In the early days of cancer therapeutics, cytotoxic molecules were deployed across the body in an indiscriminate sweep of cellular destruction. These agents, while effective, brought an inevitable and unfortunate consequence: damage to healthy tissue. The collateral damage that accompanied such treatments often undermined their efficacy, as the toxicity to normal cells limited the dosage patients could safely receive. For years, the challenge of how to deliver potent anticancer agents specifically to malignant cells without harming normal ones seemed almost insurmountable.
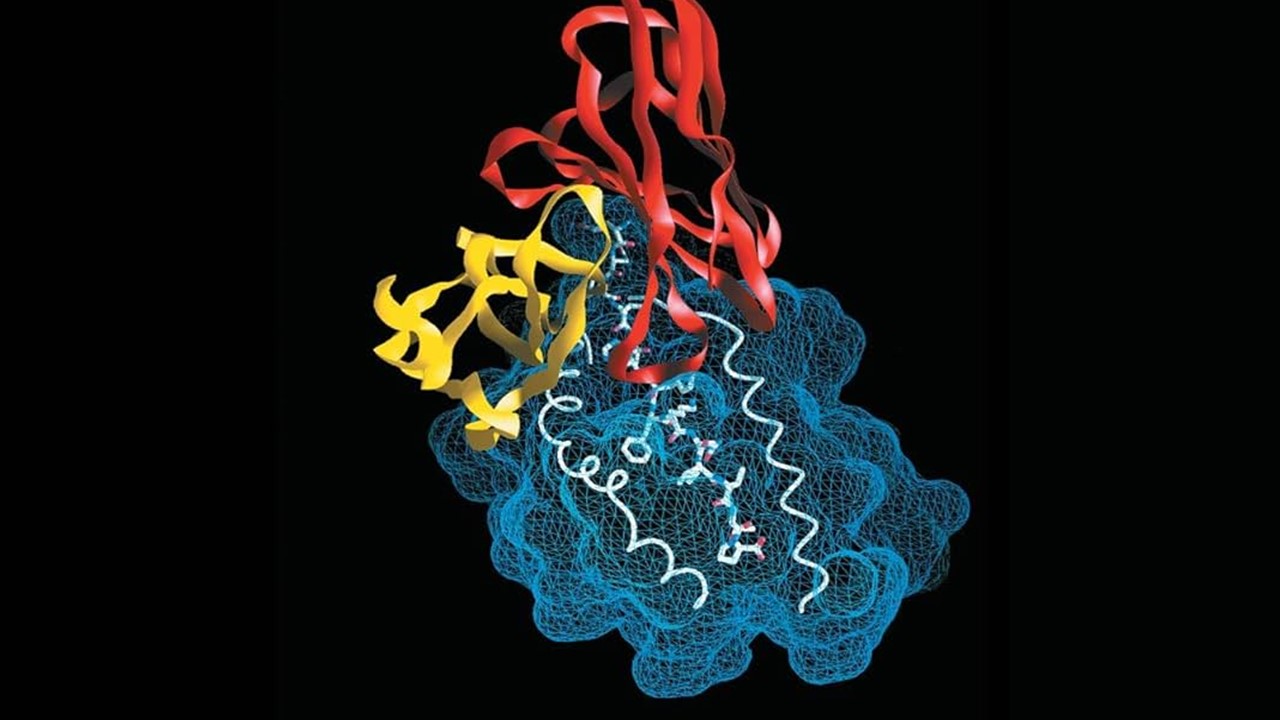
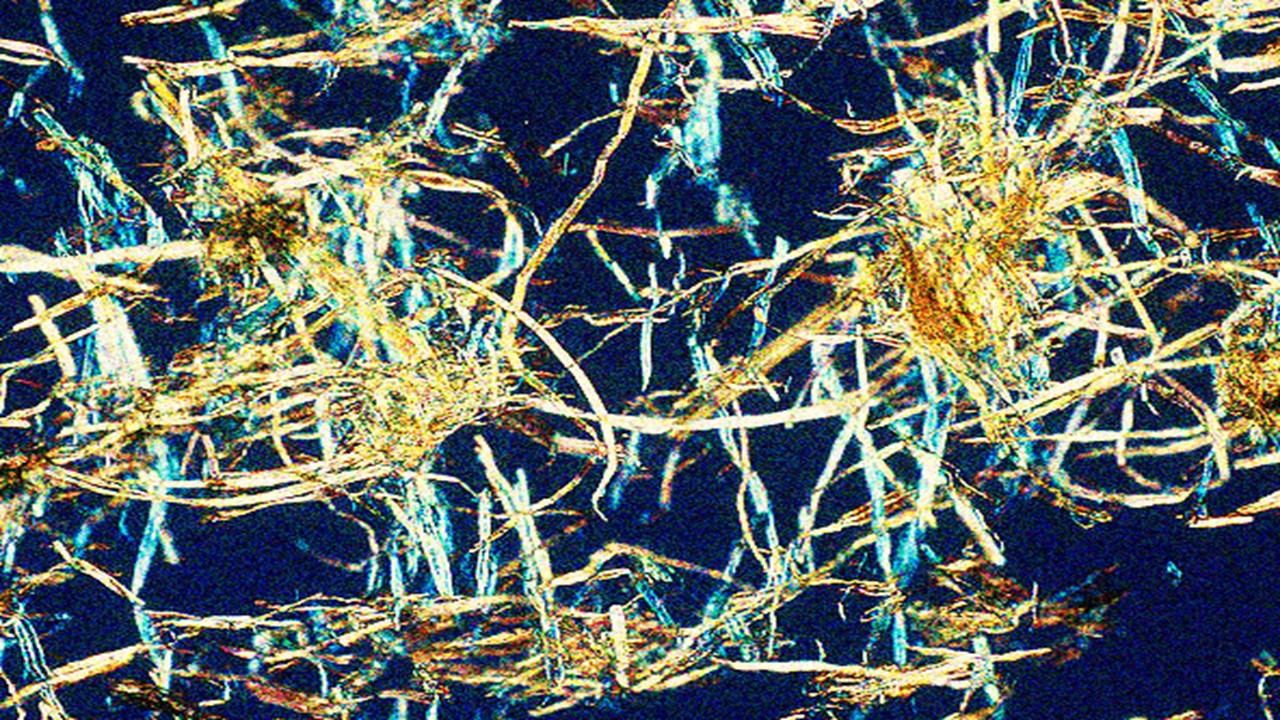
Enter the era of nanocarrier drug delivery, a method designed to focus the power of pharmacology on precision. Liposomes, artificial phospholipid vesicles, have risen to the forefront as one of the most studied and promising nanocarriers. These vesicles, typically ranging from 50 to 1,000 nanometers in size, can encapsulate a variety of drugs, providing a method to alter drug distribution dynamics and concentrate the therapeutic agent exactly where it is needed. This breakthrough technology has opened doors to simplifying drug administration, reducing the required dose, and potentially lowering treatment costs—all while maintaining or even enhancing therapeutic efficacy.
However, liposomes are not without their own limitations. Despite 30 years of intensive research, current formulations cannot selectively target cancer cells at the molecular level. The evolution of liposomes, from rapid clearance to longer-circulating versions, has been a slow but significant journey that has profoundly impacted drug discovery and delivery, marking the transition from traditional drug discovery methods to modern, highly targeted approaches.
