Over 9 million people worldwide suffer from Type 1 diabetes, which is a huge problem for patients who find it difficult to control their blood glucose levels. A recent study, however, that was released in the journal Nature Biomedical Engineering, gives hope for a longer-lasting and more viable alternative. Researchers have created a cutting-edge screening method employing cellularly barcoded alginates to find new biomaterial formulations that can aid in addressing the limits of existing treatments. The approach was developed by researchers under the direction of Rice University bioengineer Omid Veiseh.
Type 1 Diabetes: In Brief
Type 1 diabetes is a complex disease with a multifactorial etiology involving genetic, environmental, and pharmacologic factors. From a genetic perspective, individuals with a family history of type 1 diabetes are at a higher risk of developing the disease. Multiple genes, such as HLA-DQ and HLA-DR, play a role in susceptibility to type 1 diabetes, but the precise mechanisms by which these genes contribute to disease development are still being investigated.
Environmental factors also play a significant role in triggering type 1 diabetes. Certain viral infections, particularly enteroviruses, have been implicated in the onset of the disease. Additionally, early childhood exposure to cow’s milk and vitamin D deficiency have been associated with an increased risk of developing type 1 diabetes. The interplay between genetic susceptibility and environmental triggers remains an active area of research.
Diagnosis of type 1 diabetes typically involves assessing the presence of clinical signs and symptoms such as polyuria (excessive urination), polydipsia (excessive thirst), weight loss, and fatigue. Laboratory tests including measurement of blood glucose levels and detection of autoantibodies against pancreatic beta cells help confirm the diagnosis. Prognosis for individuals with type 1 diabetes has improved significantly with advancements in insulin therapy and glucose monitoring. However, long-term management of the disease is essential to prevent complications such as cardiovascular disease, kidney damage, and neuropathy.
The Unmet Need in Type 1 Diabetes Treatment
Blood glucose regulation is lost in Type 1 diabetes as a result of the immune system of the body attacking and destroying the pancreatic cells that produce insulin. Making a protective matrix to house islet cells has been the all-important objective of researchers for many years. While avoiding immune system attacks, the matrix ought to let cells get to vital nutrients and oxygen. Developing materials with the best biocompatibility, nevertheless, has proven difficult, mostly because of the drawbacks of traditional screening techniques.
Screening Biomaterials in Live Subjects
Testing on living host organisms has long been the only way to gauge the immunological response to implanted biomaterials. This presents a substantial challenge considering it is impossible to distinguish between the best-performing biomaterials because many biomaterial formulations frequently look indistinguishable. Also, it is impossible to test numerous materials concurrently in a single host.
Veiseh and his team came up with a clever way to get around these problems by finding a way to embed a special “barcode” into each alginate formulation before implanting it. Human umbilical vein endothelial cells (HUVEC) from various donors are paired with each changed biomaterial in this method, which basically uses the HUVEC cells as a barcode. The researchers were able to identify the formulations that contained live cells and identify the best materials. The cells’ genomes were subsequently sequenced, allowing them to determine the specific material-cell pairings.
Revolutionizing Type 1 Diabetes Treatment
Promising findings emerged from the investigation. The scientists encapsulated human insulin-secreting islet cells in one of the alginate formulations to successfully maintain long-term blood sugar control in diabetic rats. Two high-performance materials were coated on catheters, and they exhibited no clogging symptoms. These results show the potential of these biomaterial formulations to offer a more practical and long-lasting method of treating Type 1 diabetes.
Eliminating the Need for Immunosuppression
The need for immunosuppressive medicines is a significant disadvantage of existing islet cell therapies. This method exposes patients to a number of risks, including an elevated risk of cancer and an increased propensity for infections. However, Veiseh and his team’s biomaterial-encapsulation approach has the potential to do away with the requirement for immunosuppression. The possibility of the host immune system identifying foreign materials is increased by encapsulating HUVEC cells inside the biomaterial capsules. Using this approach, a robust experiment that examines immune response to biomaterials in general is possible.
Future Implications and Beyond
Beyond the treatment of Type 1 diabetes, the high-throughput “barcoding” method created in this study has significant ramifications. This method allows for the simultaneous screening of hundreds of biomaterials, greatly lowering the need for live test participants. This development makes a variety of medical applications and device designs possible.
