
- The development of cancer vaccines is an important step towards precision immunotherapy for cancer patients, based on a more personalised approach to specific tumour profiles. Alternative forms of immunotherapies are not always effective across a patient population, with many individuals demonstrating little to no response. Some of the latest advancements show new, innovative approaches to cancer vaccine development, including the utilisation of the mRNA technology used to create the COVID-19 vaccine.
Introduction
Cancer vaccines represent a significant development in onco-immunotherapy. In 2001, the first cancer vaccine was created against the human papilloma virus. This important breakthrough paved the way for the development of the first preventive cervical cancer vaccine – Gardasil.
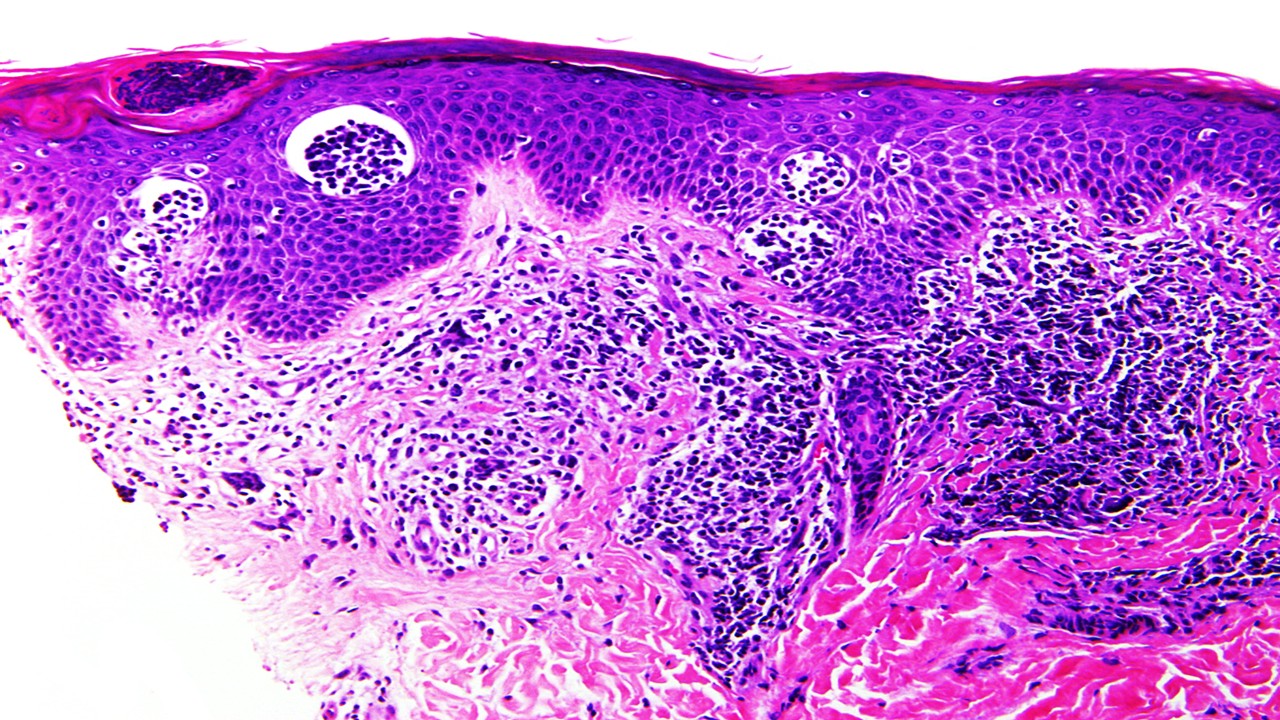
As with conventional immunotherapy, the goal of cancer vaccines is to amplify the tumour-specific T-cell response. Cancer vaccines are categorised into three platforms: cellular, viral vector, or molecular (e.g. DNA). Dendritic cells are a type of antigen-presenting cell whose role resides in consuming and processing – these cells are used to develop cellular vaccines.
The natural mechanism of viruses allows oncolytic viral vector vaccines to replicate within and destroy tumours. Their ability to directly deliver tumour antigens induces tumour-directed immune responses.
Peptide-based DNA cancer vaccines induce tumour-specific responses through the encoding of tumour-associated antigens and immunomodulatory molecules. Peptide-based cancer vaccines are popular because of their low toxicity and low manufacturing cost. In addition, they possess direct functional T-cell epitopes (the region of the antigen recognised by the immune system). DNA vaccines are easy to manufacture and present excellent safety profiles.
The latest advancements
Cancer vaccines are not a new concept in oncology, and have been in clinical use for a number of years. The HPV (human papillomavirus) vaccine helps protect against cancers caused by HPV, including cervical cancer and some head/neck cancers. It is typically offered for girls and boys aged 12 to 13 years old.
More recently however, thanks to technological advancements and the natural progression of science, a number of exciting things are happening in the cancer vaccine arena. The success of the mRNA COVID-19 vaccines has ignited significant interest in this area of science and how it could be useful for developing cancer vaccines.