The Evolution of Liposomal Drug Delivery
In the earliest iterations, liposomes faced a significant obstacle: rapid clearance by the body’s reticuloendothelial system (RES). These early liposomes were essentially engulfed by macrophages and sequestered in organs like the liver and spleen, thus reducing their ability to reach target sites, such as tumors. It wasn’t until scientists began to investigate the enhanced permeability and retention (EPR) effect—a phenomenon where liposomes accumulate more readily in areas with leaky vasculature, such as tumor sites—that the true potential of these carriers began to emerge.
This discovery catalyzed the development of more stable, longer-circulating liposomes. By incorporating polyethyleneglycol (PEG) lipid conjugates, like mPEG-DSPE, into the bilayer membrane, researchers significantly extended the blood circulation time of liposomes. These “PEGylated” liposomes accumulated in tumors by exploiting the EPR effect, wherein tumors’ abnormal, porous blood vessels allowed easier passage of macromolecules, leading to their retention within the tumor mass.
However, even this approach had limitations. Liposomes, once internalized by the tumor cells, faced another obstacle: the harsh acidic environment and enzyme activity within the lysosomal compartments, which led to the degradation of many sensitive drugs. This was especially critical for certain drug types, such as nucleic acids and peptide-based therapies, where enzymatic breakdown would drastically reduce therapeutic efficacy.
