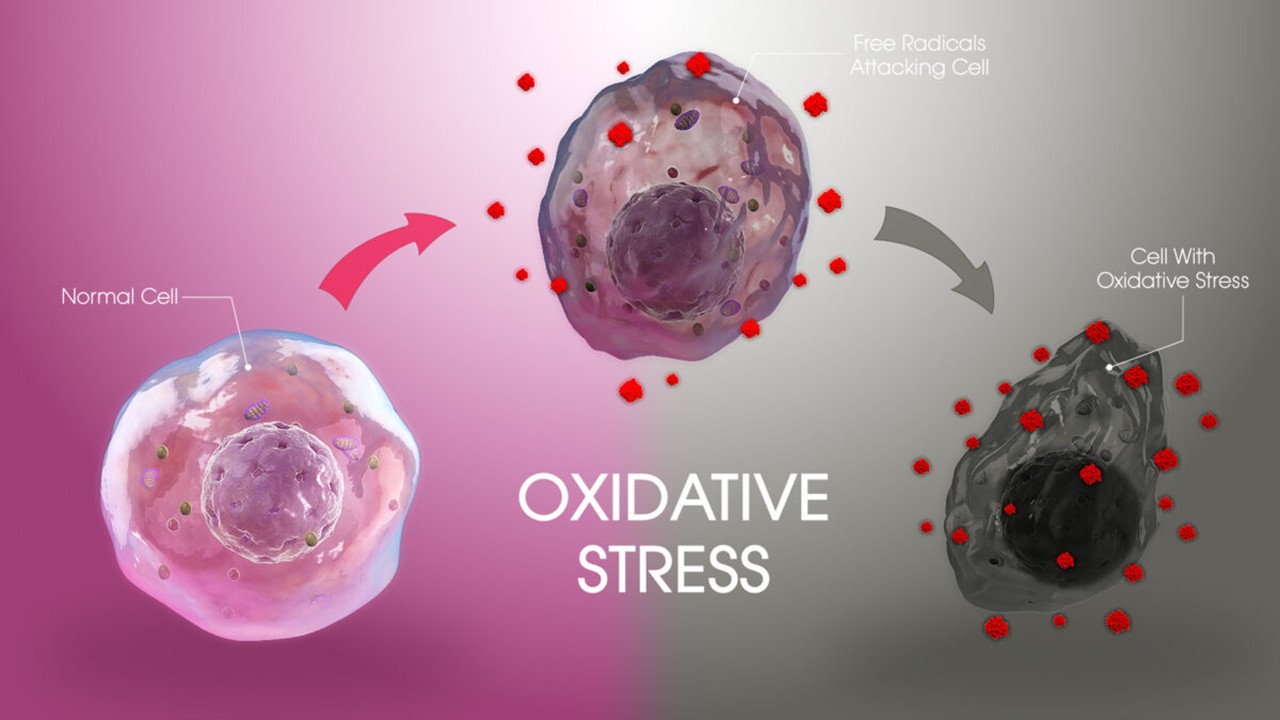
Redox Messengers: How Endogenous Gasotransmitters Rewire Vascular Biology to Resist Age-Driven Oxidative Stress
Gasotransmitters provide a biologically sophisticated means of counteracting age-related oxidative stress and preserving vascular resilience.
