In recent research, a groundbreaking concept has emerged, revealing a surprising commonality between cancers and neurological diseases. This concept, termed “Aberrant Cell Cycle Disease” (ACCD), highlights a shared mechanism driving the progression of both cancer and neurological disorders—namely, an abnormal re-entry into the cell cycle. At the core of ACCD is an interruption in the delicate balance of cell cycle regulation, leading to uncontrolled cell proliferation in cancer or neuronal cell death in neurological diseases. The abnormal cell cycle re-entry is characterized by either the activation of oncogenic kinases or inhibition of tumor suppressor pathways, mechanisms that, until recently, were thought to be mostly distinct across disease classes.
The ACCD framework reshapes the way researchers perceive these complex diseases by expanding the range of implicated cell cycle players. Traditionally, cyclins and cyclin-dependent kinases (CDKs) were the primary suspects. However, ACCD research now points to a wider array of oncogenic kinases—such as Src family kinase (SFK), Jun N-terminal kinase (JNK), and extracellular signal-regulated kinase (ERK)—as critical factors. Their roles transcend conventional boundaries, being pivotal not only in tumor proliferation but also in the degeneration of neurons.
The Aberrant Cell Cycle: A Common Pathway in Disease
Cancers and neurological diseases might seem to reside on opposite ends of the disease spectrum, but both exhibit a disrupted cell cycle. In cancer, this disruption translates into the cell’s inability to halt proliferation, leading to tumor growth. Environmental and genetic factors play a significant role in triggering the aberrant cell cycle in cancerous cells. On the other hand, neurons—being post-mitotic cells—are designed to avoid cell cycle re-entry once they reach maturity. This is to maintain a stable resting phase, known as the G0 phase. When exposed to certain stressors, however, mature neurons can be forced to re-enter the cell cycle abnormally. Since they lack the ability to complete mitosis, this leads to neuronal death, triggering or exacerbating neurodegenerative conditions.
The notion that ACCD drives both tumor growth and neurodegeneration suggests that interventions aimed at halting the cell cycle could yield therapeutic benefits. In cancer, blocking cell cycle progression holds the potential to hinder tumor growth. Conversely, in neurodegenerative diseases, preventing the aberrant re-entry of neurons into the cell cycle may provide neuroprotective effects, preserving neuronal function. This novel perspective aligns with growing efforts to repurpose kinase inhibitors—therapies that were initially designed to target cancers—to treat neurological diseases as well.
Therapeutic Directions: Blocking the Cell Cycle to Treat Disease
In targeting ACCD, two primary therapeutic strategies have emerged: inhibiting oncogenic kinases and elevating tumor suppressors. Each strategy carries potential for selectively modulating the cell cycle, thus offering potential benefits for both cancerous and neurological diseases. The focus has recently shifted to the first strategy, specifically the use of oncogenic kinase inhibitors. By 2022, the list of FDA-approved kinase inhibitors included 74 drugs, primarily approved for cancer treatment. Recent preclinical and clinical trials have begun to explore the efficacy of these inhibitors in the treatment of neurological disorders, ranging from Alzheimer’s disease (AD) to ischemic stroke (IS) and traumatic brain injury (TBI).
Although traditional drug development typically targets individual genes or proteins in a one-drug-on-one-target approach, this approach falls short in addressing the complexities of neurological disorders. These conditions are inherently heterogeneous, characterized by diverse underlying causes and variable genetic profiles. Furthermore, evidence suggests that a significant number of oncogenic kinases are elevated in neurological diseases, complicating treatment strategies. As a result, testing individual kinase inhibitors in preclinical models often yields limited success in clinical trials. Alternative approaches, like combinatorial therapies that target multiple pathways, are under consideration but present their own set of challenges, particularly in determining optimal drug combinations and managing potential interactions.
MicroRNAs: The Next Generation of Therapeutic Targets
In light of these challenges, microRNAs (miRNAs) have gained attention as a promising therapeutic alternative. Unlike traditional small molecule drugs that adhere to the one-drug-on-one-target model, miRNAs offer a broader scope of influence, functioning on a one-drug-on-numerous-target basis. MicroRNAs exert their regulatory effects by binding to the 3′ untranslated region (3′UTR) of hundreds of target genes, leading to post-translational suppression of these genes. This unique binding mechanism positions them as powerful modulators in both cancer and neurological disease, potentially acting as “master regulators” of gene expression.