From Passive to Active Targeting: The Leap Forward
As liposome research advanced, attention shifted to improving the intracellular delivery of drugs. The next generation of liposomes sought to address the limitations of passive targeting. One promising approach involved the attachment of molecular ligands to the liposome surface, enabling them to recognize and bind to specific receptors on target cells, such as cancer cells. This “active targeting” method aimed to increase the intracellular concentration of drugs in tumor cells, thus enhancing their therapeutic potential. Despite this significant improvement, liposomes faced yet another challenge—their inability to efficiently release the drug once inside the target cells.
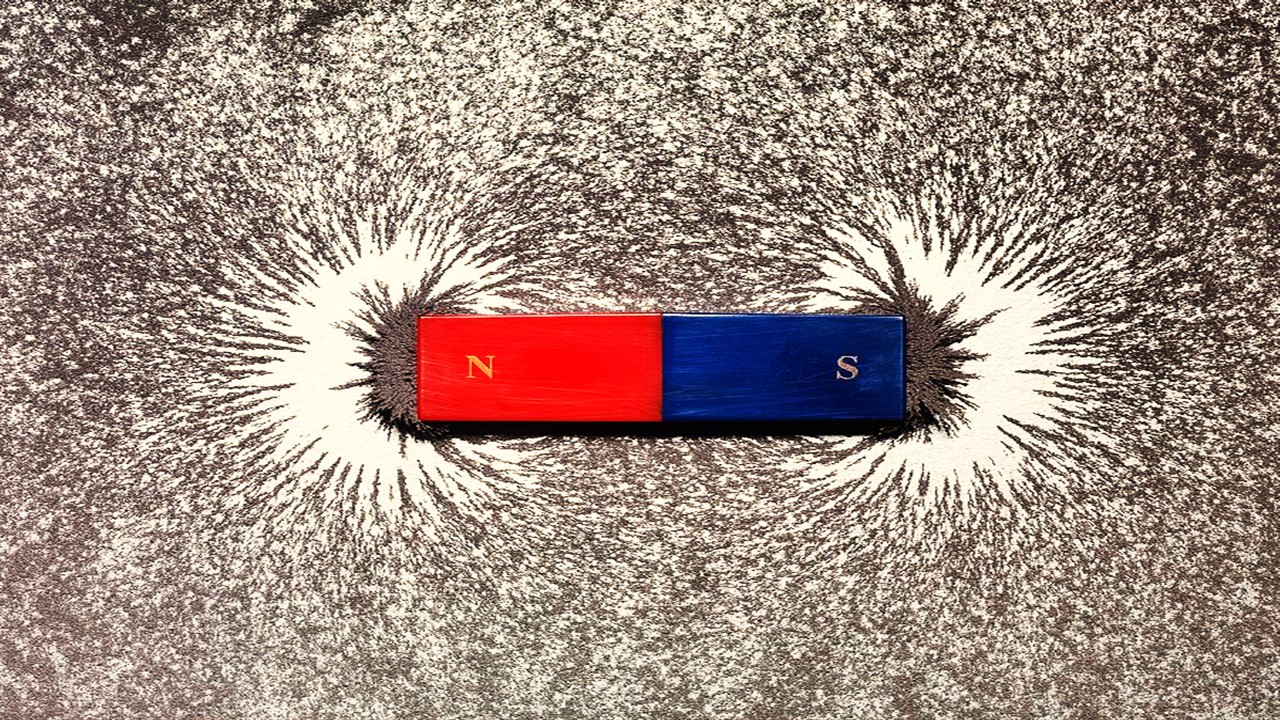
A novel solution emerged in the form of stimuli-sensitive nanocarriers. These carriers, capable of responding to specific internal or external stimuli such as pH changes, temperature fluctuations, or magnetic fields, represented a paradigm shift in liposome technology. These “smart” nanocarriers could protect their cargo until reaching the target tissue, where an external cue would trigger the release of the drug directly into the tumor cells. This fine-tuned mechanism further pushed the envelope of drug discovery, taking scientists closer to the holy grail of site-specific drug delivery.
Overcoming the Barriers to Drug Delivery
The journey from traditional to modern drug discovery techniques is punctuated by an ongoing battle against the body’s natural defense mechanisms. Liposomes have evolved over decades to evade these defenses, yet their role as passive carriers left much to be desired. A significant challenge remained in designing liposomes that could maintain their structure long enough to reach the tumor, release their contents in a controlled manner, and avoid premature degradation.
Modifications to the liposomal surface became a critical strategy. In the 1980s, researchers discovered that adding gangliosides, sialic acid derivatives, or hydrophilic polymers like PEG to the surface could create a barrier against plasma proteins and opsonins—components that mark foreign particles for destruction. PEGylation, in particular, emerged as a cornerstone of liposome longevity, with the polymer forming a protective layer that increased circulation time. By increasing the blood residence time of liposomes, PEG allowed drugs to accumulate more effectively in target areas, such as tumors.