Drug Discovery Biology
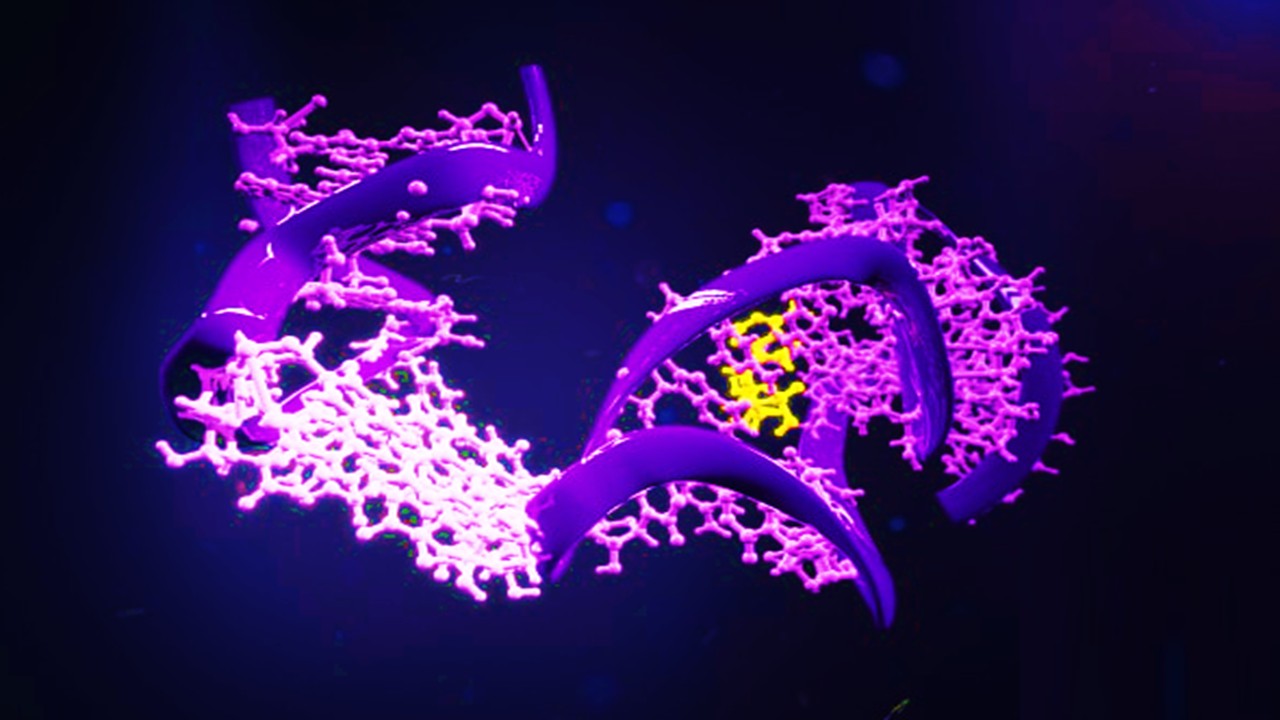
Aptamer Signal Dynamics: Engineering Nucleic Acid Recognition Systems for High-Fidelity, Multi-Modal Biosensing
Aptamers redefine biosensing by pairing programmable molecular recognition with versatile transduction strategies capable of detecting clinically relevant biomarkers with exceptional fidelity.
Read More Articles
Spatial Collapse: Pharmacologic Degradation of PDEδ to Disrupt Oncogenic KRAS Membrane Localization
PDEδ degradation disrupts KRAS membrane localization to collapse oncogenic signaling through spatial pharmacology rather than direct enzymatic inhibition.
Neumedics’ Integrated Innovation Model: Dr. Mark Nelson on Translating Drug Discovery into API Synthesis
Dr. Mark Nelson of Neumedics outlines how integrating medicinal chemistry with scalable API synthesis from the earliest design stages defines the next evolution of pharmaceutical development.
Zentalis Pharmaceuticals’ Clinical Strategy Architecture: Dr. Stalder on Data Foresight and Oncology Execution
Dr. Joseph Stalder of Zentalis Pharmaceuticals examines how predictive data integration and disciplined program governance are redefining the future of late-stage oncology development.
Exelixis Clinical Bioanalysis Leadership, Translational DMPK Craft, and the Kirkovsky Playbook
Senior Director Dr. Leo Kirkovsky brings a rare cross-modality perspective—spanning physical organic chemistry, clinical assay leadership, and ADC bioanalysis—to show how ADME mastery becomes the decision engine that turns complex drug systems into scalable oncology development programs.
Policy Ignition: How Institutional Experiments Become Durable Global Evidence for Pharmaceutical Access
Global pharmaceutical access improves when IP, payment, and real-world evidence systems are engineered as interoperable feedback loops rather than isolated reforms.
Sepsis Shadow: Machine-Learning Risk Mapping for Stroke Patients with Bloodstream Infection
Regularized models like LASSO can identify an interpretable risk signature for stroke patients with bloodstream infection, enabling targeted, physiology-aligned clinical management.