Among the types of miRNAs, tumor suppressor miRNAs (TS-miRs) stand out for their ability to inhibit multiple oncogenic kinases. By elevating levels of TS-miRs, it becomes feasible to dampen oncogenic signals across a broad spectrum of kinases. This mechanism contrasts with that of traditional kinase inhibitors, which are often limited to a single kinase target. Theoretically, TS-miRs could achieve a more robust therapeutic effect, especially in conditions like neurodegenerative diseases where multiple pathways contribute to disease progression.
MicroRNA Dysregulation in Cancer
miRNA Dysregulation Patterns in Cancer Subtypes
Studies reveal that 1132 miRNAs display abnormal expression across a wide array of cancers, such as gastrointestinal, nervous system, and urological cancers. These dysregulated miRNAs are detected in samples like plasma, serum, blood, and tissue, making them valuable for broad-spectrum cancer diagnostics. Notably, specific miRNA signatures, unique to certain cancers, could serve as critical diagnostic biomarkers.
Mechanisms of miRNA Dysregulation in Cancer Progression
In cancer, miRNA dysregulation is often tied to genomic alterations at miRNA loci — through amplification, deletion, or translocation events. For instance, deletions at the miR-15a/16-1 cluster on chromosome 13q14 are associated with B-cell chronic lymphocytic leukemia. Lung cancers commonly show deletions in regions containing miR-143 and miR-145, leading to their downregulation, while miR-17–92 cluster amplifications in B-cell lymphoma stimulate oncogenic activity. These alterations disturb cell cycle regulation and apoptosis, fostering cancer cell growth and spread.
Diagnostic Potential of Circulating miRNAs in Early Cancer Detection
Circulating miRNAs found in blood and other bodily fluids are emerging as minimally invasive cancer biomarkers. For example, miR-29c is significantly downregulated in hepatocellular carcinoma, and miR-29a-3p correlates strongly with colorectal cancer cell proliferation and migration. In prostate cancer, the loss of miR-15 and miR-16, coupled with miR-21 overexpression, signifies tumor development and progression, underscoring the role of miRNAs as early diagnostic tools.
MicroRNA Dysregulation in Neurological Disorders
Acute Neurological Disorders and miRNA Biomarker Potential
In acute brain injuries — such as traumatic brain injury (TBI), ischemic stroke, and seizures — miRNAs exhibit notable changes in expression. miR-122 and miR-125b, for example, decrease following ischemic stroke and TBI, while others like miR-124 fluctuate post-injury. These miRNA expression shifts could act as early indicators for acute neurological damage, aiding diagnosis and potentially improving patient outcomes.
miRNA Roles in Epilepsy Pathophysiology
Epilepsy features distinct miRNA dysregulation patterns, with miRNAs impacting neuronal excitability, synaptic function, and inflammation. For instance, miR-128 and miR-124 tend to be downregulated, whereas miR-134 and miR-181a show upregulation in epilepsy patients, influencing neuronal apoptosis and dendritic spine density. These miRNA profiles provide insight into epilepsy mechanisms and could inform future therapeutic strategies.
miRNAs in Neurodegenerative Disorders
miRNAs as Biomarkers in Alzheimer’s Disease (AD)
In Alzheimer’s disease (AD), amyloid-beta (Aβ) plaque buildup and neuroinflammation are hallmark features. miR-124, for instance, downregulates beta-site amyloid precursor protein cleaving enzyme 1 (BACE1), reducing Aβ production and potentially slowing disease progression. Similarly, miR-146a mitigates astrocytic inflammation, suggesting a promising approach for AD treatment and neuroinflammation management.
Parkinson’s Disease (PD) and miRNA Therapeutics
In Parkinson’s disease (PD), miRNA dysregulation, particularly miR-7 and miR-153, which target SNCA (alpha-synuclein), significantly impacts dopaminergic neuron survival. miR-205 regulates LRRK2 expression, both essential to PD pathology. Using miRNA mimics or inhibitors to modulate these interactions presents a promising PD treatment approach, potentially improving neuroprotection and slowing disease progression.
Amyotrophic Lateral Sclerosis (ALS) and miRNA Dysregulation
Amyotrophic lateral sclerosis (ALS) is characterized by motor neuron degeneration. miR-338 and miR-143 are elevated in ALS patients and are associated with neuroinflammation and degeneration. miR-206, specific to skeletal muscle, is notably upregulated in ALS and could aid in muscle repair, potentially slowing disease progression and symptom onset.