Nevertheless, the presence of the PEG coat itself presented a new dilemma. Once liposomes reached their target, the very mechanism that protected them from the immune system also hindered their ability to release the drug. To address this, scientists developed a method to selectively detach the PEG coating under specific conditions, such as the acidic environment of a tumor or endocytic vesicles. This strategy allowed for a more precise release of the encapsulated drug, improving the overall effectiveness of the treatment.
Designing the Perfect Liposomal Drug Carrier
Creating an effective liposomal drug carrier requires more than just controlling circulation time—it involves meticulous attention to drug and lipid composition. The physicochemical properties of the drug itself play a crucial role in determining its suitability for liposomal delivery. For instance, hydrophilic drugs may struggle to penetrate tumor tissue due to their poor membrane permeability, while hydrophobic drugs can destabilize the liposome by integrating too readily into the lipid bilayer. Amphipathic drugs, such as anthracyclines and Vinca alkaloids, have proven to be the most compatible with liposomal carriers, as their release rates can be fine-tuned to maximize stability in the bloodstream and promote drug release at the tumor site.
The composition of the liposome’s lipid bilayer is equally critical. Cholesterol, for example, is often included to stabilize the membrane and prolong circulation times, while high-phase transition lipids enhance the retention of the drug within the liposome. Additionally, the size and surface charge of the liposome must be optimized to avoid rapid clearance by the RES. Smaller liposomes, extruded through filters to achieve diameters less than 200 nm, have demonstrated longer circulation times, and the inclusion of PEG can further protect liposomes from opsonization and clearance.
Limitations and Future Directions
Despite the progress in liposomal drug delivery, passive targeting through the EPR effect remains an imperfect science. Tumor heterogeneity poses a significant challenge—variations in pore size and permeability across different tumors can limit the effectiveness of liposome accumulation. Furthermore, the elevated interstitial pressure within solid tumors often hinders the uniform distribution of nanocarriers, leading to incomplete drug penetration and the potential for drug resistance.
Moving forward, the field is likely to see continued innovation in stimuli-responsive liposomes and other multifunctional nanocarriers. These advancements will build upon decades of research in passive and active targeting, bringing scientists ever closer to the goal of personalized, precision cancer therapy. The shift from traditional drug discovery methods to modern lead discovery strategies, exemplified by the evolution of liposome technology, has already begun to reshape the landscape of pharmacology and oncology.
The future of drug delivery is increasingly reliant on the integration of nanotechnology, biomolecular engineering, and a deeper understanding of tumor biology. As researchers continue to push the boundaries of what is possible, the promise of more effective and less toxic cancer treatments becomes ever more attainable.
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts
Medicinal Chemistry & Pharmacology
Aerogel Pharmaceutics Reimagined: How Chitosan-Based Aerogels and Hybrid Computational Models Are Reshaping Nasal Drug Delivery Systems
Simulating with precision and formulating with insight, the future of pharmacology becomes not just predictive but programmable, one cell at a time.
Medicinal Chemistry & Pharmacology
Coprocessed for Compression: Reengineering Metformin Hydrochloride with Hydroxypropyl Cellulose via Coprecipitation for Direct Compression Enhancement
In manufacturing, minimizing granulation lines, drying tunnels, and multiple milling stages reduces equipment costs, process footprint, and energy consumption.

Medicinal Chemistry & Pharmacology
Decoding Molecular Libraries: Error-Resilient Sequencing Analysis and Multidimensional Pattern Recognition
tagFinder exemplifies the convergence of computational innovation and chemical biology, offering a robust framework to navigate the complexities of DNA-encoded science
Read More Articles
Magnetic Nanoengineering: Overcoming Biological Variability and Enhancing Therapeutic Precision
The future of nanomedicine lies in harmonizing precision, accessibility, and ecological responsibility, ushering in an era where therapies are tailored to individual biological landscapes.
Trials, Triumphs, and Trials Ahead: Navigating the Landscape of Randomized Controlled Trials in Artificial Intelligence-Driven Healthcare
The adoption of artificial intelligence in clinical practice has prompted a surge in randomized controlled trials, highlighting a balance of enthusiasm and prudence.
Illuminating the Dark Genome: Uncharted Frontiers in Therapeutic Discovery
The dark genome is not a biological void but a frontier awaiting illumination.