Adapting COVID-19 vaccine research: mRNA
Moderna, for example, are applying their mRNA technology to create personalised, mRNA-based cancer vaccines. According to their immuno-oncology portfolio, they believe that “the vaccine has the potential to direct the patient’s cells to express selected neoepitopes. In turn, this may help the patient’s immune system better recognize cancer cells as foreign and destroy them.” Neoepitopes are unique tumour-specific antigens, which typically make attractive cancer immunotherapy targets.
Moderna are currently conducting a phase 1 study in order to assess the safety, tolerability, and immunogenicity of mRNA-4157 in subjects with resected solid tumours, and in combination with KEYTRUDA in subjects with unresectable solid tumors. mRNA-4157 is a personalised cancer vaccine, and aims to induce its therapeutic effect in the following way:
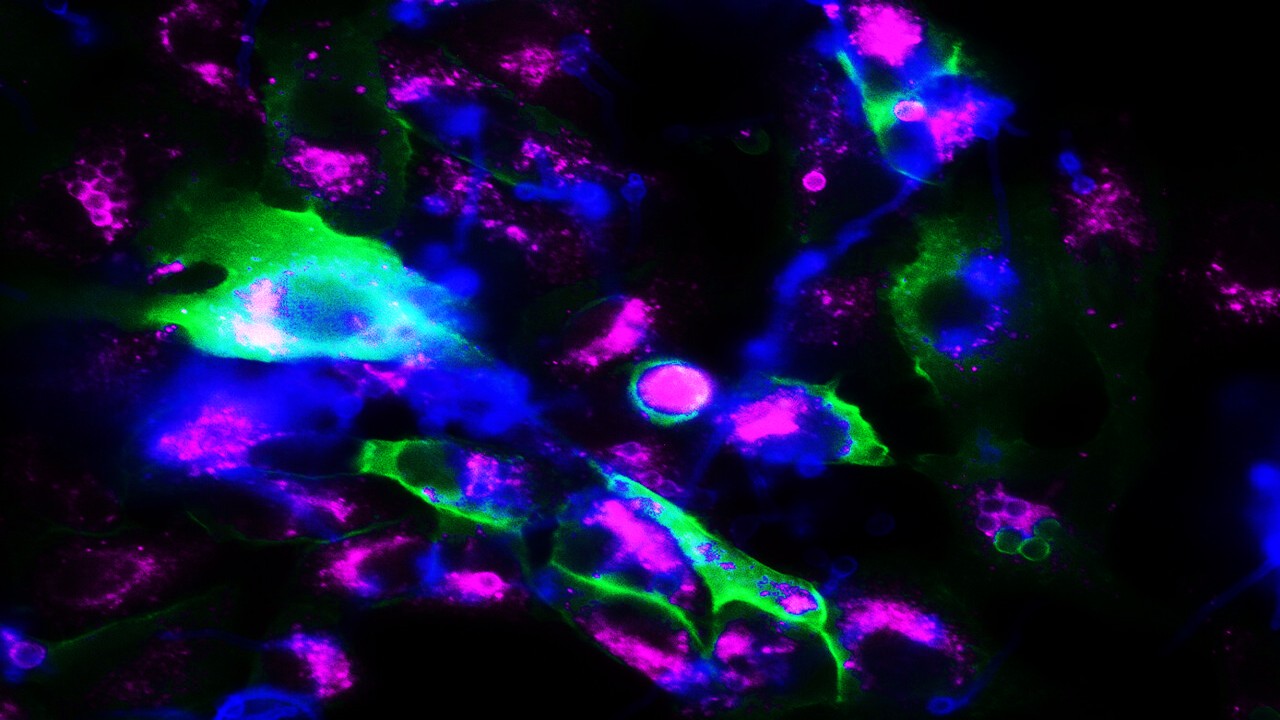
• Upon administration, the mRNA-based PCV mRNA-4157 is taken up and translated by antigen presenting cells (APCs)
• A major histocompatibility complex is used to identify expressed neoepitopes on the surface of the APCs
• This leads to an induction of both cytotoxic T-lymphocyte (CTL)- and memory T-cell-dependent immune responses that specifically target and destroy the patient’s cancer cells that express these neoepitopes
It is hoped that this approach will create a vaccine which is more personalised to the patient’s specific tumour profile, and therefore, more effective. This individualised approach to immunotherapy has been an important target for a number of years, as many patients still respond only partially or not at all to these anti-cancer therapies.
Adapting COVID-19 vaccine research: Oxford-AstraZeneca
Another study, conducted at the Ludwig Institute for Cancer Research, University of Oxford, also demonstrated positive results for cancer vaccines utilising the science for the COVID-19 vaccine. In this case, researchers have built upon the success of the Oxford-AstraZeneca’s research, and designed a two-dose therapeutic cancer vaccine using Oxford’s viral vector vaccine technology.