Shared miRNA Dysregulation in Cancer and Neurological Disorders
Common miRNAs as Biomarkers Across Cancer and Neurological Diseases
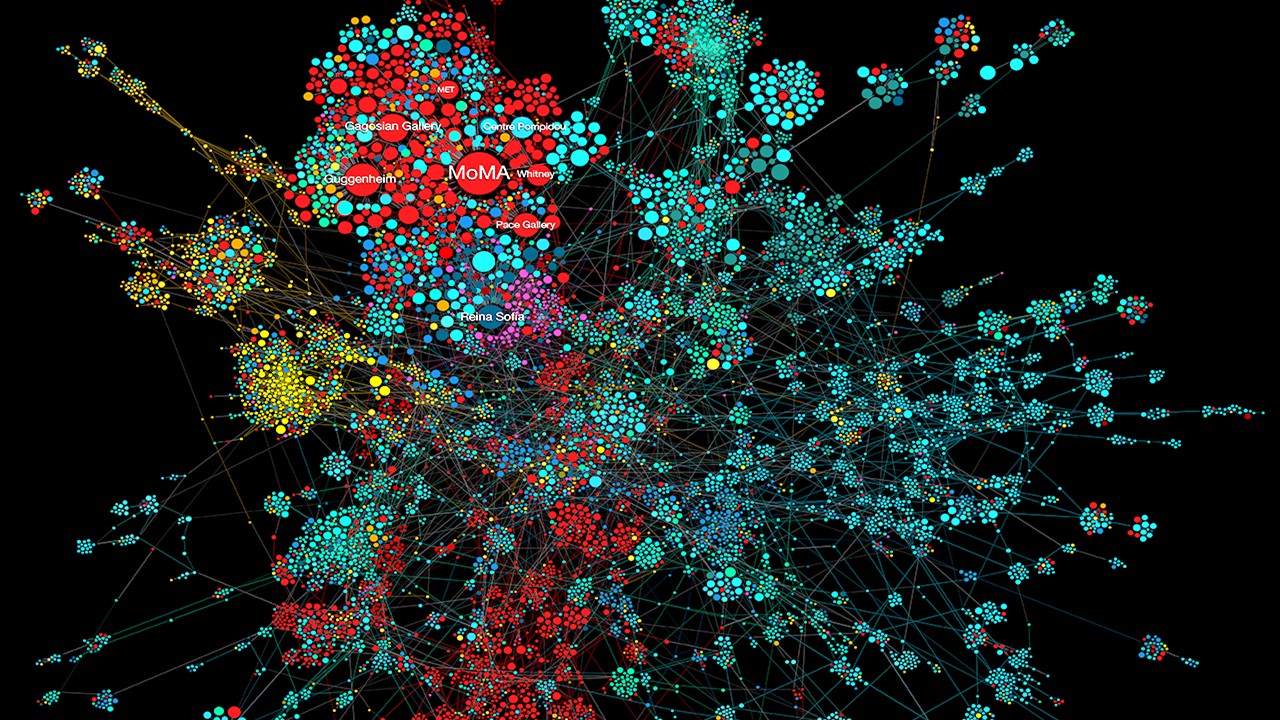
A closer look at miRNA dysregulation reveals overlap between cancer and neurological diseases, indicating common regulatory pathways. Thirty-one miRNAs, including miR-18a, miR-20a, and miR-181a, are consistently upregulated across both disease types, suggesting potential as universal biomarkers.
Tumor Suppressive miRNAs Downregulated in Both Disease Types
Among miRNAs, 17 tumor suppressors, like miR-28 and let-7i, display downregulation in both cancer and neurological disorders. These miRNAs govern cell cycle and apoptosis pathways, highlighting the potential for miRNA-based therapies that could benefit both cancer and neurodegenerative disease treatments.