The search for of better biomaterials is further aided by partnerships between bioengineers and specialists in DNA sequencing, such Dr. José Oberholzer and David Zhang. Durable implanted cell therapies can now behave as live drug factories, altering the way chronic diseases are treated.
This ground-breaking study makes it more practical and economical to translate findings into clinically useful treatments, giving millions of people with Type 1 diabetes and other diseases hope. Innovative screening methods and cutting-edge biomaterials have the potential to revolutionize the field of biomedical engineering and enhance the quality of life for patients everywhere.
Study DOI: 10.1038/s41551-023-01016-2
Subscribe
to get our
LATEST NEWS
Related Posts

Chronic & Debilitating Diseases
Renopathology Tipping Point: Deciphering the Molecular Code of Stage 2 Chronic Kidney Disease
The molecular events of Stage 2 CKD, from inflammation to lipid metabolism, offer insights for diagnosis and treatment.
Chronic & Debilitating Diseases
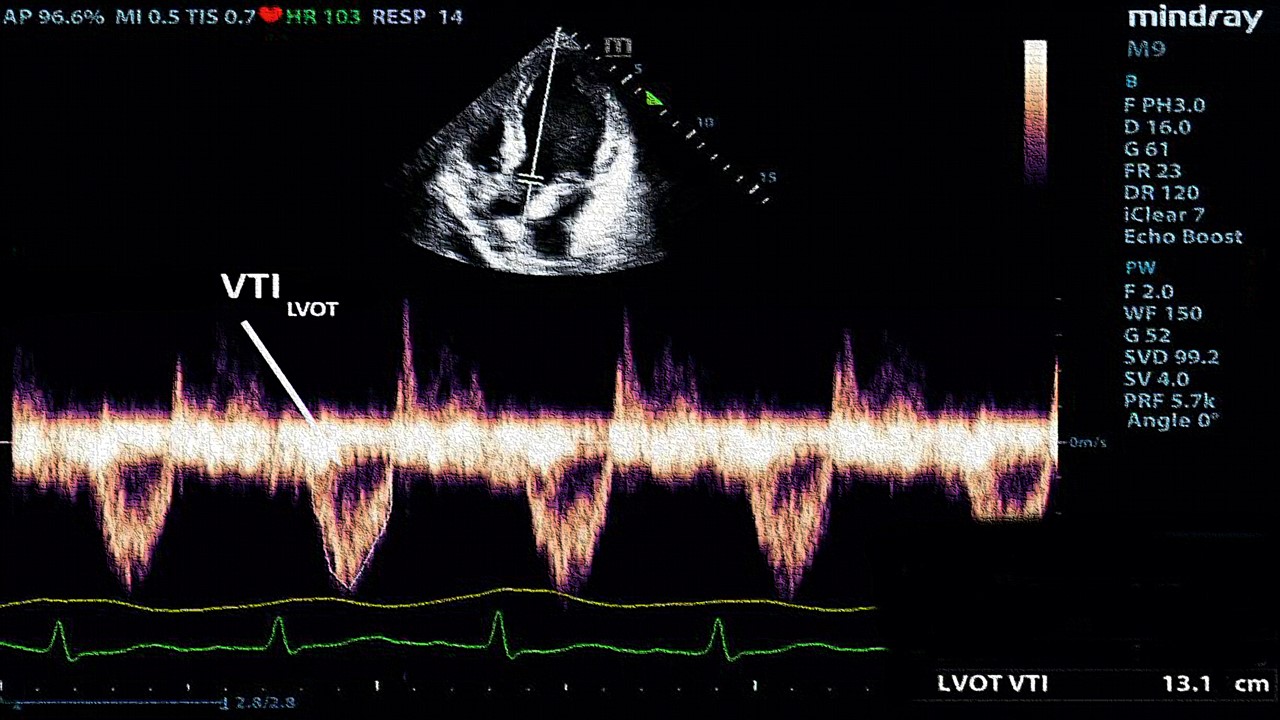
A New Lens on Shock: Hemodynamic Insights Through Critical Care Ultrasound
CCU has transformed the hemodynamic assessment of shock, delivering a reliable, reproducible, and non-invasive tool for ICU clinicians.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.
Designing Better Sugar Stoppers: Engineering Selective α-Glucosidase Inhibitors via Fragment-Based Dynamic Chemistry
One of the most pressing challenges in anti-diabetic therapy is reducing the unpleasant and often debilitating gastrointestinal side effects that accompany α-amylase inhibition.