According to a recent article, the team developed the cancer vaccine with different prime and boost viral vectors, one of which is the same as the vector in the Oxford-AstraZeneca COVID-19 vaccine. In order to create a more precise, personalised treatment, the vaccine was designed to target two MAGE-type proteins that are present on the surface of many types of cancer cells.
So far the data has been promising, demonstrating positive results in recent preclinical studies – “When tested in mouse tumour models, the cancer vaccine increased the levels of anti-tumour T-cells infiltrating the tumours and improved the efficacy of cancer immunotherapy. Compared to immunotherapy alone, the combination with the vaccine showed a greater reduction in tumour size and improved the survival of the mice.”
The vaccine will be evaluated in a phase 1/2a clinical trial later this year, in combination with an anti-PD-1 immunotherapy in 80 patients with non-small lung cancer.
Nouscom – NOUS-209 cancer vaccine
Nouscom is a clinical stage immuno-oncology company which is developing next-generation, off-the-shelf, and personalised cancer vaccines. Nous-209 is Nouscom’s lead candidate, an “off-the-shelf” immunotherapy for Microsatellite Instable High (MSI-H) tumors. The vaccine is based on the neoantigens created by frameshift mutations and are shared across multiple MSI tumors, and are not present in healthy tissues.
The first clinical results from the NOUS-209 phase 1 clinical trial were released very recently and appeared to be relatively positive. According to a news article, it was observed that “in combination with the anti-PD-1 checkpoint inhibitor pembrolizumab, [the vaccine] was shown to be safe, highly immunogenic, and demonstrated promising early signs of clinical efficacy with no dose-limiting toxicities, in the treatment of Microsatellite Instable High (MSI-H) gastric, colorectal and gastro-esophageal junction solid tumors.”
While there is still a way to go in terms of reaching the clinic, these early results are very positive and should also look to address the significant unmet need in the treatment of MSI-H tumours. In addition, it supports the need to continue research into cancer vaccines which could offer more personalised, effective cancer treatment and an option for those who show little response to alternative immunotherapies.
Charlotte Di Salvo, Former Editor & Chief Medical Writer
PharmaFEATURES
Subscribe
to get our
LATEST NEWS
Related Posts

Infectious Diseases & Vaccinology
Enduring Blockade: Five-Year Functional Antibody Persistence Against Emerging GII.4 and GII.17 Noroviruses
Natural infection with dominant GII noroviruses elicits long-lived functional antibodies, redefining immune durability in viral gastroenteritis.
Infectious Diseases & Vaccinology
Resistant Mycosis: Reimagining Antifungal Therapy Through Mechanistic Innovation and Molecular Disruption
Emerging antifungal strategies are redefining treatment by targeting fungal physiology through diversified, mechanism-driven approaches that overcome entrenched drug resistance.
Infectious Diseases & Vaccinology
Fungal Refractory States: Deciphering Pathobiology and Therapeutic Weaknesses in the Era of Rising Antifungal Resistance
Rising antifungal resistance reflects a multidimensional biological challenge that demands mechanistically innovative, host-integrated therapeutic strategies.

Infectious Diseases & Vaccinology
Epigenetic Parasite Vulnerabilities: Repurposing Histone Deacetylase Inhibitors for Complex Multispecies Therapeutics
Repurposed HDAC inhibitors target essential parasite epigenetic machinery, offering a powerful but complex frontier for next-generation antiparasitic therapy.
Read More Articles
Spatial Collapse: Pharmacologic Degradation of PDEδ to Disrupt Oncogenic KRAS Membrane Localization
PDEδ degradation disrupts KRAS membrane localization to collapse oncogenic signaling through spatial pharmacology rather than direct enzymatic inhibition.
Neumedics’ Integrated Innovation Model: Dr. Mark Nelson on Translating Drug Discovery into API Synthesis
Dr. Mark Nelson of Neumedics outlines how integrating medicinal chemistry with scalable API synthesis from the earliest design stages defines the next evolution of pharmaceutical development.
Zentalis Pharmaceuticals’ Clinical Strategy Architecture: Dr. Stalder on Data Foresight and Oncology Execution
Dr. Joseph Stalder of Zentalis Pharmaceuticals examines how predictive data integration and disciplined program governance are redefining the future of late-stage oncology development.
Exelixis Clinical Bioanalysis Leadership, Translational DMPK Craft, and the Kirkovsky Playbook
Senior Director Dr. Leo Kirkovsky brings a rare cross-modality perspective—spanning physical organic chemistry, clinical assay leadership, and ADC bioanalysis—to show how ADME mastery becomes the decision engine that turns complex drug systems into scalable oncology development programs.
Policy Ignition: How Institutional Experiments Become Durable Global Evidence for Pharmaceutical Access
Global pharmaceutical access improves when IP, payment, and real-world evidence systems are engineered as interoperable feedback loops rather than isolated reforms.