Clinical Trials of miRNA-Based Drugs for Neurological Disorders
Despite substantial experimental evidence showing the efficacy of miRNA drugs for neurological disorders, only a limited number of miRNA-based drugs have progressed to clinical trials for these indications. Currently, three miRNA drugs have been tested in clinical trials targeting neurological diseases, highlighting the emerging role of miRNA therapies in addressing complex neurological conditions.
miRNA Therapy for Huntington’s Disease: AMT-130
One of the most recent U.S. clinical trials, aimed at halting the progression of Huntington’s disease (HD), involves the investigational drug AMT-130. This gene therapy employs an adeno-associated viral vector (AAV5) to deliver a synthetic miRNA (hsa-pre-miR-451a scaffold) specifically targeting the HTT gene responsible for HD pathology. By lowering HTT levels, AMT-130 aims to mitigate the neurodegenerative impact of HD (NCT04120493). A similar trial is underway in Europe (NCT05243017). miR-451a, the miRNA scaffold used in AMT-130, also functions as a tumor suppressor in several cancers, demonstrating its diverse therapeutic potential across diseases. Early models indicate that this approach successfully reduces HTT expression, showing promise for long-term HD management.
miRNA Therapeutics in ALS and Epilepsy
In amyotrophic lateral sclerosis (ALS), a clinical trial beginning in 2024 is set to examine the safety and efficacy of AMT-162, an AAV9-based gene therapy designed to deliver miRNA silencing the SOD1 gene in patients with ALS who have SOD1 mutations (NCT06100276). This Phase 1/2 study, projected to end in 2027, aims to reduce the neurotoxic effects of SOD1, providing a potential intervention for this progressive neurodegenerative disease.
For epilepsy, specifically unilateral refractory mesial temporal lobe epilepsy, a Phase 1/2b trial is underway to evaluate AMT-260. This gene therapy utilizes the AAV9 vector to deliver miRNA, targeting the GRIK2 gene, which is implicated in epilepsy pathology. The trial, which began in 2023, focuses on assessing the safety, tolerability, and efficacy of this approach (NCT06063850).
Challenges in the Development of miRNA Therapeutics
The development of miRNA-based therapies faces several key challenges
Targeted Delivery and Tissue Specificity. Ensuring that miRNAs reach the intended tissue without affecting non-target tissues remains a major hurdle. Delivery mechanisms must be refined to improve tissue specificity, thereby reducing off-target effects and minimizing toxicity. Delivery systems, such as lipid nanoparticles and polymer-based carriers, are under investigation for their potential to enhance cell membrane penetration and miRNA stability.
Crossing Cell Membranes. Due to their hydrophilic and negatively charged nature, miRNAs struggle to traverse cell membranes unaided. Modifications to miRNAs and novel carrier methods could improve their intracellular delivery, enhancing therapeutic efficacy.
Identifying Ideal miRNA Candidates. The heterogeneity of miRNA expression, influenced by conditions like hypoxia and inflammation, complicates the selection of the most suitable miRNAs for therapy. Advanced next-generation RNA sequencing technologies are being employed to pinpoint miRNA candidates with high therapeutic potential, reducing the impact of variable expression patterns.
Synthetic miRNA Design Tools. Tools like miR-Synth, a computational pipeline developed by Laganà et al., facilitate the design of synthetic miRNAs capable of targeting multiple genes across different binding sites. This multi-target approach holds promise for diseases involving complex dysregulation of multiple genes, potentially allowing a single miRNA to counteract several pathological pathways simultaneously.
Looking Ahead
miRNA therapeutics are in the early stages of development but show significant promise for the treatment of neurological disorders. Certain tumor-suppressive miRNAs (TS-miRNAs), initially identified in cancer research, are now being explored for neurological applications due to their capacity to modulate multiple disease-relevant genes concurrently. By targeting multiple oncogenic pathways and mitigating neuronal damage, TS-miRNAs represent a promising therapeutic approach for complex neurodegenerative conditions.
Advances in miRNA research and an expanded understanding of miRNA function have spurred growing interest in their application within personalized medicine. miRNAs’ ability to regulate gene expression, serve as accessible biomarkers, and influence multiple targets underscores their potential as therapeutics. As technological advances continue to address delivery challenges, tissue targeting, and miRNA selection, miRNA drugs, including TS-miRNAs for neurological disorders, are likely to see expanded use in clinical settings. Ultimately, overcoming these barriers could lead to regulatory approval and more effective treatments for conditions with few current options.
Study DOI: https://doi.org/10.3390/ph17040426
Engr. Dex Marco Tiu Guibelondo, B.Sc. Pharm, R.Ph., B.Sc. CpE
Editor-in-Chief, PharmaFEATURES
Register your interest [here] at Proventa International’s Clinical Operations and Clinical Trials Supply Chain Strategy Meeting this 14th of November 2024 at Le Meridien Boston Cambridge, Massachusetts, USA to engage with thought leaders and like-minded peers on the latest developments in the clinical space and regulatory affairs.

Subscribe
to get our
LATEST NEWS
Related Posts

Immunology & Oncology
The Silent Guardian: How GAS1 Shapes the Landscape of Metastatic Melanoma
GAS1’s discovery represents a beacon of hope in the fight against metastatic disease.
Immunology & Oncology
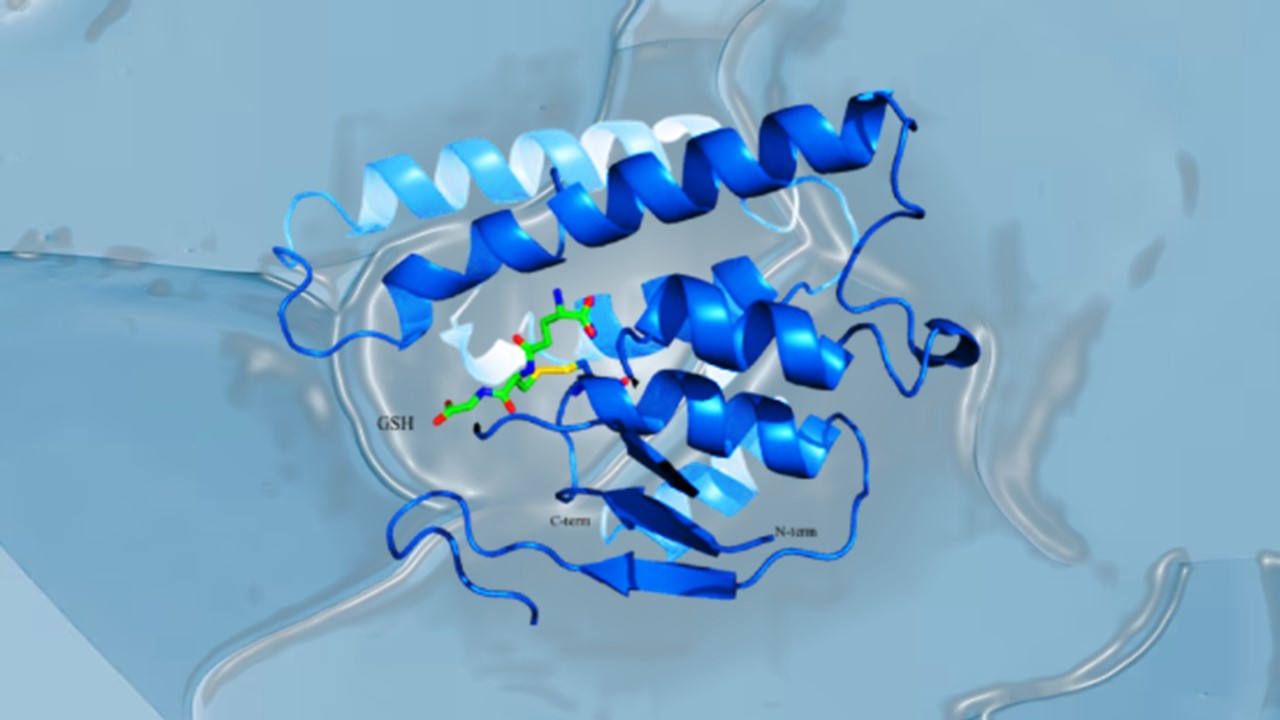
Resistance Mechanisms Unveiled: The Role of Glutathione S-Transferase in Cancer Therapy Failures
Understanding this dual role of GSTs as both protectors and accomplices to malignancies is central to tackling drug resistance.
Read More Articles
Myosin’s Molecular Toggle: How Dimerization of the Globular Tail Domain Controls the Motor Function of Myo5a
Myo5a exists in either an inhibited, triangulated rest or an extended, motile activation, each conformation dictated by the interplay between the GTD and its surroundings.
Designing Better Sugar Stoppers: Engineering Selective α-Glucosidase Inhibitors via Fragment-Based Dynamic Chemistry
One of the most pressing challenges in anti-diabetic therapy is reducing the unpleasant and often debilitating gastrointestinal side effects that accompany α-amylase inhibition.